3 January 2021
31958
0
4.1 out of 5
Some diseases of the spine, vascular disorders and even endocrine pathologies can provoke the occurrence of such an unpleasant and very detrimental condition as cervical myelopathy. It is accompanied by disturbances in sensitivity and mobility, and can also lead to serious complications. Therefore, it is important to diagnose it in the early stages of development, establish the cause of its occurrence and effectively influence it in order to avoid worsening the condition.
Causes of myelopathy
Myelopathy is a disorder of the spinal cord, most often due to one of several reasons:
- Compression (prolapsed disc herniation, bone growth, displaced vertebra, vertebral fragment);
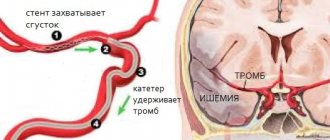
- Poor circulation of the spinal cord (blockage, narrowing or congenital anomaly of the arteries of the spinal cord, spinal stroke);
- Previous trauma (bruise, spinal fracture, surgery);
- Inflammation of the vertebrae or spinal cord (spinal arachnoiditis, myelitis).
- Complication after spinal puncture.
Spinal cord compression at the level of the 5th and 6th cervical vertebrae
Etiology and pathogenesis of myelopathy
In the overwhelming majority of cases of myelopathy, its location is the cervical spine, which occurs as a result of the development of osteochondrosis or spondylosis. In the latter case, we are talking about vertebrogenic cervical myelopathy.
Myelopathy can also develop due to diseases such as congenital spinal stenosis, craniovertebral anomaly, damage to spinal tissue as a result of injuries and deformations, cirrhosis of the liver, deficiency of vitamins E and group B, borreliosis, rheumatoid arthritis, paraneoplastic syndrome. There is myelopathy that develops as a result of therapeutic measures, which can be chemical and radiation therapy, epidural anesthesia.
There are other types of myelopathy, the causes of which can be atherosclerosis, various inflammations, received doses of radiation, osteoporosis, diabetes, etc.
Among the causes of the vertebrogenic form are herniated intervertebral discs, congenital stenosis of the spinal canal and osteochondrosis. Myelopathy of this type develops when the spine regularly experiences loads falling on its upper zones, where the pathology is localized. The acute version of myelopathy is the result of injuries that patients usually receive in car accidents due to whiplash. This is a special movement of the head and neck when the car suddenly stops, for example, when colliding with an object. Typically, this injury occurs to an unbelted driver or front seat passenger. In this case, the spinal cord is damaged as a result of displacement.
Symptoms of myelopathy
The spinal cord is the main “cable” of the nervous system, connecting the brain to the body. If this cable malfunctions, the connection between the brain and the body is disrupted, which can lead to the following symptoms:
- Decreased muscle strength in the arms and/or legs (paralysis, paresis) below the site of spinal cord injury. Does not always coincide with sensory impairment.
- Loss of sensation below the site of spinal cord injury. It is possible to decrease or increase only one type of sensitivity (pain, tactile, temperature, muscle-articular sensation) or all types of sensitivity.
- Bladder and bowel dysfunction (pelvic disorders). Incontinence or difficulty emptying the bladder and bowels may occur.
- Tension in the muscles of the legs and sometimes the arms (spasticity). This is due to the brain's control over the spinal cord being switched off. Nerve cells in the spinal cord autonomously tense the muscles of the limbs. The legs are characterized by forced flexion of the knee and plantar flexion of the foot. For the arms – forced flexion at the elbow joint and fingers.
Classification of myelopathy according to ICD
Rational division of pathology forms based on the International Classification of Diseases 10th revision by etiology:
- Necrotic;
- Idiopathic;
- Edema;
- Thrombophlebotic;
- Neurogenic;
- Non-embolic;
- Embolic.
The choice of treatment is based on the neurological classification of forms:
- Infectious;
- Carcinomatous;
- Post-traumatic;
- Ischemic;
- Spondylogenic;
- Metabolic;
- Toxic;
- Demyelinating;
- Radiation.
With all varieties, loss of sensitivity in the limbs, spasm of the leg muscles, and weakness develop.
Loss of sensitivity forms paresis, paralysis, weakening of vibration and pain activity.
Examination and diagnosis
MRI clearly visualizes the spinal cord, brain, intervertebral discs, and spinal cord tumors. Well distinguishes areas of spinal stroke.
Computed X-ray tomography (CT) clearly visualizes the bones of the spine. CT angiography is a method for studying blood vessels (including the spinal cord) with preliminary intravenous administration of a contrast agent.
Electromyography (EMG, ENMG, somatosensory evoked potentials, magnetic stimulation study) allows you to evaluate the conduction of electrical excitation along the spinal cord and peripheral nerves.
blood tests mainly to diagnose infectious, metabolic, and autoimmune diseases of the spinal cord. The analysis also provides the necessary information about circulatory disorders of the spinal cord associated with increased blood viscosity.
Tests and diagnostics
The diagnosis of myelopathies is based on manual examination, testing sensitivity/reflexes at certain points and instrumental research methods, including:
- Survey/targeted radiography of the spinal column in several projections.
- Electroneurogram.
- Computed tomography.
- Magnetic resonance imaging.
- Contrast research methods ( discography , pneumomyelography , myelography , venospondylography , epidurography ).
If necessary (suspicion of heavy metal poisoning, vitamin B12 ), laboratory tests are prescribed. If infection is suspected, a spinal tap .
Prognosis for myelopathy
Basically, the prognosis is determined by how much spinal cord substance is preserved or lost. Everything becomes clear after the action of the damaging factor on the spinal cord ceases (cessation of compression, restoration of blood flow, etc.). The sooner the damaging factor stops, the better the prognosis. That is why we often insist on a full examination with all the details clarified, and, in some cases, on a consultation with a neurosurgeon. Presumable conclusions can be drawn from the results of MRI and electroneuromyography.
Forecast
In 60% of patients with myelopathy, complete/partial regression of neurological symptoms is observed. In 20% of patients, the condition does not change significantly and remains stable, but functional adaptation to the resulting neurological defect is noted, and in 10% of patients there is progression with a gradual worsening of symptoms.
With chronic compression myelopathies, irreversible destructive changes increase in muscle tissue, nerves and directly in the spinal cord - muscle atrophy , proliferation of connective tissue. Therefore, even in cases where the compressive factor is eliminated, it is impossible to restore full sensory/motor functions, and the resulting neurological disorders are irreversible, which causes disability for the patient.
Treatment at the Echinacea Clinic
The sooner treatment for myelopathy is started, the better the prognosis. Our clinic provides non-surgical treatment of myelopathy, including the consequences of previous operations.
The specialists of our center will perform the most complete examination and, based on its results, will draw up an individual treatment and rehabilitation program. The treatment program will not require regular visits to the clinic - you will be able to follow most of the recommendations at home with periodic monitoring by your doctor.
If surgical intervention is necessary, we will help you seek the help and experience of a serious specialist in the field of low-traumatic endoscopic neurosurgery of the spine.
When going to our clinic, be sure to take all the medical documents available to you: pictures, disks with tomograms, tests, maps, ultrasound reports, ECG and others, even, at first glance, not related to spinal cord problems.
You can contact Dr. E.A. Engels or the head of the clinic K.A. Shlyapnikov.
List of sources
- Agasarov L., Petrov A. Neurovertebrogenic syndromes // MG. - 2003. - No. 24. - P. 8-9.
- Kamalov I.I. Degenerative-dystrophic changes in the spine / I.I. Kamalov // Vertebroneurology. - 1995. - No. 1-2. — P. 24-31.
- 3abbarova A.T. Centromedullary cervical myelopathy: clinical significance of the spondylogenic factor and the “tight cistern magna” syndrome / A.T. Zabbarova, E.I. Bogdanov // Nevr. messenger Journal named after V.M. Bekhtereva - 2011. -No. 1. - P. 87-90.
- Gorbunov F. E., Penionzhkevich D. Yu. Cervical myelopathy and its treatment by physical factors / To help the practitioner, 2001-N 6, p. 46-50.
- Nekrasov A.K., Nekrasov M.A., Igoshin Yu.A., Seregin A.B., Shevchuk V.V., Gogolev A.Yu. Acute discogenic lumbar myelopathy: clinical characteristics and course options" Bulletin of the Ivanovo Medical Academy T. 12, N° 3-4, 2007
Myelopathy syndrome with lower paraparesis
Lower myelopathy against the background of dorsopathy in the lumbosacral spine can be associated with cauda equina syndrome. The signs of these two pathologies are similar. But the essence of the diseases is slightly different. In myelopathy syndrome, compression occurs in the spinal canal. With cauda equina syndrome, compression occurs externally as the plexus of radicular nerves exits in the coccyx area. Therefore, different treatments are used.
Myelopathy with lower paraparesis is a reason for immediate contact with a neurologist or vertebrologist. Immediately after differential diagnosis, treatment must begin. With prolonged compression of the spinal cord, a person may become paralyzed in the lower extremities. It will be extremely difficult to subsequently restore the ability to move independently.
Acute type
All three forms of myelopathy differ in the speed of development of symptoms, as well as the degree of pronounced functions that were once lost. The most severe type of spinal cord compression is considered to be the most severe. In this case, there is a loss of motor and sensory functions of the body, and a flaccid type of paralysis may develop. Usually sensitivity disappears in the lower extremities. In addition, the functionality of the bladder or rectum is impaired. This condition is called spinal shock. After a certain time, a flaccid type of paralysis may develop, which passes into the spastic stage with the manifestation of its characteristic reflexes or convulsions. The joints may become stiff and contracture develops.
Chronic form
Let's take a closer look at compression in the cervical spine. Its chronic form usually begins with dull pain in the neck muscles or the back of the head. It can also appear in the upper chest, upper and lower extremities. Around these parts of the body, sensory dysfunction occurs, which manifests itself in the form of goosebumps or numbness. In the future, muscle weakness in the limbs may occur. In addition, atrophy and even muscle twitching may occur. If the compression site is located in the first or second segment, the characteristics of the affected facial nerve may appear, which is reflected in sensory disturbances on the face. It is also possible that symptoms such as unsteady gait and trembling hands may occur.
Another symptom inherent in compression myelopathy is squeezing in the chest. It should be said that compression in these parts of the spinal cord is extremely rare. They are most often characterized by increased weakness and decreased tone in the lower extremities. Sensation in the chest, abdomen or back may also be impaired.
A version of this disease in the lumbar region manifests itself as pain in the muscles of the thighs, buttocks, and lower legs. In addition to the characteristic pain, there is also a corresponding change in sensitivity in these same areas. As the duration of action of the traumatic factor itself increases, the patient feels noticeable weakness in the muscle fibers, decreased muscle tone, and atrophy (reduction in muscle volume). Over time, a flaccid type of peripheral paresis may develop in one leg (or both).