What causes it to appear
Impaired walking function is associated with pathologies of the central nervous system (CNS). The cerebellum is responsible for coordination. When it is damaged, incoordination of motor skills and movement appears, and it is difficult to maintain balance.
Causes of poor coordination when walking:
- brain tumors;
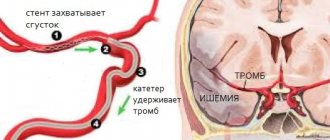
- pathology of cerebral arteries;
- endocrine diseases, including hypothyroidism;
- congenital malformations of the central nervous system;
- injuries;
- taking sleeping pills, anticonvulsants and other psychotropic drugs in large quantities;
- chemical poisoning;
- genetic abnormalities;
- vitamin B12 deficiency;
- multiple sclerosis.
Depending on the etiology, treatment for walking disorders is selected.
Treatment
Treatment of deterioration in coordination associated with stroke or other central nervous system pathologies is carried out only in a hospital setting. Treatment for vestibular ataxia can be carried out on an outpatient basis. The most common factor in the deterioration of coordination in vestibular ataxia is inflammatory diseases of the inner ear. Treatment is aimed at sanitizing the source of infection.
Complex therapy with antimicrobial and anti-inflammatory drugs (Otinum, Otipax, Sofradex) is used. When infection is excluded, treatment is carried out with nootropic (Piracetam, Phenibut), anticonvulsant (Carbamazepine, Carbalepsin) drugs and antihypoxants (Mildronate, Actovegin), and vitamin complexes are prescribed. Physiotherapy is required, including physical therapy and massage. Daily exercises combined with drug therapy make it possible to restore a complex coordination system.
The reception is conducted by specialists
Kinds
Manifestations of the disease depend on its type. They are divided by etiological nature and symptoms.
Types of ataxia:
- Sensitive - formed against the background of polyneuropathy, that is, multiple damage to nerve fibers. Characteristic features: a high rise of the leg and a sharp lowering of the leg, which is called a “stamping gait.” It is difficult to maintain balance with your eyes closed. People walk carefully, keeping every step under visual control.
- Vestibular – associated with nausea, vomiting, dizziness. Symptoms become more pronounced due to turning the head and changing body position.
- Psychogenic - a hysterical type of ataxia, in which the gait is very confused, while there is no organic brain damage.
- Cerebellar - in the dark and with eyes closed there is no coordination of movements, but in the presence of vision it is normal. The person has a slow reaction, slurred speech, and incomprehensible handwriting.
- Hereditary - includes the classic symptoms of ataxia with features characteristic of a specific pathology.
- Cortical - formed due to pathological processes in the anterior lobe of the cerebrum. It manifests itself as unsteady walking, difficulty at the beginning of movement and when turning (“legs get tangled”). Often accompanied by hallucinations, problems with the grasping reflex, and inability to sit without support.
Other symptoms of impaired walking function include a wide gait, in which a person sways strongly in different directions, difficulties in performing small movements, and self-care in everyday life. Vomiting, nausea, pain in the head, and speech impairment may occur.
Ataxia
The emergence of sensitive ataxia
caused by damage to the posterior columns (bundles of Gaulle and Burdach), less commonly the posterior nerves, peripheral nodes, parietal cortex, thalamus (funicular myelosis, tabes dorsalis, tumors, vascular disorders). It may manifest itself in all limbs, or in one leg or arm. The most significant phenomena are sensory ataxia, which occurs as a result of a disorder of joint-muscular sensation in the lower extremities. The patient is unsteady, when walking he bends his legs excessively at the hip and knee joints, and steps too hard on the floor (stamping gait). Often there is a feeling of walking on cotton wool or carpet. Patients try to compensate for the disorder of motor functions with the help of vision - when walking, they constantly look at their feet. This can significantly reduce the manifestations of ataxia, and closing the eyes, on the contrary, aggravates them. Severe lesions of the posterior columns practically make it impossible to stand and walk.
Cerebellar ataxia
- a consequence of damage to the cerebellar vermis, its hemispheres and peduncles. In the Romberg position and when walking, the patient falls (even to the point of falling) towards the affected cerebellar hemisphere. If the cerebellar vermis is damaged, it is possible to fall to any side or backward. The patient staggers when walking and places his legs wide. The flanking gait is severely impaired. Movements are sweeping, slow and awkward (more so on the part of the affected cerebellar hemisphere). Coordination disorder is almost invariable during visual control (open and closed eyes). There is a disturbance in speech - it slows down, becomes stretched, jerky, and often chanted. Handwriting becomes splayed, uneven, and macrography is observed. There may be a decrease in muscle tone (more on the affected side), as well as a violation of tendon reflexes. Cerebellar ataxia can be a symptom of encephalitis of various etiologies, multiple sclerosis, malignant neoplasm, vascular lesion in the brainstem or cerebellum.
Vestibular ataxia
develops when one of the sections of the vestibular apparatus is damaged - the labyrinth, vestibular nerve, nuclei in the brain stem and the cortical center in the temporal lobe of the brain. The main symptom of vestibular ataxia is systemic dizziness (it seems to the patient that all objects around him are moving in the same direction), dizziness intensifies when turning the head. In this regard, the patient staggers randomly or falls, and makes head movements with noticeable caution. In addition, vestibular ataxia is characterized by nausea, vomiting and horizontal nystagmus. Vestibular ataxia is observed in brainstem encephalitis, ear diseases, tumors of the fourth ventricle of the brain, as well as in Meniere's syndrome.
Development of cortical ataxia
(frontal) is caused by damage to the frontal lobe of the brain caused by dysfunction of the fronto-pontine-cerebellar system. In frontal ataxia, the leg contralateral to the affected cerebellar hemisphere is most affected. When walking, there is instability (more so when turning), tilting or leaning to the side ipsilateral to the affected hemisphere. With severe lesions of the frontal lobe, patients cannot walk or stand at all. Vision control has no effect on the severity of walking disorders. Cortical ataxia is also characterized by other symptoms characteristic of damage to the frontal lobe - the grasping reflex, mental changes, and impaired sense of smell. The symptom complex of frontal ataxia is very similar to cerebellar ataxia. The main difference between cerebellar lesions is evidence of hypotonia in the ataxic limb. The causes of frontal ataxia are abscesses, tumors, and cerebrovascular accidents.
Hereditary cerebellar Pierre-Marie ataxia
- a hereditary disease of a chronic progressive nature. It is transmitted in an autosomal dominant manner. Its main manifestation is cerebellar ataxia. The pathogen has high penetrance, skipping generations is very rare. A characteristic pathological sign of Pierre-Marie ataxia is cerebellar hypoplasia, less often - atrophy of the inferior olives, the cerebral bridge (pons). Often these signs are combined with combined degeneration of the spinal systems (the clinical picture resembles Friedreich's spinocerebellar ataxia).
The average age of onset is 35 years when gait disturbance appears. Subsequently, it is accompanied by disturbances in facial expressions, speech and ataxia in the hands. Static ataxia, adiadochokinesis, and dysmetria are observed. Tendon reflexes are increased (to pathological reflexes). Involuntary muscle twitches are possible. Strength in the muscles of the limbs is reduced. Progressive oculomotor disorders are observed - paresis of the abducens nerve, ptosis, convergence insufficiency, less often - Argyll Robertson's sign, optic nerve atrophy, decreased visual acuity, narrowing of the visual fields. Mental disorders manifest themselves in the form of depression and decreased intelligence.
Familial Friedreich's ataxia
- a hereditary disease of a chronic progressive nature. It is transmitted in an autosomal dominant manner. Its main manifestation is mixed sensory-cerebellar ataxia, resulting from combined damage to the spinal systems. Consanguineous marriages are very common among patients' parents. A characteristic pathological sign of Friedreich's ataxia is increasing degeneration of the lateral and posterior columns of the spinal cord (up to the medulla oblongata). Gaulle's bundles are most affected. In addition, the cells of Clark's columns are affected, and along with them the posterior spinocerebellar tract.
The main symptom of Friedreich's ataxia is ataxia, which is expressed in an uncertain, clumsy gait. The patient walks in a sweeping manner, deviating from the center to the sides and placing his feet wide. Charcot designated this gait as a tabetic-cerebellar gait. As the disease progresses, incoordination spreads to the arms, chest muscles and face. Facial expressions change, speech becomes slow and jerky. Tendon and periosteal reflexes are significantly reduced or absent (primarily on the legs, later on the upper extremities). In most cases, hearing is reduced.
With the development of Friedreich's ataxia, extraneural disorders appear - cardiac lesions and skeletal changes. The ECG shows deformation of the atrial wave, rhythm disturbance. There is paroxysmal pain in the heart, tachycardia, shortness of breath (as a result of physical stress). Skeletal changes are expressed in a characteristic change in the shape of the foot - a tendency to frequent dislocations of the joints, an increase in the arch and extension of the fingers, as well as kyphoscoliosis. Among the endocrine disorders that accompany Friedreich's ataxia are diabetes, hypogonadism, and infantilism.
Ataxia-telangiectasia
(Louis-Bar syndrome) is a hereditary disease (phakomatoses group), transmitted in an autosomal recessive manner. Very often accompanied by dysgammaglobulinemia and hypoplasia of the thymus gland. The development of the disease begins in early childhood, when the first ataxic disorders appear. In the future, ataxia progresses and by the age of 10, walking is almost impossible. Louis-Bar syndrome is often accompanied by extrapyramidal symptoms (hyperkinesis of the myoclonic and athetoid type, hypokinesia), mental retardation, and damage to the cranial nerves. There is a tendency to repeated infections (rhinitis, sinusitis, bronchitis, pneumonia), which is primarily due to the insufficiency of the body’s immunological reactions. Due to the deficiency of T-dependent lymphocytes and class A immunoglobulins, there is a high risk of malignant neoplasms.
Which coordination exercises to choose?
Any physical exercise, from simple morning exercises to complex acrobatic elements, improves your ability to control your body. You can take up yoga or tai chi, learn to juggle, or go to the gym and do strength exercises - all of which will improve your coordination.
If you want to improve your strength in a short time, try complex coordination movements: they require maximum concentration, involve many muscle groups at once and allow you to increase the complexity due to the speed of execution.
We offer several options for such exercises:
- Strength exercises with your body weight.
- Different types of jumping rope.
- Exercises on the coordination ladder.
- Movements with a tennis ball.
Choose what you like best, or try everything.
How are variants of gait disorders identified?
According to the method of manifestation of certain signs, the following types can be roughly distinguished:
- Atactic, or shaky. Occurs when the cerebellum or thalamus is damaged. The patient spreads his legs wide apart and walks, constantly staggering, regularly losing his balance.
- Stamping. Appears as a result of damage to the conducting fibers of the nervous system. When walking, the patient lowers his leg onto the entire foot at once, as if imprinting each step.
- Shuffling. This type of walking is characteristic of the elderly, and it also develops against the background of a number of neurological pathologies and general weakness. It is characterized by a decrease in the length of the step, in which the foot almost does not come off the floor, as if dragging.
- Cock (peroneal, steppage). Occurs when there are problems with the peroneal nerve, against the background of multiple sclerosis, poliomyelitis and some other pathologies. When lifting the leg, the foot hangs down, and the patient has to bend the knee strongly so as not to catch the dangling toe on the ground.
- Duck gait (Duchenne lameness). While walking, the patient seems to shift from one foot to another, resembling a duck. Such an unsteady gait occurs in people suffering from paresis or who have received a mechanical injury to the abductor group of the thigh muscles.
- Paretic. Develops as a result of muscle paresis of the lower extremities. Specific features depend on which muscle group is involved in the pathological process.
- Hemiparetic gait. Accompanies hemiparesis of any nature: strokes, birth injuries, abscesses and brain tumors. When moving, the patient's arm is pressed to the body, and the diseased leg is straightened and describes a semicircle as it moves, while the body deviates each time towards the healthy half of the body.
- Hypokinetic. Manifested by stiffness of movement. Develops in people suffering from Parkinson's disease or occurs against the background of hydrocephalus.
- Hyperkinetic. Characterized by chaotic sudden movements. It occurs with chorea, foot dystonia and hyperkinesia.
- Iatrogenic. Develops as a result of alcohol intoxication or taking certain medications. Patients have the feeling that their legs do not obey them when walking.
- Paraspastic. It is typical for people suffering from hypertension, and also occurs in patients with cerebral palsy, severe or critical deficiency of B vitamins and myelopathy.
- Idiopathic senile. Appears in old age and is associated with degenerative-dystrophic changes in the musculoskeletal system.
- Freezing dysbasia (freezing when walking) and propulsion (acceleration while walking resulting from a small involuntary push). Appear in patients suffering from Parkinson's disease. Sometimes freezing appears after multifocal strokes or simply in older people without signs of neurological pathologies.
- Skater pose. When walking, a person bends his body low and makes wide, sweeping movements. Such instability occurs with orthostatic hypotension.
Coordination
Coordination
- the process of coordinating the work of muscles necessary for the successful performance of a motor function. With the development of a motor skill, the coordination of movements changes, including the development of the inertia of moving organs. At first, control occurs through active static fixation of these organs, then through short-term physical impulses directed at a certain moment to the desired muscle. At the final stages of coordination development, inertial movements are used. In an already established dynamically stable movement, balancing of all inertial movements occurs automatically, without producing additional correction impulses.
Old age
Often, older people (over 60 years old) experience swaying, as well as “floaters” before the eyes.
It is also common to experience tinnitus and dizziness when walking. Headaches appear sharply, and sometimes even fainting occurs. As a rule, all these symptoms are ignored and blamed on age. In some cases, this may indicate problems with the body, so you should consult a doctor. This way you can ensure your usual full life.
One of the reasons is a malfunction of the cardiovascular system of the brain. Atherosclerosis appears (as mentioned above, a disease of the second category).
With age, the functioning of the vestibular apparatus is impaired.
Gait disturbance may also be due to heart disease. For example, ischemia can reduce blood circulation in the area of the ear where the organ responsible for balance is located. Also, insufficient blood circulation leads to uncertain movements. Other diseases also have a detrimental effect (arrhythmia, hypertension).
It has a great influence on gait and blood viscosity, because it supplies oxygen to the organs. How quickly it reaches the desired place, including the cerebellum, depends on its speed.
Injuries and diseases of the spine also make it difficult to transmit signals. Therefore, movement disorders are possible. Elderly people are often susceptible to sleep disorders, which leads to diseases of the third category.
The most common occurrence of maladaptation is observed. The person feels extremely insecure, there is a feeling that no one needs him, inexplicable fears and anxiety. As a result, he may skid when walking, become dizzy, have dark vision, and his condition worsens every day. For treatment, you must definitely contact professionals and it is better not to delay, because the consequences can be disastrous.
Based on all of the above, we can conclude that many factors can lead to an unsteady gait and they should not be ignored.
If the cause is eliminated, the consequences will also be eliminated. Life will be familiar, fulfilling and healthy. Therefore, it does not matter how old a person is, treatment is necessary regardless of age.
What can be done for an elderly person with unsteady gait
Since unsteady gait increases the risk of falls, it is important to secure the elderly person's home:
- Remove all items from walkways (shoes, furnishings, extension cords, etc.).
- The corridors should be well lit (especially the path to the bathroom, toilet and kitchen).
- Place non-slip mats on the floor of the bathtub as well as at the exit of the bathtub.
- Buy comfortable house shoes with non-slip soles.
- You can keep a flashlight by your bed and use it if you need to get up at night.
According to doctors' recommendations, an elderly person needs:
- wear leg braces and orthoses;
- use a cane or walker for additional support and balance.
When to see a doctor
If your gait changes, you will need to consult a neurologist, traumatologist, orthopedist, ENT specialist or other specialist.
You should immediately seek medical help if your gait changes as a result of a fall or along with other symptoms:
- speech problems;
- labored breathing;
- dizziness;
- facial asymmetry;
- involuntary urination;
- severe throbbing headache;
- sudden numbness in one or more parts of the body.
You also need to urgently consult a doctor if problems with gait in an elderly person occur suddenly.