Our clinic specializes in neurology; we diagnose and treat various organ dysfunctions and movement disorders. We focus our main efforts on finding and treating the cause of the disorder in order to offer you targeted treatment .
- Dysfunction of the pelvic organs in diseases of the nervous system
- Paralysis, paresis, hemiparesis, paraparesis, monoparesis
- Muscle spasticity. Muscle tension
- Leg cramps, toe cramps
- Treatment of vision, hearing, smell disorders
In the labyrinth of terms
The scientific name of this pathology is paraparalysis (otherwise known as paraplegia). It’s very easy to remember: a pair of arms, a pair of legs (because this problem can also affect the lower extremities).
Paralysis (or plegia) is a complete loss of the ability to move (and not only in the limbs).
Unlike paraparalysis, paraparesis is a more “gentle” variant of the manifestation of pathology in the extremities, “sent from above” from the brain to both sides of the body at once.
Here, only the arms or only the legs are “beaten off” and therefore do not work. The movements in them are so weakened that they cannot perform the work intended for them, but there is sensitivity, so the limbs are only half deprived of life.
In other words, paresis is almost paralysis, but not complete: movements, sharply limited in volume and strength, are possible, but they are uncontrollable by the owner of the body.
For final clarity with strength and sensitivity in the limbs, it is worth remembering the ancient languages:
- mono
paresis or monoplegia - a destructive process in one limb; - pair
paresis or paraplegia - the same in two identical limbs (upper or lower); - hemiparesis
or hemiplegia - the development of a process in one half of the body; - tetra
paresis or tetraplegia is a pathology of all four (both upper and lower, both right and left) limbs.
Monoparesis of the lower extremities
Lower monoparesis is diagnosed much more often than upper monoparesis. This is due to the fact that the lumbosacral spine is subject to significantly greater shock absorption and physical load than the cervical spine. Monoparesis of the lower limb may be a consequence of damage to brain structures - this possibility should not be excluded during the initial diagnosis of the patient’s condition. After all, high-quality and comprehensive medical care can be provided to a person only in the first 3 hours after a cerebrovascular accident occurs.
Left-sided lower monoparesis is a lesion of the muscular system on the left leg. Left-sided monoparesis can develop against the background of osteochondrosis, its complications and tunnel syndromes.
Right lower monoparesis is a weakening of muscle strength in the right leg. Often, monoparesis of the right leg is a complication of deforming osteoarthritis of the hip joint, which provokes the development of piriformis syndrome and compression of the sciatic nerve. Monoparesis of the left lower limb can also be caused by compression of the sciatic nerve, but this happens less frequently.
Leg monoparesis can be partial or complete. In the first case, certain muscles are affected, for example, the calf muscles. There is difficulty in adducting and abducting the foot while walking. Monoparesis of the left leg can be combined with degeneration of cartilage tissue in the ankle and knee joints. The load on them increases and this leads to thinning of the cartilage tissue.
“Plege” means blow - the reasons are available
For what reason does a decline in muscle strength occur, accompanied by a complete absence of voluntary movements in both arms (or legs) - paraplegia?
For this condition to develop, one of the motor pathways of the nervous system must be affected, each of which bears the name of the researcher who discovered it.
Depending on the cause that caused it and the speed of onset of the condition, paraplegia can be:
- Acute
, which can develop as a result of an electrolyte imbalance such as severe hypokalemia, or due to a stroke, both of the brain and spinal cord, or as a result of compression of the spinal cord caused by a vertebral fracture (compression myelitis). - A subacute
variant of development is a possible result of a “drama” that plays out in the brain or spinal cord under the influence of a bacterial infection (myelitis and meningomyelitis of an infectious nature, including polio), or a liquorodynamic (like a hydraulic) shock, or a consequence of ischemia of some kind. either part of the nervous system, or the cause may be a congenital deformity of the spine. - A sluggish form
of the disorder can manifest itself as a parasitic infection of the central nervous system, as well as a tumor that has arisen in it, or a herniation of the spinal cord, as well as spondyloarthrosis. Or there may be no obvious cause at all - an idiopathic variant of flaccid paraplegia.
In the case of damage to the nervous system of organic origin, paraplegia is called organic, in the case of mental genesis - psychogenic, mainly - hysterical.
The basis of organic paraplegia, most often spastic, is damage to the nervous system (both peripheral and central) due to atherosclerosis, arteritis, which lead to the formation of foci of softening of the brain of a bilateral nature, while psychogenic paraplegia is a predominantly sluggish course of the disorder.
Paraplegia occurs as a consequence of amyotrophic lateral sclerosis or multiple sclerosis, and also occurs with syringomyelia.
Why is “water hammer” the reason for the development of paraplegia?
With this pathology (due to confusion in the control of electrical currents), the normal flow of cerebrospinal fluid, the main fluid connecting all levels of the nervous system, is always disrupted.
So “water breaks the mill” is a popular wisdom; it cannot be said more precisely.
Causes
The main reasons for the development of paresis include:
- birth injuries (most often the occurrence of distal paresis is associated with birth injury in the brachial plexus);
- hemorrhage;
- cerebral stroke;
- typical multiple sclerosis;
- prolonged migraine;
- other disorders of the spinal cord or brain.
Sometimes paresis develops in patients with laryngotracheitis, typhoid fever, syphilis, botulism and syringomyelia.
Flaccid paresis of the lower extremities (for example, peripheral paresis of the lower extremities) can occur due to various diseases. It manifests itself as a decrease in strength in one or more muscles.
The clinical picture depends on the cause and type
In the case of spastic paraplegia of central origin, the most often diagnosed is the symmetry of the pathology of the corticospinal or pyramidal motor tract, which can arise at any of its levels.
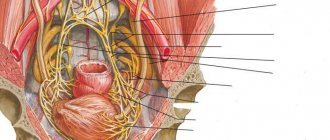
The appearance of paraplegia of peripheral origin is usually due to either the involvement of both anterior horns of the spinal cord in the process, or there is a connection with the pathology of the anterior roots, plexuses, and peripheral nerves.
A characteristic feature of spastic paraplegia, in addition to signs of paralysis of the muscles of the limbs of the same name, is the appearance of symptoms of muscular hypertonicity (spastic hypertension).
Extrapyramidal system in the central nervous system
Lower spastic paraplegia can be of the following nature:
- flexor flexion;
- and extensor extensor type.
For the flexor type (Babinski paraplegia, which occurs due to a particularly large process in the spinal cord, or in patients with a high degree of exhaustion or with the development of bedsores), hypertonicity is characteristic, leading to the development of contractures in the flexor muscles of the hip and lower leg.
Extensor paraplegia, which has a predominant distribution, is characterized by hypertonicity of the extensor muscles of the hip and leg, with the involvement of the plantar flexors of the feet, which leads to straightening of the lower extremities.
Tendon and periosteal reflexes in this type of disorder are excessive - but the skin reflexes fade and pathological reflexes appear, both extensor and flexion, as well as protective and synkinesis reflexes (global and coordinating).
Spasticity
Spastic paraplegia is manifested by an increase in the level of knee and Achilles reflexes, as well as the appearance of pathological reflexes (Gordon, Schaeffer, Babinsky, Oppenheim, Rossolimo).
Babinski reflex
The possibility of developing this paraparalysis can be caused by both a symmetrical subcortical lesion of the corona radiata and involvement of the pyramidal system in the process (at the level of the internal capsule or on one of the sections of the corticospinal tract).
One of the most common causes of paraplegia is transverse spinal cord injury. Moreover, with symmetrical damage to the spinal cord, the following appears:
- when the upper cervical segments are involved - spastic tetraplegia;
- in case of damage to the thoracic segments - lower spastic paraplegia.
The manifestation of the pathology will be expressed by the protective reflex Bekhterev - Marie - Foix: in response to heat, cold, or painful stimulation of the limb due to flexion in the hip, knee and ankle joints.
The occurrence of synkinesias (coordinating friendly movements) is also characteristic: the tibial phenomenon-Strumpel synkinesis with involuntary flexion of the foot with its supination and simultaneous extension of its big toe when trying to flex the limb at the knee and hip joints and Raymist synkinesis - repetition of actions by the affected leg (adduction and abduction) performed with a healthy leg.
Motor symptoms of spastic paraplegia are accompanied by disturbances of coordination, sensitivity, tissue trophism and pelvic disorders.
With a complete transverse section of the spinal cord with damage to the pyramidal and extrapyramidal tracts, spinal spastic paraplegia can develop into flaccid paraplegia with attenuation of not only tendon, but also periosteal reflexes and muscle atony.
Sluggish development of the disorder
Flaccid paraplegia is caused by bilateral damage to peripheral motor neurons due to:
- polio;
- spinal injury;
- plexites;
- polyneuritis;
- intramedullary tumors.
A characteristic feature is the absence of muscle tone in the limbs, attenuation of reflexes, both tendon and periosteal, muscle atrophy with suppression of electrical excitability (degeneration reaction) and with electromyogram indicators indicating damage to peripheral motor neurons.
Pathology of central motor neurons leads to paraplegia, flaccid either permanently or at certain stages of development, most often at the beginning or at the very end of the disease.
A pathology that continues throughout the entire duration of the disease in a sluggish form, characterized by atony, attenuation of tendon and periosteal reflexes, is always a manifestation of complete or almost complete rupture of the spinal cord due to injury. It is manifested by depression of sensitivity, advanced disorders of the pelvic organs, and bedsores.
If flaccid paraplegia occurs suddenly as a result of injury, this does not always indicate a complete transection of the spinal cord - this picture may be a consequence of diaschiosis. As it weakens, the symptoms of flaccid give way to the symptoms of spastic paraplegia.
A process that spreads more and more throughout the spinal cord and compresses it more and more. A tumor of the spinal cord occurs, which leads to the fact that his paraplegia, spastic at the beginning, eventually turns into flaccid.
Paraplegia that develops due to bilateral damage to peripheral motor neurons is always flaccid paraplegia, characterized, in addition to atony, by extinction of tendon and periosteal reflexes.
Spastic paraplegia - main types
There is a significant difference between flaccid peripheral paraplegia and those of central origin: the former result in muscle loss of mass and irreversible degeneration of their structure with a drop in electrical excitability.
Symptoms
Patients with paresis of the lower extremities experience the following symptoms:
- gait changes: gait disturbance is associated with weakening of the pelvic girdle muscles. The patient’s steps become “waddling” from one foot to the other;
- the leg muscles weaken: it is difficult for the patient to walk and even get up from a sitting position;
- the tone of the extensor muscles of the lower extremities decreases: when raising the legs, the feet may hang helplessly;
- hypotonicity or hypertonicity of muscles occurs;
- deep or pathological reflexes appear (Zhukovsky, Babinsky);
- the activity of the circulatory system is disrupted: lack of movement of the legs and feet leads to a deterioration in their blood supply and atrophy of the walls of blood vessels, which can lead to the development of disorders of the entire cardiovascular system.
Strumpel's paraplegia
Synonyms for the name: Erb-Charcot-Strumpel disease, or familial spastic paraplegia.
This is a disease with an inherited defect of the nervous system - bilateral degeneration of glia of the pyramidal tracts in the cords (lateral and anterior) at the level of the thoracic and lumbar regions of the spinal cord, with the involvement in subsequent stages of the pyramidal fibers of the brain stem and partial death of Betz cells in the motor zone of the cerebral cortex.
The mechanism of inheritance is autosomal dominant, or autosomal recessive, or it is X-linked; the genes responsible for the transmission of pathology have already been identified.
Due to genetic heterogeneity, the disease can manifest itself between the 1st and 7th decades of life as symmetrical lower spastic paraplegia, manifested by:
- gradual development;
- early appearance of tendon reflexes;
- rapid fatigue of the legs from walking;
- stiffness;
- cramps in the leg muscles of a tightening nature;
- spastic gait;
- increased level of tendon reflexes;
- clonus of the feet and patellas;
- the formation of contractures and deformities of the feet with the formation of a “hollow foot” - with its shortening and increase in height.
When the upper extremities are involved, which happens in the advanced stage of the disease, this does not affect sensitivity and intelligence.
Possible damage to the optic and oculomotor nerves (II and III pairs of cranial nerves), the occurrence of dysarthria, ataxia, nystagmus, and intention tremor.
MRI demonstrates a picture of characteristic atrophy of the spinal cord along its entire length, with particular severity in the cauda equina region.
In differential diagnosis, this disease is indicated by:
- late onset of the disease with a slowly progressive course, complicated by spastic paraplegia, with normal psychomotor development;
- maintaining the patient’s ability to walk until adulthood;
- health of heterozygous family members.
Associated symptoms
With a bilateral process in the cerebral cortex with a tumor in the upper third of the precentral gyrus, spastic lower paraparalysis is often accompanied by Jacksonian epilepsy with the appearance of clonic convulsions with their onset in the leg muscles.
In children, spastic diplegia is characterized by insurmountable spasticity of the leg muscles with a pronounced adductor dominance and the formation of a characteristic gait, or even the inability to walk independently. The pathology is also manifested by combined athetotic hyperkinesis of the muscles of the arms and face.
General principles of treatment
The main actions should be aimed at eliminating the causes of paraplegia:
- surgical removal of the tumor;
- elimination of spina bifida;
- treatment of nervous system infections;
- and similar measures.
Prescription of medications is made taking into account the nature of the pathology.
With spastic paraplegia, electrotherapy can lead to increased contractures, while with its peripheral origin, this method of influence will give a favorable result.
In case of multiple sclerosis, or systemic sclerosis, spondylitis of tuberculous etiology, mud therapy is contraindicated.
With lower paraplegia, the emphasis should be on the development of the muscles of the upper extremities, the condition of which determines the subsequent fate of the patient. And here the first step to getting out of helplessness is learning the art of sitting in bed.
Symptomatic treatment is prescribed to relieve the underlying concomitant pathology. Antihypertensive, anticonvulsant and antispasmodic drugs, and agents to improve tissue trophism are prescribed.
Balneological procedures are also used, and the use of mud therapy, massage and exercise therapy is indicated.
When does the disorder most often occur?
Monoparesis can occur due to damage to the peripheral or central nervous system. Let's take a closer look at these violations.
The occurrence of the disease is most often associated with the fact that peripheral motor neurons are affected and their sensitivity is impaired.
With this type of paralysis, the muscles weaken significantly, and the muscles' resistance to gravity is reduced or completely absent.
Monoparesis, which is caused by lesions directly in the muscle tissues themselves, is extremely rare.
Lesions of the peripheral nervous system that may cause this syndrome include disorders such as neuropathy, radiculitopathy, and plexopathy. In this case, the muscles weaken, sensitivity decreases, and pain occurs.
The rarest are monoparesis due to lesions of motor neurons in the central nervous system. This type of paralysis, which is a consequence of disturbances in the functioning of the central nervous system, is usually caused by embolic cortical infarction. In this case, paralysis affects the arms more often than the legs.
During the first days of disease development, central paresis is not easy to distinguish from peripheral paresis. This is due to the fact that the main signs of central paresis, such as spasticity, do not appear immediately.
From the practice of a neurologist
As an example, it is worth citing a treatment regimen for lower paraplegia, of central origin, due to spinal cord injury in a young patient, where complex treatment had a noticeable effect:
- Actovegin
- intravenous stream; - Trental
- intravenously; - Prozerin
; - vitamin B12
intramuscularly; - massage of the lower extremities
in combination with physical therapy; - acupuncture and electrical myostimulation
of extensor muscles
This is a set of measures that were prescribed in addition to independent physical activity on the shoulder girdle and early learning to sit in bed, to help overcome the fear of which psychotherapy sessions helped.
The combination also gave satisfactory results:
- muscle relaxant Mydocalm
; - Sibazon,
which has a complex sedative-hypnotic, anticonvulsant and anxiolytic effect ; - Pentoxifylline
is a means to improve microcirculation; - Milgamma
is a complex of B vitamins; - ATP
- tissue energy stimulator; - Cerebrolysin
is a nootropic drug.
Modern view of therapy
Since monoparesis is a secondary disease, that is, it occurs as a result of diseases, treatment methods should be aimed at combating the cause of paralysis. The following methods are used in the treatment process:
- Drug therapy includes the use of drugs aimed at treating the underlying disease. For example, if the development of a disorder is associated with hemorrhage in the brain, then drugs are prescribed to restore blood circulation in the brain tissue.
- In this case, massage sessions These measures are aimed at restoring muscle function.
- Physical therapy includes a set of exercises with passive movements. In this case, the exercises are performed both for the affected limb and for the healthy one, and the load should be the same.
- For monoparesis of the arms and legs, a method of physiotherapy such as electrophoresis . This allows you to restore nerve impulses and improve the condition of tissues in the affected limb.
- In addition to the above, you should visit the pool , since swimming improves the condition of the muscles, which can increase the effectiveness of the treatment.
- In addition, it is necessary to take vitamin and mineral complexes .
In conclusion, it should be mentioned that paresis of the limbs is a fairly serious disorder that significantly complicates a person’s life and can lead to dangerous consequences.
To avoid complications, the disease must be treated in the early stages of its development under the supervision of competent specialists.
Possibility of complications and prognosis
{banner_banstat9}
Prognostically, flaccid and spastic flexor paraplegia is less favorable than spastic extensor paraplegia. The inability to develop labor skills due to muscle weakness of the legs should also be considered an unfavorable prognosis for the patient.
Complications of the disease are complete loss of the ability to move independently due to the progression of the emerging pathology, disability and the appearance of pelvic disorders and trophic disorders-bedsores.
There are currently no proven, reassuring treatments for paraplegia.
Comparatively good results are obtained only by using traditional Chinese medicine methods in the form of acupressure, reflexology, acupuncture, using electric needles and a lamp with Chinese herbs, drinking fresh herbal infusions prepared according to an individual recipe, herbal boluses and similar methods of influence.
Diagnostics
An important role in the diagnosis of paresis belongs to a careful collection of anamnesis and determination of how prone the patient is to the occurrence of typical psychogenic reactions.
Microlaryngoscopy is used for modern examination of patients with laryngeal paresis at the Yusupov Hospital. In addition, radiography and computed tomography of the larynx are additionally prescribed. Clinic specialists evaluate neuromuscular transmission and muscle contractility. To confirm the diagnosis, an X-ray examination may be prescribed.
When diagnosing paresis of the limbs, the extent of distribution and localization of existing muscle weakness is taken into account.