A microstroke is microdamage and disruption of the brain as a result of lack of oxygen; the first bell before a stroke. It does not cause significant harm, but is an indicator of various disorders. At the same time, doctors generally do not call such a disease as a microstroke; now they are increasingly inclined to think that this is the same stroke (only in a mild form) or a transient cerebrovascular accident. But, no matter what we call this disease, the fact is a fact: it exists, affects people and has its consequences.
Differences between a minor stroke and an ischemic one
In fact, in terms of symptoms, these two diseases are quite similar (even to diagnose a microstroke at home, the patient needs, for example, to try to raise both arms; the same exercise is used for stroke). They are distinguished only by their duration (a ministroke comes and goes quickly) and the consequences for the body (a minor stroke can go away on its own, without medical intervention). But the diagnostic and treatment methods are the same, because usually a microstroke foreshadows the onset of an ischemic one.
Make an appointment
Possible manifestations: numbness and immobilization of one half of the face, unsteadiness of gait, severe headache, dizziness. Symptoms can be isolated or combined. With microstrokes, the symptoms disappear within 24 hours.
Tests and diagnostics
All patients with transient ischemic attack should be examined within 24 hours of the onset of neurological symptoms. Since there is no brain damage in a microstroke, computed tomography or magnetic resonance imaging will not help diagnose this disease, but they are performed to rule out a stroke.
- Magnetic resonance imaging in a diffusion-weighted mode provides accurate and early diagnosis of ischemic brain damage. Diffusion-weighted magnetic resonance imaging is based on the study of the diffusion of water molecules in normal and altered tissues.
- For diagnosing microstrokes, a more informative research method is duplex ultrasound examination of intracranial vessels and neck vessels. This allows us to identify the presence of occlusion and its degree. Ultrasound and Doppler studies are of less value in assessing vertebral arteries where occlusion cannot be corrected.
- If damage to the vertebral arteries is suspected, angiography - a contrast agent is injected into the artery and pictures of the head and neck are taken. CT angiography examines the condition of the arteries of the neck and large branches of cerebral vessels.
- In addition to CT angiography, perfusion computed tomography after intravenous administration of a contrast agent is performed to study cerebral blood flow at the capillary level.
- a cardioembolic microstroke is suspected, echocardiography is performed, which allows identifying cardiac pathology.
- For differential diagnosis with an epileptic attack, electroencephalography is performed.
- Clinical and biochemical blood test (coagulogram).
- Blood sugar test.
- Lipidogram.
Myths about microstroke
Many of us have heard the name “ministroke,” but not everyone knows what it is and why this condition is dangerous.
To begin with, we note that, at the same time, it is necessary to distinguish between this condition and a stroke, and not.
Why?
- A disease that doesn't exist? Experts do not separately identify such a disease as microstroke. In the medical lexicon, this is called transient cerebrovascular accident (TCI);
- "Micro" disease? The prefix “micro” in the word is only misleading: it does not mean at all that there is no need to be afraid of this condition or that there is no need to take urgent measures to eliminate it; rather, on the contrary, it emphasizes the “kinship” with stroke with only one difference - in symptoms. The symptoms of a minor stroke are not as severe as those of a cerebral hemorrhage, and they go away much faster.
- Is it possible to recover? After a mini-stroke, the body can often recover without the help of a doctor, but it is still worth getting examined: even if the symptoms have already disappeared, the specialist should know that they were there. Thus, it is more likely that relapses and strokes will be prevented.
The “micro” in the word does not make this disease insignificant, it only hints that the disease is reversible (unlike a full-blown stroke). Therefore, diagnosis and treatment should be approached with full responsibility. So what myths about microstroke are just myths and should not be believed?
- Minor stroke is a rare disease. Unfortunately, it is not. Every year it affects tens of thousands of people, and many of them, without proper treatment, lead to disability.
- Only old people can get sick. Unfortunately no. This disease increasingly affects people aged 20-30 years. True, a young body usually fights the consequences better than an older person’s body, but that’s another story.
- What can happen cannot be avoided: a stroke cannot be prevented. This is also a myth. There are certain preventive measures that can help avoid encountering this unpleasant disease.
- A microstroke cannot be recognized: the symptoms are too mild. In part, this is not a myth; the symptoms are really mild. But if you have the signs described above, the time-tested exercise “raise both arms up” is suitable - one part fails during a microstroke, so the patient can only raise one arm.
- Micro-stroke, stroke and heart attack are the same thing. If we mentioned the differences between the first two diseases above, then the third differs from both of them in location. A heart attack is located in the heart, while a (micro)stroke is located in the brain.
Diagnosis of microstroke at the Yusupov Hospital is carried out using modern medical equipment. European CT and MRI installations make it possible to accurately determine the location of the lesion and its extent. An individual treatment and rehabilitation program is developed for each patient. The recovery period takes place under the supervision of experienced neurologists, massage therapists, exercise therapy instructors and physiotherapists. A personal approach can reduce the time of hospital stay and reduce the risk of recurrent microstroke.
Classification
According to the mechanism of development, transient circulatory disorders are:
- Cardioembolic , caused by the reflux of emboli from the cavities and heart into the vessels of the brain.
- Atherothrombotic , associated with the formation of a blood clot on an atherosclerotic plaque, which causes blockage of the artery lumen.
- Hemorheological , caused by increased blood viscosity and an increased tendency to thrombus formation.
- Hemodynamic , developing with a sharp drop in blood pressure (with orthostatic hypotension , cough , hyperventilation , overdose of antihypertensive drugs, hypovolemia or myocardial infarction ).
- Cryptogenic - unspecified, of unknown origin, developed without atherothrombosis or embolism .
By severity:
- Lungs - the duration of neurological disorders does not exceed 10 minutes.
- Moderate severity - disturbances last several hours.
- Severe, lasting up to 24 hours.
By frequency of manifestations:
- Rare - transient attacks occur 1-2 times a year.
- Medium frequency - repetition of attacks 3-5 times a year.
- Frequent, in which attacks are repeated once a month or even more often.
According to some authors, transient disorders in the carotid system occur 4 times more often than in the vertebrobasilar region. According to other authors, the occurrence is greater in the vertebrobasilar region in the same proportion.
The main difference between transient cerebrovascular accidents is the instability and reversibility of the pathological process. Microstroke in men occurs with the same frequency as microstroke in women. In the latter, additional causes include the use of oral contraceptives. The use of oral contraceptives causes a deterioration in the rheological properties of blood and increases its viscosity, which are factors in the formation of blood clots.
Causes of microstroke
- Atherosclerosis (in this case, the cause of the disease is a plaque in the vessels, which either comes off or sticks to the wall of the vessel: both lead to obstruction of blood through the vessel);
- Thrombosis - separation of a blood clot, disruption of the nutrition of neurons in the lower extremities;
- Vascular spasm, as a result of which blood does not flow to the brain;
- Anemia - a drop in hemoglobin levels, a decrease in oxygen levels in the brain;
- Increased blood viscosity (usually due to chronic diseases, polycythemia, insufficient fluid intake);
- High blood pressure;
- Obesity (there is an increased load on the heart when the body has extra pounds);
- Hereditary brain pathologies;
- Heart attack and other heart diseases that weaken it;
- Previous heart surgery;
- Stress (provokes increased blood pressure);
- Age (despite the fact that this disease is getting younger, more often older people still suffer from it, since their blood vessels are worn out);
- Abrupt climate change (more than 10 degrees).
Medicines
The following groups of medications are used to treat pathology:
- Antihypertensive drugs. Arterial hypertension is the most important risk factor for TIA and stroke, so it is important to keep your blood pressure under control at all times. It should be less than 140/90 mmHg. Art., it is gradually brought to the figures of 130/80 mm Hg. Art. Drugs to lower blood pressure are prescribed the next day after the attack and are selected individually. If the blood pressure is persistently elevated, a combination of several agents is used. Reduce blood pressure below 120 mm Hg. Art. is not recommended, since in this case it is possible to deteriorate blood circulation in the brain and develop a repeated ischemic attack.
- Vascular agents and nootropics are used to restore cerebral circulation and brain functions. These include Cavinton, Cinnarizine, Piracetam. Medicines of animal origin are used - Actovegin, Cortexin. The listed remedies improve blood circulation and eliminate the consequences of a micro-stroke.
- Antiplatelet agents are medications that prevent blood cells from sticking together in the vascular bed. Used to prevent blood clots. Some patients who have suffered an ischemic attack are prescribed antithrombotic drugs for life. Most often, low doses of Aspirin are used to prevent thrombosis - from 50 to 150 mg/day. Aspirincardio and Cardiomagnyl are used. If the patient has problems with the digestive system, Aspirin is combined with antacids - magnesium hydroxide, calcium carbonate.
- Medicines to lower cholesterol. It is known that people with blood lipid disorders are at risk of getting a stroke more often than others. To normalize indicators, statins, fibrates, and cholesterol reabsorption blockers are used. Nicotinic acid acts in several directions: it not only reduces “bad” cholesterol, but also improves blood circulation, dilates blood vessels, relieves spasms and normalizes blood pressure. The goal of therapy is to achieve cholesterol levels <4.5 mmol/L.
Cardiomagnyl
Important! The doctor selects a set of medications. The characteristics of the patient, the presence of hypertension, atherosclerosis, obesity and other risk factors are taken into account.
The first signs of a microstroke
The very first sign of a microstroke is numbness of the extremities for a short time (many patients attribute it to “numbness” of the leg or arm). Also, the first, that is, appearing earlier than others, signs of a microstroke include:
- Short painless blindness in one eye (as if a shadow had crept into the field of vision for 20-30 seconds);
- Temporary and sudden numbness of the face (the person will not be able to smile);
- Loss of the ability to speak coherently (sounds and words are confused, sometimes it is impossible to utter a word at all);
- A sharp headache (like a flash) - does not go away even if you take any medications;
- Short-term disturbances in coordination of movements are possible (objects fall from hands, the patient simply cannot lift them for some time);
- The skin becomes pale;
- Weakness appears throughout the body (a person suddenly wants to sit down or lie down);
- Sweating increases sharply for no apparent reason.
Possible consequences
A microstroke is a serious phenomenon that most often leaves behind temporary or permanent consequences of this kind:
- Headaches and slight dizziness;
- Increased fatigue;
- Absent-mindedness and inability to focus attention;
- Drowsiness and general weakness;
- Sudden mood swings.
If the problem is not treated in a timely manner, very dangerous consequences may occur in the form of:
- Paralysis;
- Problems with coordination, memory, speech, vision;
- Development of mental disorders;
- Problems with normal urination and swallowing.
To prevent such problems, it is necessary to provide timely assistance to the patient and call an ambulance.
The first symptoms of a microstroke
In terms of symptoms, a microstroke is not very different from a traditional one. The most important difference is the duration of symptoms (usually no more than a few hours) and its intensity (signs are not as noticeable as with a stroke). Symptoms manifest themselves differently, depending on the location of the outbreak (the place where blood circulation is impaired):
- Occipital lobe of the brain (responsible for the perception of visual information): there is visual impairment to complete blindness in one or both eyes;
- Parietal lobe (responsible for tactile sensations): loss of smell, sensation of movement under the skin.
- Temporal lobe (responsible for hearing and memory): short-term memory and hearing loss.
- Frontal lobe (responsible for intelligence and muscle tone): paralysis, mood swings.
The body usually overcomes this condition on its own, and the brain is not seriously damaged.
As already noted, a micro-stroke often hardly manifests itself: the symptoms are very mild, which is why they are so easy to overlook. But it’s still worth paying attention to these first signs of the disease:
- Numbness of the whole body (or one part of it, so it may be impossible to smile or raise both arms);
- Dizziness;
- Severe headache;
- Double vision;
- Unsteady movements, weakness, desire to sit down or lie down.
To diagnose a microstroke at home, you can use the FAST test. It was developed in America for emergency doctors so that they could easily diagnose cerebral hemorrhage. This test is also suitable for a micro-stroke, since the symptoms (facial distortion, weakened arms and incoherent speech) are also present in this case, although they pass much faster. FAST is an abbreviation, but the word itself is translated from English as “quickly” - one of the main rules when diagnosing a disease.
F (face - “face”) - you need to pay attention to the victim’s face: it can be unnaturally skewed.
A (arms - “hands”) - the patient’s hands do not obey: they are weakened, trembling and do not rise up.
S (speech - “speech”) - words are confused, it is impossible to pronounce even a simple sentence without errors.
T (time - “time”) - time: so precious in the case of this disease. It is better to start diagnostics as soon as the first signs appear, because as soon as they pass (with a microstroke this usually takes no more than an hour or two), the patient will feel great again. But for emergency doctors, diagnosing the symptoms will help a lot.
Who does the disease affect?
This disease is getting younger and, if previously it was believed that it only affected older people, now this is not the case. Much depends on the person’s health status, lifestyle and chronic diseases.
Still, patients with the following problems are at risk:
- Atherosclerosis (chronic artery disease);
- Hypertension (pressure surges can trigger a minor stroke);
- Vascular lesions;
- Diabetes mellitus (high sugar content affects the walls of blood vessels);
- Alcohol abuse (the functionality of brain vessels decreases, toxins destroy tissue);
- Congenital and acquired heart diseases.
Busy people suffer a micro-stroke on their feet, that is, they do not pay attention to its symptoms and first signs, trying to maintain their usual activity. This should not be done under any circumstances, since within 24-48 hours there is a high risk of a stroke; the consequences in this case can be disability and even death. Therefore, a minor stroke is an indication for emergency hospitalization of the patient.
Causes
The main causes of transient cerebral circulatory disorders are identified:
- Hyperlipidemia and atherosclerosis . Atherosclerotic damage to the carotid and brachiocephalic arteries is the basis for atherothromboembolism , which causes micro-stroke in 50% of cases.
- Arterial hypertension . Damage to cerebral vessels in hypertension is associated with changes in small arteries, arterioles and capillaries, which acquire pathological tortuosity, lose elasticity and the ability to quickly expand when necessary. In addition, arterial hypertension accelerates the development of atherosclerosis , which is an independent risk factor for micro-stroke.
- Anomalies of the development of the vertebral and carotid arteries.
- Angiopathy due to diabetes mellitus .
- Vascular damage in systemic diseases, vasculitis .
- Hematological diseases ( sickle cell anemia , erythremia , leukemia ).
- Carotid stenosis , which causes microstroke in 50% of cases.
- Heart diseases with rhythm disturbances (for example, atrial fibrillation ), in which there is a tendency to form blood clots in the cavities of the heart and there is a risk of cardiogenic thromboembolism .
- Obstructive sleep apnea .
- Coagulopathies ( protein C , antithrombin III protein S deficiency ).
Predisposing factors:
- Smoking.
- Physical inactivity.
- Alcohol abuse.
- Overweight.
- Hyperhomocysteinemia.
If we consider the causes of disturbances in the vertebrobasilar system, these will be a variety of conditions and diseases leading to obliteration of the vertebral arteries:
- Tortuosity of the arteries (characteristic of arterial hypertension), which can lead to kinking of the vertebral artery - stenosis will form and blood flow will be disrupted.
- Congenital anomalies of the vertebral arteries. Insufficiency of blood flow in one vertebral artery can be compensated for a long time by another vertebral artery. With age and the development of atherosclerosis and arterial hypertension, decompensation occurs.
- Changes in the rheological properties of blood. This refers to an increase in platelet and blood viscosity, an increase in hematocrit - all these conditions in the body worsen microcirculation.
- Compression of the vertebral artery by an osteophyte , an articular process (for example, with instability of the cervical spine), a spasmodic neck muscle, or an accessory cervical rib.
Insufficiency of blood flow in the vessels of the vertebrobasilar system is manifested by attacks of falling, but without loss of consciousness (drop attacks), which occur with sudden turns of the head or throwing back the head. The risk group for the development of micro-strokes includes people who have:
- severe osteochondrosis of the cervical spine;
- previous skull injuries and concussions;
- constant nervous professional stress;
- congenital vascular pathology.
Types of microstroke
There are three main types of microstroke:
- Hemorrhagic stroke is hemorrhage with the formation of hematomas. Recovery takes from two weeks to several months.
- Ischemic stroke leads to blockage of blood vessels by blood clots. It differs from hemorrhagic in its increasing effect. In most cases, patients are diagnosed with this type of microstroke.
- Lacunar strokes involve damage to small arteries in the brainstem or cortex.
It is important to correctly diagnose the type of microstroke in order to provide assistance to the patient. A minor stroke is dangerous because it can recur and, without proper treatment, lead to extensive hemorrhage in the brain.
Types of microstrokes
Microstrokes are divided into two types, based on the cause of their occurrence:
- Ischemic occurs when the blood supply to certain parts of the brain is stopped due to obstruction of blood vessels or arteries. It does not matter what blocked the blood flow - a blood clot, a blood clot or an overgrown atherosclerotic plaque.
- A hemorrhagic stroke is a microstroke that occurs as a result of a hemorrhage that occurs when a small vessel ruptures. In addition, thinning of the vascular wall is also a risk of intracerebral hemorrhage.
Both conditions are dangerous and require the help of qualified professionals.
Diagnosis of microstroke
Despite the fact that this disease, compared to traditional stroke, is relatively harmless, it still needs to be diagnosed and treated. Although a microstroke occurs and passes quickly, it still causes some harm to the body and in half of the cases ends in a stroke or heart attack. That's why diagnosing the disease is so important. To make a correct diagnosis, the patient is prescribed the following examinations:
- ECG and ultrasound of the heart;
- Vascular examination;
- An echocardiogram determines any abnormalities in the heart;
- Blood test for platelet count, clotting time, sugar, etc.
- CT can detect a blood clot and determine its nature.
- REG (rheographic method for studying the vascular system of the brain) and ultrasound examination (ultrasound examination) with functional tests (for example, with turns and tilts of the head) - these methods are necessary for examining the arteries of the spine.
- MRI will allow you to detect the location of the blood clot with high accuracy.
It may be necessary to involve other specialists. For example, an ophthalmologist determines the visual field and conducts an examination of the fundus.
Pathogenesis
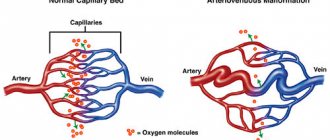
The key point in the pathogenesis of this condition is reversible cerebral ischemia, which occurs when there is a mismatch between the needs of the brain and the currently existing blood supply. Local anemia of brain tissue develops when perfusion decreases below 18-22 ml of blood per 100 g/min.
A transient drop in blood flow, due to various reasons, causes the development of ischemia in the brain tissue and is accompanied by reversible focal symptoms. The main pathogenetic mechanisms for the development of transient disorders are: microembolism ; hypotonic and hypertensive crisis , pathological tortuosity of the main vessels of the brain, as well as disorders of the anticoagulation system of the blood.
The outcome of ischemic cerebral circulatory disorders is determined by the caliber of the artery, the rate of development of blockage, localization, and the development of collateral circulation. If cerebral perfusion is restored, regression of symptoms is observed and the episode of transient ischemic attack ends. In the event of a further drop in blood supply to 8-10 ml per 100 g/min, which causes irreversible changes in brain tissue, cerebral infarction ( ischemic stroke ) develops.
Treatment of microstroke
Treatment is aimed at normalizing blood supply and metabolism, preventing relapses and preventing stroke. In case of hemodynamically significant occlusion of large arteries, surgical treatment by angiosurgeons is possible. Patients with a ministroke are usually prescribed:
- Drugs aimed at restoring blood microcirculation in blood vessels;
- Drugs that dilate blood vessels and improve blood flow;
- Agents that prevent platelet accumulation;
- Drugs that improve brain activity;
- Vitamins.
During the rehabilitation period, the patient visits:
- Exercise therapy (to restore motor activity);
- Massage sessions (to stimulate motor activity in the limbs);
He also follows a diet (without fatty, spicy and salty foods) and does special breathing exercises (to ensure that sufficient volume enters the body).
But if the patient delays diagnosis and treatment, complications may arise. In this case, with a microstroke, the doctor prescribes the following groups of drugs responsible for restoring the body:
- improving blood microcirculation;
- improving metabolic processes in blood vessels;
- dilating vessels;
- preventing the formation of blood clots;
- stimulating brain activity;
- vitamins (to strengthen the immune system and improve brain activity).
Forecast of microstroke
If the disease was diagnosed on time, no serious consequences are observed in patients after a mini-stroke. In young patients, the rehabilitation period can take only a few days; in older patients it usually takes up to a month. If a person begins to pay due attention to his health and follow the doctor’s recommendations, the prognosis is favorable, but if not, he should expect a recurrence of the attack, including an increased possibility of a stroke.
During the rehabilitation period, patients may experience the following disorders:
- Men at a young age experience memory loss, erectile dysfunction, frequent headaches, seizures, and mood swings.
- In women, the consequences usually affect the nervous system and are associated with frequent mood swings and even possible depression.
- In the elderly: difficulty in motor activity, decreased vision, epileptic attacks, decreased memory and mental activity, speech impairment, sclerosis.
If the patient does not receive timely treatment, the microstroke may return within two to three days, and 50% of patients subsequently develop an ischemic stroke. In this case, mortality increases from 10 to 40%.
Micro-stroke “on your feet”
Since the symptoms of a mini-stroke can last for a fairly limited time, some resilient men can suffer them without even stopping their daily activities. It seems to them that nothing terrible is happening - just a slight malaise, which goes away after an hour. Accordingly, neither a visit to a doctor nor adequate treatment occurs here.
This is very dangerous, because an ignored attack often becomes the reason for its rapid recurrence or, in general, the main factor in the development of cerebral ischemia. If this happens, the consequences will be very serious, including disability, and treatment will take several months or even years.
How to recover after a mini-stroke?
The following principles that patients adhere to contribute to rehabilitation and speedy recovery:
- A doctor is a specialist. And you need to trust specialists. If the patient is incompetent in matters of treatment and rehabilitation, it is worth following the doctor’s recommendations and taking the medications he prescribed;
- Don’t put it off until tomorrow... If a patient needs to do exercise therapy every day, this means that classes cannot be missed, otherwise the desired effect will not be achieved;
- The importance of support. After a ministroke or, worse, a stroke, the support of loved ones is very important for the patient. Sometimes they simply give up, patients become depressed, and only family and friends are able to influence and help a person they know well. You can accompany the patient to a massage or exercise therapy, help him prepare food so that it fits the diet, and just talk. Feelings of loneliness should not be present in rehabilitation.
- Systematicity. This means that if a patient is prescribed exercise therapy, he should not miss a single day; if he has a diet, then he needs to strictly follow it. In terms of timing, rehabilitation after a mini-stroke is an individual process, since everything depends on the degree of impairment and the patient’s condition.
- Gradualism. This means that the body does not recover immediately, it needs time. This means that it is better to leave the usual active workouts for later, and immediately after a micro-stroke go for a massage or exercise therapy.
Also, recovery and rehabilitation after a mini-stroke imply the following actions:
- Drug treatment
- Restoration of motor functions
- Vision restoration
- Restoration of speech function
- Normalization of psychological state
A ministroke usually affects the lower and upper extremities, and motor function is impaired. The grasping reflex may disappear, weakness in the arms and legs may appear (symptoms may intensify and then it will be impossible to move at all).
The following methods are used to restore motor functions:
- Exercise therapy. Therapeutic exercise is designed to normalize muscle tone and restore strength to the muscles.
- Massage. This procedure relaxes, stimulates blood circulation and normalizes muscle tone. In this case, a massage session can be carried out both by a specialist and by the patient himself, if he is ready to strictly follow the doctor’s recommendations. You can also combine a procedure with a specialist and a home massage. This approach will speed up the recovery process.
- Physiotherapy. After a micro-stroke, the patient is usually prescribed warming, which allows the body to regain lost sensitivity.
Vision restoration
Frequent symptoms of a microstroke are double vision, darkening, spots, and even temporary blindness in one or two eyes at once. While the patient is undergoing treatment, the issue of vision restoration is dealt with by an ophthalmologist, and less often by a surgeon (if it is impossible to avoid surgical intervention).
During the rehabilitation period, the patient is usually prescribed pills that normalize vision function, and is also recommended to perform special exercises that stimulate the work of the oculomotor nerve. To record progress or regression, it is recommended to visit a doctor regularly.
Restoration of speech function
Confusion of speech is another symptom of a mini-stroke, which can be cured with proper treatment. But, if after treatment the speech function is not completely restored, special classes are conducted with the patient aimed at its restoration. They are usually carried out by a speech therapist or neuropsychologist. In case of complications and serious speech disorders, all basic speech skills are studied with the patient from scratch: listening (understanding what is heard), reading, writing, speaking.
The process of speech restoration will accelerate if the patient’s relatives continue to study with him at home. For the process to be effective, in addition to training with the victim, you just need to talk (ask him simple questions, patiently waiting for an answer; tell the news; share opinions, etc.), even if this seems useless at first glance. But we must remember that a person can only speak in a linguistic environment (that is, he must constantly hear speech in order to begin to produce it), which is the task of family and friends to create during the rehabilitation period.
Normalization of psychological state
Patients who have suffered a mini-stroke often experience depression (people with a fine mental organization and women are especially prone to it due to their physiology and psyche). Relatives need to try to understand this condition: the patient suddenly lost some abilities, is forced to take pills and regularly visit the doctor. His life has completely changed. To help him overcome this condition it is necessary:
- Interact and communicate with him more often;
- Go for walks, which will provide him with physical activity;
- Help you find a new hobby or return to an old one, if possible.
As soon as rehabilitation is over, it is better for a person to return to work: to the old one or, if this is not possible, to find a new one as soon as possible.
Any activity requires a certain amount of effort and time, therefore, by getting busy, the patient will think less about problems and, accordingly, will quickly overcome a depressive state.
Where and how to undergo rehabilitation and how long will it take to recover after a mini-stroke? These are the most frequently asked questions by patients. Of course, everyone wants to return to normal life as soon as possible, go to work or go on a trip.
Rehabilitation is possible both at home and in a hospital setting. In the first case, success will depend on those who surround the patient: on their willingness to communicate, care and support. Secondly, it depends on the literacy of specialists and the development of the rehabilitation program.
Expert opinion
Author: Tatyana Aleksandrovna Kosova
Head of the Department of Rehabilitation Medicine, neurologist, reflexologist
According to statistics, the number of cases of first-time transient cerebrovascular accident is increasing every year. A microstroke is provoked by various factors. It has been noted that the disease is most common among men of working age. According to clinical studies, in 10-15% of cases, myocardial infarction develops after a transient cerebrovascular accident. 30-40% of patients experience a major stroke over the next 5 years. Therefore, it is important to seek medical help on time and undergo preventive examinations.
Diagnosis of microstroke at the Yusupov Hospital is carried out using modern medical equipment. European CT and MRI installations make it possible to accurately determine the location of the lesion and its extent. An individual treatment and rehabilitation program is developed for each patient. The recovery period takes place under the supervision of experienced neurologists, massage therapists, exercise therapy instructors and physiotherapists. A personal approach can reduce the time of hospital stay and reduce the risk of recurrent microstroke.
Nutrition for microstroke of the brain
After an acute cerebrovascular accident, patients need a nutritious diet that ensures the body receives a balanced amount of proteins, fats and carbohydrates. A necessary component of a healthy diet is a sufficient amount of vitamins and minerals in the food consumed. After a mini-stroke, it is important to maintain a water regime.
When selecting products from which to prepare dishes, nutritionists recommend giving preference to whole grains or products made from them. After a micro-stroke, you should eat orange and dark green foods, peas and beans. The menu should include a sufficient amount of fresh, frozen or dried fruits and berries every day.
Diet after a stroke is aimed at reducing the risk of another attack. When selecting food products, you should pay attention to the following criteria:
- nutritional value (calorie content);
- presence of fat;
- the presence of saturated and trans fats;
- do you have cholesterol?
- content of table salt and fiber.
Limiting your intake of trans fats will reduce blood cholesterol, which is of great importance in cases of brain damage.
The diet after a microstroke should contain vitamins and minerals. Vitamin B6 is present in the following foods:
- carrot;
- sunflower seeds;
- walnuts;
- spinach;
- peas;
- herring;
- salmon.
Legumes and whole grains are rich in potassium, and α-pinoleic acid is found in sea fish. An important component of the menu after a microstroke are fruits and vegetables, seeds and nuts. The energy value of foods consumed per day should not exceed 2.5 thousand kilocalories.
Why is memory impaired after a stroke?
The moment when a vessel in the brain becomes clogged or ruptures, a person may not notice, because... there may be no consequences of circulatory disorders. However, in situations where the circulatory system is significantly damaged and the blood does not deliver oxygen to one or another part of the brain, its cells stop functioning with proper efficiency and gradually die.
Cell necrosis is the main reason why various complications occur after a stroke: paralysis, speech dysfunction, memory loss.
Timely medical care and intensive rehabilitation sessions provide a chance to eliminate the negative consequences. Cells in a healthy area can take over the functions of those affected.
Scientists, based on cutting-edge brain research, view human memory in the light of three integral components that are involved in its formation and functioning:
- Short-term. The ability to store material in a short time period and small volume - about 20 seconds and several elements.
- Long-term. Unlimited in time and volume. Provides long-term storage of information.
- Operational. The ability to hold any amount of information and perform various operations with it in a short period of time.
Recording, storing and reproducing information is one of the main functions that makes a person capable and ensures his normal functioning. Each new source contributes to the formation of new neural connections. In a situation where a person needs to use the knowledge he has ever acquired, the neural connection is activated.
However, after a cerebrovascular accident, countless neurons die, and the connections that were formed between them are destroyed. This is how the process of memory loss occurs. Together with the killed neurons, a lot of material that a person has managed to accumulate during his life goes away.
The nature of the disorders depends on which area was destroyed and in which hemisphere of the brain critical changes occurred. The hemispheres work together, exchanging millions of impulses with each other every second. Their normal operation is impossible without the use of memory mechanisms. Therefore, it is very difficult to specify and accurately state what changes will be entailed by the death of one or another part of memory, and how this will affect a person.
In any situation, a patient with a stroke requires immediate medical attention and a long recovery process.
Prevention of micro-stroke
Prevention is always simpler and more effective than treatment, and preventive measures are usually the same, so by following simple rules, you can eliminate many diseases from your life. What should be done?
- Maintain normal blood pressure. Any stroke is a surge in pressure, so just measure your blood pressure at least once a day using a home blood pressure monitor;
- Give up bad habits: for example, coffee and alcohol increase blood pressure, smoking thins the walls of blood vessels. All this provokes strokes of varying severity;
- Follow the diet recommended by your doctor: it is aimed at reducing cholesterol levels and, accordingly, preventing the appearance of plaques;
- Exercise regularly: physical activity keeps all body systems in good shape;
- Monitor your sleep status, sleep at least 8 hours a day;
- Monitor hormonal levels;
- Seek help for head injuries;
- Visit doctors periodically and promptly treat vascular diseases.
Prevention
Prevention of transient ischemic attacks is:
- Following a diet with limited intake of salt and animal fats.
- Active lifestyle (moderate physical activity, swimming, walking, exercise, cycling).
- Normalization of weight.
- Stop drinking alcohol.
- To give up smoking.
- Regular examination and treatment in the presence of pathologies that are risk factors for transient ischemia and stroke ( atherosclerosis , diabetes , hypertension ).
Women with risk factors ( hypertension , obesity , dyslipidemia , migraine ) are not recommended to use high-dose estrogen contraceptives. Patients who have suffered a transient ischemic attack should constantly take antiplatelet, antihypertensive drugs and statins, the use of which reduces the risk of stroke by 30%. If there are indications, it is not recommended to refuse surgical treatment - carotid endarterectomy , stenting or angioplasty .
Main conclusions
A minor stroke is small because it is often followed by a large one and this can only be avoided if the disease is diagnosed in time. The fact that the symptoms were there but went away is not a reason to put off going to the doctor, not even a trip, but a trip by ambulance, because if a micro-stroke is diagnosed, doctors have only three hours to start treatment and reduce all risks to a minimum. The longer the disease goes undiagnosed, the greater the likelihood of complications.
It is also important to understand that if a person, for example, has incoherent speech, this does not mean that he has a minor stroke: at least 4-5 of the symptoms described above must be observed. Do not forget about the most effective diagnostic methods: what could be simpler than smiling or raising your hands up - but not for a victim of a mini-stroke. The results of these two exercises will be enough to call an ambulance and speed up competent treatment.
Treatment of heart diseases of any complexity is carried out at the Yusupov Hospital: top-class specialists work here, only modern methods of examining and restoring patients after illnesses are used.
Other treatments
Many people with vascular pathology lead a sedentary lifestyle, but it is the lack of activity that affects the condition of the blood vessels. The patient, immediately after a mini-stroke, is recommended to exercise daily for 5 to 10 minutes. They start with simple exercises - raising arms and legs, rotating the body, bending to the sides. In the future, the complex becomes more complicated, and the duration of classes increases.
If you feel better, walking is recommended - 30 minutes daily or 3-5 hours a week. Easy running and swimming are shown.
The rehabilitation program includes physiotherapeutic treatment:
- electrophoresis,
- darsonval,
- electrosleep,
- manitotherapy.
Aeroionization of the facial and collar zones has a good effect. To raise muscle tone, thermal procedures are used - paraffin wraps, therapeutic mud, ozokerite applications. A combination of thermal effects and electrical procedures (galvanization, ultrasound) is effective.
Restoring emotional health is an important part of rehabilitation efforts. If a person has a speech disorder, sessions with a speech therapist will help. The psychotherapist will identify hidden problems and set you up for successful treatment.
A person who regularly faces stressful situations should learn relaxation techniques - breathing exercises, auto-training. It is important to get a good night's sleep - at least 7-8 hours. Annual vacation and weekends are best used for active recreation.