Astrocytoma (or glioma) is a brain tumor, the basis for the development of which are special cells - astrocytes. This disease can affect people of all ages and develop in almost any part of the central nervous system (from the optic nerve to the cerebellum). And since more than 50% of such neoplasms have signs of malignancy, it is very important to diagnose the pathology in time and begin its treatment.
To have a more detailed understanding of this disease, we need a short excursion into human anatomy.
- What does an MRI show?
Brain astrocytomas: structure
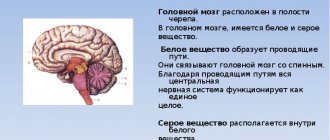
The nervous system is one of the most complex and poorly understood parts of our body. Even with modern technologies, it has not yet been possible to completely determine the principle of the brain. However, scientists still achieved some results.
In addition to the main cells that are responsible for transmitting and storing information (neurons), there are also auxiliary cells, the totality of which is called “neuroglia”. It makes up approximately 35-45% of the volume of the entire CNS (central nervous system) and performs supporting, trophic (provides nutrition), secretory, and protective functions. In other words, this tissue creates favorable conditions for neurons so that they can generate and transmit nerve impulses, thanks to which our body functions.
Astrocytes are star-shaped cells with numerous processes that are part of neuroglia. They support and nourish neurons, and can also take over their functions, for example, if nerve tissue is damaged during a stroke. This is a rather important link in the nervous tissue, and when a tumor develops from them, the functioning of the entire central nervous system is disrupted. We will talk about how and why this happens below.
Brain astrocytoma: causes
A proven cause for the appearance of tumor cells has not yet been found. There are a number of theories, but they remain unconfirmed. At the moment, only the presence of certain risk factors has been proven that increase the chance of developing this disease. These include:
- Hereditary predisposition to cancer pathology.
- Oncoviruses. They cause another disease, but their presence in the body can trigger the formation of a tumor (hepatitis B virus, human papillomas, etc.).
- Radioactive exposure.
- Advanced age.
- Exposure to harmful chemicals.
Brain astrocytoma: classification
There are several stages in the development of this pathological process. Depending on their stage, brain astrocytomas have a number of features. As you move from one type to another, the degree of its malignancy increases.
Pilocytic astrocytoma
This is the least aggressive tumor that rarely spreads to surrounding tissue. This neoplasm is characterized by slow growth, but can reach quite large sizes. It has clear boundaries and a uniform structure (a sign of good quality). Children most often suffer from this pathology. It responds well to treatment through surgery, after which there is a high probability of complete recovery.
Astrocytoma in children
Fibrillary astrocytoma
The degree of malignancy of this neoplasm is slightly higher than that of pilocytic astrocytoma. This tumor is still homogeneous and does not contain any inclusions. However, its outlines cease to be smooth (the first sign of degeneration). Tumor cells divide slowly, so this pathology can remain undiagnosed for a long time and reach large sizes. It can also be removed surgically, but the risk of relapse here is much higher than in the previous stage.
Aplastic astrocytoma
The third stage is characterized by rapid tumor growth. The boundaries of the pathological focus are uneven, the structure is already heterogeneous. Such an astrocytoma is no longer an isolated formation; it grows into surrounding tissues and causes irreparable damage to the brain. Most often, middle-aged men are susceptible to this disease. Unfortunately, the success rate after surgery is not high.
Glioblastoma
The last stage of development of brain astrocytoma. For unknown reasons, this disease is more common in the male population. The tumor quickly increases in size and grows into the surrounding tissue. The contours of such a formation are unclear, the structure has many inclusions. It is practically not amenable to surgical therapy. Treatment for this astrocytoma is most often done with radiation therapy or chemotherapy.
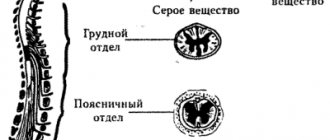
General information
Astrocytoma is considered the most common type of glial tumor. Almost half of all neoplasms of this type are represented by pathologies that arise due to the degeneration of stellate cells. Astrocytoma can develop rapidly at any age, regardless of gender and social status, as well as region of residence (it is equally common in both developed and third world countries). However, doctors note that most often neoplasms of this origin are presented in men aged 20 to 50 years. In addition, astrocytoma is usually localized in the white matter of the hemispheres in adults, and in the cerebellum in children. At the same time, in young patients, along with other characteristic signs of a tumor, lesions of the optic nerve appear, since the tumor at the same time penetrates the brain stem. This manifestation of pathology can also occur in the early stages of the disease.
What is cancer and why does it occur? October 30, 20203147 50
Brain astrocytoma: symptoms
Complaints from patients with this pathology are varied and nonspecific. They largely depend on the location of the tumor, its size and degree of development. With a large lesion, intracranial pressure increases and cerebral symptoms occur. These include:
- Bursting headaches.
- Vomiting that does not bring relief.
- Decreased memory and performance.
- Cramps.
Bursting headaches
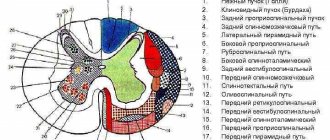
Focal symptoms of astrocytoma are associated with destruction or compression of areas of brain tissue near the tumor. Patients' complaints will be related to the extent to which changes have occurred. For example, when the temporal region is damaged, speech is impaired and memory decreases, the cerebellum suffers from balance, the frontal lobe causes mood and even personality changes, etc.
Prevention
To avoid complications and tumor recurrence, oncologists advise patients to adhere to the following recommendations after removal of an astrocytoma:
- Give up bad habits (alcohol, smoking).
- Lead an active lifestyle (will help restore the body, normalize hormonal balance and strengthen the immune system).
- Adequate rest (a person should sleep at least 6–7 hours a day).
- Proper nutrition (exclude heavy, fatty, junk foods from the diet).
Thus, spinal cord astrocytoma is a dangerous cancer that leads to serious consequences. If the pathology is identified in time and comprehensive treatment is started, the prognosis will be favorable. In other cases, it all depends on your general health and the stage of the cancer. By following your doctor's recommendations, you will be able to reduce the risk of tumor recurrence and improve your health.
Brain astrocytoma: diagnosis
In order to suspect and identify such a pathology, it is necessary to carefully examine the patient. The first step is collecting anamnesis (when the first symptoms appeared, how quickly they progressed, etc.). Next, a detailed examination by a neurologist is required. The specialist will check your reflexes and conduct tests to evaluate your brain function.
Well, the next stage is instrumental diagnostics. It will help to definitively establish a diagnosis and begin treatment immediately. The most popular examination methods for this pathology are CT and magnetic resonance imaging.
What does an MRI show?
This study is the gold standard for diagnosing cerebral astrocytoma. The procedure is very informative thanks to the ability of modern tomographs to perform layer-by-layer scanning of the brain in various planes. As a result of such a study, it is possible to examine in detail the changes in the selected area in 3D mode, as well as to bring a certain area closer or further, if there is such a need.
MRI of the brain for astrocytoma
During MRI of the brain, the skin remains intact and the patient does not experience any discomfort. All that is required of the person is to remove metal objects and remain motionless for the duration of the examination. The magnetic waves generated by the tomograph are absolutely safe for the human body, unlike the X-ray radiation used in CT. Thanks to this, the procedure can be repeated many times, for example, to determine the degree of tumor progression or to evaluate the results of treatment for astrocytoma.
The study does not last long (on average 15-30 minutes). After this, patients are given the results and a specialist’s report, which describes all the changes recorded during the tomography.
Literature
- B.V. Gaidar, T.E. Rameshvili, G.E. Trufanov, V.E. Parfenov, Radiation diagnostics of tumors of the brain and spinal cord - St. Petersburg: FOLIANT Publishing House LLC, 2006-336p.
- V.N. Kornienko and I.N. Pronin Diagnostic neuroradiology Moscow 2009 0-462.
- Abdullah ND, Mathews VP (1999) Contrast issues in brain tumor imaging. Neuroimaging Clin North Am 9(4):733–749 Abul-kasim K,
- Thurnher MM, Mckeever P et-al. Intradural spinal tumors: current classification and MRI features. Neuroradiology. - 2008;50 (4): 301-14.
- Agrawal V, Ludwig N, Agrawal A et al. Intraosseous intracranial meningioma. AJNR Am J Neuroradiol. 2007;28(2):314-5
- Presentation “Positron emission tomography in neurology and neuro-oncology” INSTITUTE OF THE HUMAN BRAIN named after. N.P. Bekhtereva RAS author E.S. Malakhova.
Brain astrocytoma: treatment
The choice of therapy for this pathology depends on the location of the tumor, its size and degree of malignancy. The main treatment method for astrocytoma currently is surgery. The purpose of the operation is to remove the tumor, if possible without damaging the surrounding brain tissue. However, if the neoplasm grows into neighboring areas, this is not possible. In this case, only part of the pathological focus is removed to relieve symptoms. But complete recovery does not occur in such situations.
Radiation therapy is also an important treatment for astrocytoma. It is based on the use of X-ray waves to damage tumor cells at the DNA level. As a result, they lose the ability to divide and die.
Another way to combat cancer is chemotherapy. To slow down the progression of the disease, drugs that have a cytotoxic effect are used (they trigger destruction processes inside the malignant cell).
Drugs with cytotoxic effects
Signs of increasing degree of anaplasia
The appearance of perifocal edema, an increase in size, and the manifestation of a mass effect characterize an increase in the degree of malignancy of the tumor and its degeneration into anaplastic astrocytoma. With increasing malignancy, the tumor increases the cellularity of its stroma, which leads to diffusion limitation reflected in DWI and ADC maps.
The first study reveals an area of diffuse damage in the temporo-occipital region on the right (arrowheads in Fig. 187), as well as limited diffusion in the affected area (arrow in Fig. 188). There are no hemorrhages in the tumor stroma (Fig. 189).
A study performed 2.5 months later revealed an increase in tumor volume (arrow heads in Fig. 190), an increase in the intensity of the MR signal on DWI (arrow heads in Fig. 191), areas of blood saturation (arrow in Fig. 192), and the appearance of areas of contrast and strengthening of existing ones (arrowheads in Fig. 192).
Brain astrocytoma: prognosis and consequences
Unfortunately, brain astrocytoma often leads to negative consequences. The lifespan of the first stage, as a rule, does not exceed 10 years. In the second, survival may decrease to 5-6 years, in the third - to 2-3. Once diagnosed with glioblastoma, a person rarely survives the one-year mark.
Pathology entails many negative consequences, which is not surprising. The disease itself is quite serious, and the methods for its treatment have their own characteristics. Possible complications include:
- Loss of vision.
- Inability to move independently.
- Speech impairment.
- Change in taste.
- Decreased sense of touch, etc.
The disease is very serious, therefore, when diagnosing astrocytoma of the brain, one should not delay treatment. The length and quality of future life depends on this.
Contrast enhancement
There may be minimal contrast or its complete absence, which indicates a preserved BBB, but this does not at all mean that this formation is benign, or characterizes this process as non-tumor growth.
After intravenous contrast enhancement, there is no accumulation of the contrast agent (Fig. 177-179).
In cystic astrocytomas there is also no accumulation of contrast agent after contrast enhancement (Fig. 180-182).
The appearance of areas with contrast enhancement characterizes an increase in the degree of anaplasia of the contrast-enhanced areas [2].
Zones of increased MR signal on T1 (arrowheads in Fig. 183-185) indicate a local violation of the integrity of the BBB and an increase in cellular atypia.