Materials and methods
The study included 109 patients with MS (49 men, 60 women; mean age - 33 years; range - 17-54): 51 with secondary progressive course, 19 with primary progressive course, 8 with progressive-recurrent course and 31 with relapsing course. remitting course. The EDSS index value before transplantation ranged from 1.5 to 8.0 points (the average was 5.0 points). The follow-up duration averaged 19 months (range 6 to 108 months). Disease activity was determined by neurological examination and magnetic resonance imaging. Patients underwent the following types of HDT+AuSCT: — Early transplantation
was performed at the onset of the disease in the presence of unfavorable prognostic factors regarding chemoresistance or the possibility of severe disability of the patient.
— Staged transplantation
was carried out when the disease was beyond the control of traditional treatment methods and the formation of secondary chemoresistance.
— Salvage transplantation
was carried out in an advanced stage of the disease with high activity of the immunopathological process and rapid progression of the patient’s disability. Thirty-two patients underwent early transplantation (EDSS 1.5-3.0); 70 patients received staged transplantation (EDSS 3.5-6.5) and 7 patients received salvage transplantation (EDSS 7.0-8.0).
Clinical and quality of life response assessments were performed pretransplant, at hospital discharge, 3, 6, 9, and 12 months posttransplant, then every 6 months for the first 4 years and annually thereafter. The study of neurological status included determination of the severity of neurological deficit on the EDSS scale and magnetic resonance imaging. The quality of life of patients 16 www.ctt-journal.com 2008;1(2) was assessed using the FACT-BMT (functional assessment of patients after bone marrow transplantation) and FAMS (functional assessment of patients with multiple sclerosis) questionnaires. Clinical improvement was defined as a decrease in the severity of neurological symptoms by at least 0.5 points on the EDSS scale compared to baseline, provided that this improvement was confirmed at the next visit 6 months later. Any increase in the severity of neurological symptoms according to the EDSS scale was considered disease progression. Relapse was defined as the appearance of new symptoms or worsening of previous symptoms for at least 24 hours in the absence of fever in a patient who had been stable for the previous 4 weeks. The response related to quality of life was characterized as minimal, moderate, good or maximum. To determine the response associated with quality of life, differences in the value of the integral indicator of quality of life before transplantation and at different periods of time after it were calculated.
Causes of the appearance and development of multiple sclerosis
The main source of the development of pathology are numerous viruses - rubella, mumps, herpes, measles, rabies and a number of others. Penetrating into nerve cells, they live in them for years, destroying both the cells themselves and myelin. The disease develops as follows.
- Destroyed tissues are gradually replaced by a prion, a foreign protein that plays the role of a powerful antigen.
- The human immune system responds to its appearance and spread with powerful autoimmune aggression - the production of antibodies occurs.
- The latter are directed to destroy the white matter of nerve fibers, perceiving it as a foreign protein.
As a result, the body's immune system gradually destroys the nervous system. During the development of the pathology, several parts of it are damaged at once: the membrane is gradually destroyed and, during demyelination, lesions are formed - the so-called plaques of multiple sclerosis. Since the lesions are diffuse in nature, sclerosis is called multiple sclerosis. The word “sclerosis” itself in this context means “scar” - these are the same sporadically spreading scars-plaques (areas of connective tissue) that form in place of destroyed nerve tissue. The size of the formations can reach several centimeters or more (if they merge during the course of the disease). Active lesions that are in the process of formation are called acute.
results
All 79 patients with a follow-up period of ≥9 months showed clinical improvement or stabilization in the course of the disease. There were no deaths or severe uncontrolled side effects reported during the transplantation. 6 months after transplantation, the distribution of patients according to clinical response was as follows: improvement - 42 (53%) patients, stabilization - 37 (47%) patients. Among the patients with improvement, 20 had a secondary progressive course, 7 had a primary progressive course, 4 had a progressive-recurrent course, and 11 had a relapsing-remitting course. In this group, 25 patients underwent staged transplantation, 15 – early and 2 – salvage transplantation. Of the 37 patients in whom disease stabilization was recorded, 19 had a secondary progressive course, 8 had a primary progressive course, 2 had a progressive-recurrent course, and 8 had a relapsing-remitting course. In this group, 23 patients underwent staged transplantation, 9 – early and 5 – salvage transplantation.
During longer follow-up periods, improvement remained in 40 patients (50.6%), and stabilization in 34 (43.1%). One patient after 6 months and two patients after 18 months of stabilization experienced an increase in the disability index. In two patients, disease progression occurred after 12 and 30 months of clinical improvement. According to MRI, all patients without disease progression after transplantation had no active or new lesions. Overall, 6-year progression-free survival after UDT+AuSCT was 72%. Patients who showed no signs of disease progression did not receive immunomodulatory or immunosuppressive therapy after transplantation. Quality of life monitoring was carried out in 44 patients included in the study. In 40 of them, improvement in quality of life indicators was observed 6 months after transplantation. Improvement in quality of life parameters was established using questionnaires – FACT-BMT and FAMS. 1 year after UDT+AuSCT, the following distribution of patients was recorded in accordance with the degree of response associated with quality of life: 3 patients had a maximum response (more than 75% improvement in the integral indicator of quality of life compared to the baseline); 12 patients had a good response (improvement by 50-75%); 11 patients had a moderate response (25-50%); in 13 there was a minimal response (improvement of less than 25%) and in 5 patients there was no response related to quality of life. It should be noted that patients with a longer follow-up period showed further improvement in quality of life indicators. The article presents a classification of types of transplantation for multiple sclerosis, based on the concept of VDT + HSCT for autoimmune diseases.
Multiple sclerosis
The first description of the disease was compiled by neurologist Jean Martin Shirko (France) in 1868. Disseminated encephalomyelitis (this is the scientific name of this disease) is an autoimmune progressive chronic disease of the nervous system, the course of which is accompanied by gradual damage to the myelin sheath of nerve fibers of the brain and spinal cord. The fibers connect the centers of the brain through electrical impulses, the speed of which is accelerated by myelin, an electrolyzing white substance of lipid-protein origin. In addition to this function, the sheath also performs another, no less important one - myelin insulates the nerve processes from each other.
Treatment of MS with stem cells in our clinic
One of the most effective methods of combating this insidious disease is treating multiple sclerosis with stem cells. It is this progressive and effective method of replacement therapy that is offered today in leading clinics in St. Petersburg. It provides:
- restoration of myelin, and with it the normal speed of transmission of nerve impulses;
- regeneration of brain and spinal cord cells in areas of nerve tissue replaced by connective scar tissue;
- normalization of the activity of the immune system with the cessation of autoimmune “attacks” on its part on the nervous system of the body.
At an early stage of disease development, MS can be cured due to the powerful regenerative potential of stem cells. The method of treating multiple sclerosis with stem cells is characterized by achieving high results: in each of the cases of therapeutic intervention, it provides stable remission. As a result of the therapeutic procedures, the clinic’s patients regain motor skills, the ability to fully care for themselves, move independently, in other words, the ability to live a full life.
Description and benefits
Arthrex Angel uses the patient's own biological material to prepare the concentrate in a closed, sterile, disposable system. It is a fully automated system that uses 3 Sensor Technology (3ST) to accurately dispense blood or bone marrow components into PRP/BMC (Platelet Rich Plasma), PPP (Poor Plasma) and RBC (Red Blood Cells) into sterile containers. 3ST technology is unique and allows you to achieve a concentration 18 times higher than the original one.
The main advantage of the system is that the user can set the desired concentration of various elements in the resulting useful product (PRP, BMC or PRF/BMC gel) by changing the centrifugation parameters. This allows you to control the concentration of platelets, leukocytes and red blood cells, while obtaining the desired proportion of elements in the plasma. This is especially important, since for each type of pathology the most effective is a particular concentration of certain elements in the final product.
Multiple sclerosis - clinical manifestations
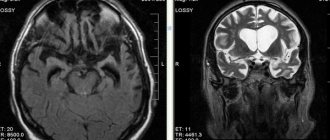
In the photo: Plaques - foci of demyelination
Clinical manifestations of MS are a direct consequence of focal lesions in parts of the brain.
The symptoms of multiple sclerosis are complex and varied. Among the most common characteristic manifestations, we name the following.
- Disorders of the motor system associated with damage to the cerebellum - the patient experiences staggering when walking, awkwardness in movements occurs, coordination is impaired, and muscle tone in the arms increases. In some cases, paresis occurs and paralysis occurs.
- Visual impairment - possible disturbance of the movement of the eyeball, the appearance of a “veil” in front of the eye or a black dot in the center of the visual field, while decreased vision (up to its loss) is typical for one eye.
- Dysfunction of the pelvic organs - urinary incontinence.
- Decreased taste sensitivity.
- Damage to the facial nerve with weakening of the muscles on one side of the face.
- Mental disorders - neurosis-like conditions, asthenic syndrome, depression, etc.
- Rapid onset of fatigue, fatigue even after minor physical and mental stress.
Multiple sclerosis
- a very “insidious” disease: after the first manifestations appear, the symptoms may disappear for quite a long period of time (even for 10 - 15 years), but subsequently, if the disease is not treated, it will certainly make itself felt in more severe manifestations. In addition, an exacerbation of the disease can be triggered by overheating and hypothermia, ARVI and other diseases, and neuro-emotional overload.
Multiple sclerosis by severity
- Mild type: relapsing-remitting course of MS - exacerbations are rare, periods of remission are long.
- The course is moderate in severity - remitting-progressive.
- Severe, progressive course (can be primary or secondary).
Multiple sclerosis by shape
The form of multiple sclerosis is determined depending on the prevailing symptoms. There are spinal, cerebral, ocular, hyperkinetic, and atypical forms of MS.
Groups and risk factors
Regions with a high risk of MS are highlighted in dark blue, regions with a likely high risk are highlighted in red.
Much earlier, long before the advent of technology for treating multiple sclerosis with stem cells, it was believed that the main risk group was women aged 20 to 40 years. The modern collective portrait of patients is very heterogeneous: doctors note a significant increase in cases of the disease among men and women over 40 years of age. At the same time, men most often experience an unfavorable progressive form of the disease. Multiple sclerosis is much more common today among Europeans - residents of the northern regions (Scandinavia, North-West Russia, Belarus). Thus, the region of residence is now recognized as one of the risk factors that determine the possibility of multiple sclerosis. In addition, a number of other main factors include:
- vascular diseases;
- autoimmune diseases;
- disturbed psycho-emotional state;
- infectious and allergic diseases;
- genetic predisposition (changes in enzyme parameters, T-suppressor deficiency).
Treatment of multiple sclerosis
Etiotropic therapy for MS, i.e. Treatment aimed at eliminating the specific cause of the disease is not practiced due to the impossibility of identifying its specific pathogen. As a result, pathogenetic therapy is used, the main objectives of which are:
- stopping the exacerbation of the disease with an impact on the foci of autoimmune inflammation and simultaneous activation of compensatory and adaptive mechanisms;
- preventing and reducing the severity of exacerbations;
- symptomatic therapy to eliminate symptoms that negatively affect the patient’s ability to lead a normal lifestyle.
During the treatment of multiple sclerosis, plasmapheresis, glucocorticoids, Copaxone, adrenocorticotropic hormone, biostimulants, B vitamins and other drugs are used.