Persistent and long-term diabetes leads to damage to almost all vital human organs, including disruption of nerve nutrition (oxygen starvation) of the peripheral nervous system, both somatic and autonomic.
Diabetic polyneuropathy (neuropathy) occurs in more than 50% of patients with diabetes. It affects diabetics with the first and second types of the disease equally. Most often (40–65%), the complication makes itself felt after 15–25 years from the onset of the underlying disease, but cases of its earlier manifestation cannot be excluded.
Polyneuropathy
Polyneuropathy (polyneuropathy is also used as a variant of the name) is a group of pathologies in which peripheral nerves, their roots and plexuses are exposed to multiple lesions.
This disease is a severe neurological disorder, manifested by weakness and atrophy of the muscles of the distal legs or arms, decreased tendon reflexes, changes in sensitivity, and the development of autonomic disorders. Most often, diseases of the peripheral nervous system affect older people. And the most common form is diabetic neuropathy.
Classification
Based on the type of manifestations and localization of symptoms, the following forms of diabetic polyneuropathies are distinguished:
- Proximal symmetrical polyneuropathy (amyotrophy).
- Asymmetrical proximal neuropathy of large nerves (usually femoral, sciatic or median).
- Neuropathies of the cranial nerves.
- Asymptomatic polyneuropathies.
- Distal types of polyneuropathy.
Distal polyneuropathy is the most common type of diabetic polyneuropathy. It accounts for more than 70% of all types of this disease. The word distal indicates damage to parts of the extremities remote from the body (hands, feet). The lower extremities are more quickly affected. Depending on the nature of the lesion, the following forms are distinguished:
- Sensory.
- Motor.
- Vegetative.
- Mixed (sensorimotor, motor-sensory-vegetative, sensory-vegetative).
Causes of development and types of disease
Polyneuropathy can appear for various reasons, and it is important to determine them, since they affect the course of treatment. By the way, there is also idiopathic polyneuropathy - then the cause remains unknown. In other cases it could be:
- Diabetes mellitus, as a result of which the functioning of blood vessels is disrupted, affecting the nutrition of the nerves and the condition of the myelin sheath of nerve fibers. In diabetes, polyneuropathy of the legs most often occurs.
- Severe lack of B vitamins, which play an important role in the functioning of the nervous system.
- Exposure to the body of harmful substances that cause several types of polyneuropathies: toxic (heavy metal poisoning, chemotherapy), alcoholic (alcohol abuse), medicinal (drug abuse).
- The presence of infections and viruses in the body (HIV, borreliosis, etc.).
- Chronic diseases (autoimmune, renal and liver failure, thyroid dysfunction), oncology.
- Hereditary predisposition.
Polyneuropathy of the upper extremities can also develop as a result of professional activities.
The time of development of the disease varies. Sometimes it takes several years, and in some cases it can occur in a few weeks. Based on this, it is divided into:
- acute (less than 4 weeks), usually caused by Guillain-Barré syndrome;
- subacute (up to 8 weeks);
- chronic (more than 8 weeks).
There is also a classification based on how polyneuropathy of the extremities manifests itself:
- sensory - the sensitivity of the affected limbs is impaired (numbness, tingling, burning, chilliness are felt, shooting pains appear);
- motor - muscle weakness occurs, leading to muscle atrophy;
- motor-sensory - first of all, motor disorders become noticeable in the patient;
- sensory-motor - changes in sensitivity predominate.
Causes of neuropathy of the lower extremities
The development of the disease may be associated with the following factors:
- long-term exposure to toxic substances (drugs, alcohol, arsenic, lead, mercury, etc.);
- metabolic disorders (diabetes mellitus, thyroid dysfunction, chronic renal failure);
- long-term hypovitaminosis;
- injuries;
- taking certain medications;
- infections (chickenpox, diphtheria, mumps, HIV infection);
- autoimmune diseases (for example, Guillain-Baré syndrome);
- burdened by heredity (genetically determined pathologies, for example, Charcot-Marie-Tooth amyotrophy).
Symptoms of polyneuropathy
The symptoms of the disease are varied, and the clinical picture depends on in which nerve fibers the pathological process arose. They can appear:
- changes in sensitivity - from sensations of numbness, goosebumps, tingling and burning to the complete disappearance of sensitivity or, conversely, hyperesthesia of the skin;
- disorder of motor functions - difficulties in moving the arms or legs against the background of muscle atrophy (tremor, difficulty walking up the stairs and performing habitual movements with the hands);
- reaction of the autonomic system - surges in blood pressure, heart rhythm disturbances, constipation or indigestion, severe pain of an unknown nature, increased sweating, sexual problems, swelling and slow healing of wounds.
The severity of the symptoms depends on the stage of polyneuropathy, as well as the individual characteristics of the patient.
Preventive measures
To prevent the disease it is necessary:
- Constantly monitor sugar levels in the body;
- systematically measure blood pressure;
- get rid of bad habits;
- to live an active lifestyle. It is advisable to walk for half an hour and do 15-minute exercises. Physical therapy and going to the gym several times a week will also bring tangible benefits;
- maintain foot hygiene, if possible, do not walk without shoes, treat any skin lesions that appear;
- undergo an annual examination for the presence of pathological changes in the nervous system.
Timely diagnosis of diabetic polyneuropathy and effective treatment lead to complete relief from the disease.
Diagnosis of the disease
Polyneuropathy is the responsibility of a neurologist, and you should make an appointment with him if similar symptoms appear. After studying the medical history and listening to complaints, the specialist will assess the neurological status and prescribe an examination.
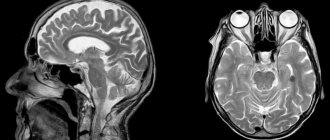
The main instrumental method for establishing a diagnosis is ENMG (electroneuromyography), with which you can not only confirm nerve damage, but also find out the nature of the damage. If this is not enough, ultrasound, contrast MRI and nerve biopsy are used. To clarify the diagnosis and determine the causes, one cannot do without blood tests: general, biochemical and to determine the presence of infections, vitamin levels, as well as ultrasound, CT and various endoscopies for general somatic examination. If hereditary neuropathy is suspected, a molecular genetic study is performed.
Features of treatment of neuropathy of the lower extremities
Identification of the provoking factor (endocrine disorders, infections, injuries, etc.) is the basis for the development of therapy. The latter is aimed at eliminating the negative impact of the detected disease on the nerve fibers.
How to treat lower extremity neuropathy itself? Treatment of this disease is complex and includes:
- drug therapy aimed at improving the conduction of impulses along nerve fibers, muscle relaxation, pain relief, replenishing vitamin deficiencies, getting rid of toxins, etc.;
- physical therapy (to maintain muscle tone);
- physiotherapy (manual therapy, laser therapy, electrical stimulation, vacuum therapy).
More information about the treatment of the disease can be found on the website of the CDC "IntegraMed" (formerly "NDC").
Treatment and prognosis of polyneuropathy
A patient who has been diagnosed with this condition requires comprehensive, individually tailored long-term treatment. But the basic principles are:
- treatment that eliminates or reduces the effect of harmful factors;
- treatment selected after determining the mechanisms that caused disruption of the peripheral nerves;
- symptomatic (treatment of autonomic disorders, pain relief).
Various forms of the disease are treated by a neurologist, but sometimes other specialists (endocrinologists, psychotherapists, etc.) may be involved. For example, with diabetic polyneuropathy, it is important to control glucose levels and adhere to the endocrinologist’s prescriptions and take prescribed medications. If the disease is of toxic origin, it is important to prevent harmful substances from entering the body, and if there is a deficiency of vitamins, therapy that restores their deficiency is used. Separate treatment programs exist for autoimmune types. But in all cases, drugs are used for polyneuropathy, providing symptomatic treatment (anaesthetics, analgesics, anticonvulsants, antidepressants). After undergoing therapy, a rehabilitation course is usually required, including therapeutic massage, which helps improve muscle tone and restore motor functions of the arms and legs. Physiotherapy (improves microcirculation) and ergotherapy (development of a specific algorithm of actions for daily movements) also help. This group of rehabilitation methods includes vitamin and diet therapy, as well as work with a psychologist.
Sequence of treatment procedures
Treatment of polyneuropathy must be supervised by a doctor, who in each specific case develops an individual scheme for combating the pathology.
Treatment of pathology has three main goals:
- Normalize blood glucose levels.
- Ease pain syndrome.
- Restore damaged nerve fibers.
Restoration of nerve fibers is the main goal of treatment of diabetic polyneuropathy
Sugar balance is normalized using the following groups of drugs:
- promoting the production of insulin by the pancreas: Nateglinide, Gliclazide, Liquidon;
- increasing the sensitivity of peripheral tissues to insulin: Ciglitazone, Englitazone, Metformin;
- preventing the absorption of sugars in the intestines: Miglitol.
Restore nerve function and relieve pain by resorting to:
- to drugs that help normalize blood sugar levels and have antioxidant activity: Espa-lipon, Thioctacid, etc.;
- medications that stop the inflammatory processes of nerve tissue, restore nerve fibers and improve the passage of signals through them: Milgamm, B vitamins;
- relieving pain, inflammation and swelling of the nerves: Nimesulide, Indomethacin;
- a drug that can block the flow of pain impulses into the brain - Amitriptyline;
- anticonvulsants, which prevent convulsive muscle contractions and eliminate pain: Gabapentin, Pregabalin;
- synthetic opioids: Zaldiar and Oxycodone, which inhibit pain impulses, reducing sensitivity to pain and temperature changes;
- the antiarrhythmic drug Mexiletine, which helps block sodium channels, which causes disturbances in the transmission of pain impulses;
- local anesthetics: ointments and plasters Versatis, Ketoprofen, etc.
Almost all medications have contraindications and side effects, which makes self-medication impossible.
In addition to medication, treatment of diabetic polyneuropathy of the lower extremities is possible:
- warming up the extremities with a light massage and warm socks. It is prohibited to treat this pathology with a heating pad, hot baths or open fire;
- using orthopedic insoles that reduce the load on the feet;
- treating wounds with antiseptic agents;
- daily 10-minute exercises recommended by experts.
Frequently asked questions about polyneuropathy
What pain does polyneuropathy cause?
Pain varies in nature and can occur unexpectedly or be felt constantly. Mostly, patients experience itching, burning, coldness and chilliness; there are also manifestations of acute cutting and stabbing pain.
How to diagnose polyneuropathy yourself?
This is impossible to do, since only a doctor can differentiate the symptoms, and instrumental methods and laboratory tests are important for making a diagnosis.
How long to treat polyneuropathy?
Treatment of polyneuropathy is a long process under the constant supervision of a doctor.
Mechanism of occurrence
The exact mechanism of damage to nerve cells is unknown; it is assumed that the drug penetrates from the blood into the intercellular fluid, from there it diffuses into the cell, where it damages the protein tubulin and other proteins.
Each drug has its own “point of application” to tubulin: taxanes break up its microtubules, platinum derivatives denature it, vinca alkaloids are disassembled into components.
The process of protein damage by cytostatics in all cells is the same, its consequences are varied:
- degeneration of nerve processes - axonopathy;
- degenerative changes in neuron cell bodies—neuronopathy;
- destruction of the myelin sheath of the nerves - myelinopathy throughout or partially.
Clinical phenomenology of chronic renal failure
Symptoms of damage to the nerve process - axonopathy - manifest several weeks and even months later than damage to the neuron - neuronopathy.
Platinum derivatives predominantly cause sensory disturbances in the legs, which destabilizes the gait, does not give the foot a feeling of the floor, which is why the patient has to use his eyes to choose a place to place the foot. It is possible that a motor component may be associated with muscle spasms. After completion of chemotherapy, the manifestations of polyneuropathy decrease very slowly, perhaps even increasing over 3 months - a symptom of inertia.
Pactitaxel initiates sensory disturbances, usually “pins and needles” and numbness, more often in the legs than in the arms. The feeling of “burning” soles is typical, especially after high-dose chemotherapy. Motor disorders are as atypical as autonomic ones. Normalization may take up to a year.
Docetaxel affects sensory fibers, the frequency of symptoms increases with a total of 500 mg, but severe polyneuropathy is practically impossible. Every 5-6 patients develop asthenia - weakness.
Vinorelbine does not begin to ruin your life right away - after a month of weekly injections, the sensitivity of the fingers is often impaired, gastrointestinal motility decreases, which is manifested by constipation, but the most common complication is asthenia in six out of ten patients, when they complain of severe fatigue precisely from the treatment.
Oxaliplatin changes the sensitivity of the hands with tingling of the fingertips, and the disturbances appear very early - literally after the first dose, reaching a maximum on the 3rd day. Between administrations everything seems to return to normal, but in the next course it is repeated and more intensively. The peculiarity is that 3 months after chemotherapy, the symptoms of polyneuropathy are the brightest, then improvement begins, six months after chemotherapy, symptoms of impaired sensitivity in the legs come to the fore, and the hands are less bothersome.
Fluorouracil “hits” the brain, causing gait instability - cerebellar ataxia and spasmodic eye movements - nystagmus, and changes speech due to sluggishness of the tongue. High doses and multi-day infusions may be complicated by encephalopathy. The frequency and intensity of manifestations increases many times in the absence of an enzyme in the cells that destroys fluorouracil metabolites.
During administration, irinotecan
With all the variety of clinical manifestations of polyneuropathy after chemotherapy and the absence of a clear diagnostic algorithm, the neurological complication can be recognized in time, but it is absolutely impossible to predict its duration.