The scourge of the 21st century is stress. His faithful companions: anxiety, excitement, neuroses, panic attacks, somatic manifestations (urticaria, skin itching, allergic dermatitis, eczema), sleep disturbances. It would seem that there’s nothing wrong with it, just rest and everything will pass. But if it does not go away, gets worse and disrupts the usual rhythm of life, then you need to consult a doctor. During drug treatment, doctors often prescribe a prescription for the anxiolytic (tranquilizer) Atarax, which is allowed even for children over one year of age.
Stress is a very common problem
Composition of the medicine
The main active component - hydroxyzine - has a calming, anti-allergenic, analgesic, antispasmodic effect, and also increases concentration, improves attention and cognitive functions. If anxiety is pronounced, and chronic insomnia is also associated with it, then Atarax, or rather hydroxyzine, relieves anxiety, normalizes sleep, strengthening and increasing its duration, and reduces the frequency of awakenings at night. The drug is able to relax skeletal muscles, as well as smooth muscles. All this is due to the effect of the drug Atarax on certain areas of the subcortical zones of the brain.
The drug is absorbed into the gastrointestinal tract, after which it quickly enters the systemic circulation. That is why the effect of taking Atarax is noticeable within 15-30 minutes.
If you take Atarax for a long time, then addiction or dependence on the drug will not develop. This means that he does not have “withdrawal syndrome”.
Anti-anxiety effectiveness of Atarax
Sometimes anxiety is natural, adequate, and useful. Everyone feels anxious, restless or stressed in certain situations, especially if they have to do something unusual or prepare for it. For example, giving a speech in front of an audience or passing an exam. A person may feel anxious when walking down an unlit street at night, or when lost in a strange city. This type of anxiety is normal and even useful, as it prompts you to prepare a speech, study the material before an exam, and think about whether you really need to go out at night all alone. In other cases, anxiety is unnatural, pathological, inadequate, harmful. It becomes chronic, constant and begins to appear not only in stressful situations, but also for no apparent reason. Then anxiety not only does not help the person, but, on the contrary, begins to interfere with him in his daily activities. The line between a “normal” stress response and a pathological anxiety disorder is often quite blurred, and it is difficult for a person to know when to seek professional help. These subsyndromal anxiety disorders are the most difficult to diagnose and often remain untreated, while having an extremely negative impact on the quality of life of the patient and those around him. It is believed that treatment options should be considered when anxiety about everyday events is beyond the patient's control. The following disorders may also be a reason for prescribing therapy: nervousness, fussiness, impaired concentration, irritability, sleep disturbance, symptoms of autonomic dysfunction. The main approaches to the treatment of anxiety disorders are: • psychotherapy • pharmacotherapy For treatment purposes, you can use simple relaxation methods (muscle relaxation, calm breathing, distraction). Friendly and encouraging conversation also helps improve the condition. The main groups of drugs for the treatment of anxiety disorders: • Benzodiazepine tranquilizers • Antidepressants: – selective serotonin reuptake inhibitors, – tricyclic antidepressants • Neuroleptics • Non-benzodiazepine tranquilizers Benzodiazepines – quickly relieve sleep disorders and anxiety symptoms. Among the disadvantages of treatment with benzodiazepines, the following should be mentioned: “recoil” syndrome (rapid resumption or transient increase in symptoms after discontinuation of the drug), the risk of addiction and the formation of drug dependence, impaired cognitive functions (attention, concentration, memory), and impaired coordination. Therefore, drugs of the benzodiazepine group should not be taken for more than 2–4 weeks. Tricyclic antidepressants are powerful drugs that effectively relieve all anxiety and depressive symptoms (affecting both physical and mental manifestations of anxiety) and sleep disorders. Can be used for long-term treatment and prevention of anxiety. Tricyclic antidepressants have more pronounced side effects (dry mucous membranes, constipation, cardiovascular disorders, transient cognitive impairment). This worsens tolerability and increases the list of contraindications for their use in the treatment of anxiety, especially in patients with concomitant somatic diseases. Selective serotonin reuptake inhibitors are relatively safe, have a minimal range of side effects, are not addictive, and therefore can be used as long-term maintenance treatment. Their relative disadvantage is the long “waiting” period before the onset of the clinical effect of the drug (from 2 to 4 weeks). In addition, antidepressants in this group have side effects such as increased appetite and weight gain, nausea, loose stools, constipation, sweating, sleep disturbances, and sexual functions (libido and orgasm). In some cases, a positive effect in the treatment of anxiety is achieved with the use of antipsychotics. Typically, small doses of these drugs are used. However, when antipsychotics are prescribed, weakness, decreased blood pressure, menstrual irregularities, weight gain, colostrum secretion, and decreased libido may occur. Finally, international recommendations list another drug for the treatment of anxiety – hydroxyzine (Atarax). It is characterized by a rapid onset of effect, absence of addiction and drug dependence, does not impair cognitive functions, and has antipruritic and antiemetic effects. Hydroxyzine is neither a benzodiazepine nor a phenothiazine. The non-benzodiazepine anxiolytic Atarax (hydroxyzine) is a derivative of diphenylmetane, an antagonist of histamine H1 receptors. Hydroxyzine has been successfully used in a variety of areas of medicine: as a means of controlling tobacco smoking [1]; in pediatric dentistry [2]; for its intended purpose – for the treatment of anxiety neurosis (even in the era of the existence of such a nosological form) and for “mild” depression [3]; for behavioral and learning disorders in children [4]. Due to its antihistamine properties, hydroxyzine was used in allergology, to treat itching [5], and for urticaria pigmentosa (mastocytosis) in children [6]; in oncology [7]; in burn patients [8], in narcology [9] and in many other conditions. Recently, there has been interest among researchers in the use of hydroxyzine in patients with generalized anxiety disorder (GAD). The prevalence of this pathology and the associated burden of social consequences in the current scientific literature appear to be quite significant. According to one review [E.G. Starostina. Generalized anxiety disorder and anxiety symptoms in general medical practice. Rus. honey. magazine 2004; 12, 22 (222): 1277], with reference to numerous foreign works, “GAD is among the top ten diseases with the greatest temporary disability and according to this indicator is on the same level with ischemic heart disease, diabetes, joint diseases, peptic ulcer disease, and among mental disorders – with depression or even ahead of it.” In a double-blind, placebo-controlled study for the treatment of generalized anxiety disorder [10], the anxiolytic activity of Atarax at a dose of 50 mg (in 3 doses of 12.5 mg in the morning and afternoon plus 25 mg in the evening) was shown, which was manifested in a statistically significant, rapid and a significant reduction in anxiety symptoms already at the end of the 1st week of treatment, which persisted for another 1 week after cessation of treatment (n=110; course duration 4 weeks; Hamilton scale score - A). In this case, there was no phenomenon of “rebound” or return of anxiety. In another double-blind multicenter study [11], in which, along with placebo control, the benzodiazepine drug Bromazepam was also used, it was shown that hydroxyzine used for 3 months was statistically significantly different from placebo and was as effective as the comparison drug . Moreover, with benzodiazepine, side effects of severe drowsiness were observed twice as often as with hydroxyzine (n = 334; dose of hydroxyzine 50 mg/day in 3 divided doses; bromazepam - 6 mg/day in 3 divided doses; improvement on the Hamilton-A scale >50 %; p<0.03 at the end of the 6th week and p<0.001 - after 12 weeks; the number of patients who responded to treatment: 40% at the 6th and 60% at the 12th week, respectively). Another study [12] showed the effectiveness of Atarax (50 mg in 3 doses), comparable to that of the control buspirone (20 mg in 3 doses), with a statistically significant difference between Atarax and placebo on the 28th day of treatment (p <0.015) . There was no rebound phenomenon with abrupt withdrawal of both drugs (n=244; age 18–65 years). Another advantage of hydroxyzine is that, unlike benzodiazepines, it does not depress cognitive abilities [13] (triple crossover, double-blind clinical trial; comparing a single dose of 50 mg of hydroxyzine with a single dose of 2 mg of lorazepam and placebo; n = 9; healthy volunteers; 3-day interval before cross-over; assessment of cognitive functions 2-5 hours after taking comparator drugs). Some studies have shown a positive effect of hydroxyzine on cognitive function [14] (comparison with lorazepam; double-blind multicenter clinical trial; n = 30; GAD, Atarax 100 mg in 3 divided doses, lorazepam 4 mg in 3 divided doses; Beck score 28 -th day of treatment). Unlike lorazepam, with the same anxiolytic activity, hydroxyzine restored cognitive function to normal limits. Similar results were obtained in another, less evidence-based study - an open RCT [A.E. Bobrov et al. Journal neurol. and psychiatrist. them. S.S. Korsakov. 1988; 2] outpatients with GAD; (n=50). The course of treatment is 4 weeks, plus 2 weeks of follow-up. Features of Atarax - rapid onset of action, good tolerability, lack of dependence and depression of the central nervous system, make it an alternative drug to benzodiazepines in children and adolescents. In a study conducted at the Children's Psychiatry Center [15], Atarax was prescribed for various forms of mental illness in children and adolescents with symptoms of anxiety, irritability and insomnia-type sleep disorders, and its effectiveness was assessed. The study included 50 patients aged 5 to 18 years with various forms of mental illness, who were undergoing outpatient observation and treatment at the Children's Psychiatry Center. At the end of the 4th week of therapy, there was a decrease in the manifestations of anxiety and various fears noted earlier - falling asleep in the dark, staying at home in the absence of parents, fears of animals, noise of household appliances. In one case, a 5-year-old boy could stay at home with a nanny without his parents - a pronounced affective reaction was previously noted. In addition, all patients' sleep improved already in the second week of therapy, tearfulness, moodiness, and irritability were reduced. Simultaneously with the reduction of anxiety, the mood improved in 7 patients with a mixed anxious and depressive reaction caused by an adaptation disorder and with a mixed anxiety and depressive disorder, which was associated not with the direct antidepressant effect of Atarax, but with the comorbid dependence of anxiety and depression: anxiety was reduced - depression went away. Hydroxyzine (Atarax) has its obvious advantages over benzodiazepine anxiolytics in the treatment of anxiety disorders; it does not produce “rebound” phenomena, does not depress cognitive function and does not cause pathological dependence. References 1. Turle G. An investigation into the therapeutic action of hydroxyzine/Atarax in the treatment of nervous disorders and the control of tobacco–habit. Brit J Psychiat 1958; 104: 82 rub. 33. 2. Lang L. An evaluation of the efficacy of hydroxyzine (atarax–vistaril) in controlling the behavior of child patients. J–Dent–Child 1965; 32, 4: 253–8) 3.R.Middlefell, K.Edwards Hydroxyzine/Atarax in the relief of tension associated with anxiety neurosis and mild depressive states. Brit J Psychiat 1959; 105:792–4. 4. Segal L, Tansley A. A clinical trial with Hydroxyzine (Atarax) on a group of maladjusted educationally subnormal children.J Mental–Science; Br J Psychiat from 1963; 1957; 103:677–81. 5. Rhoades R, Leifer K, Cohan R, Wittig H. Suppression of histamine-induced pruritus by three antihistaminic drugs. J Allergy Clin Immunol, 1975 Mar.; 55, 3: 180–5. 6. Kettelhut B, Berkebile C, Bradley D, Metcalfe D. A double-blind, placebo-controlled, crossover trial of ketotifen versus hydroxyzine in the treatment of pediatric mastocytosis. J Allergy Clin Immunol 1989 May; 83, 5: 866–70) 7. Broder L, Lean N, Hilsenbeck S. A randomized blinded clinical trial comparing delta–9–tetrahydrocannabinol (THC) and hydroxizine (HZ) as antiemetics (AE) for cancer cancer (CT). PROC–AM–ASSOC–CANCER–RES; 1982; 23: 514. 8. Vitale M, Fields–Blache C, Luterman. A Severe itching in the patient with burns. J burn care & rehabilitation 1991; 12, 4: 330–3. 9. Kaim S, Klett C, B. Rothfeld. Treatment of the acute alcohol withdrawal state: a comparison of four drugs. Agressologie: revue internationale de physio-biologie et de pharmacologieappliquees aux effets de l'agression, 1968; 9, 2: 305–8. 10. Ferreri M, Hantouche T, M. Billardon. Interet de l'hydroxizynedans des troubles d'anxiete generalalisee: etude controlee en double aveugle versus placebo. L'encephale 1994; 20: 785–91. 11. Llorka P. et al. Efficiency and safety of hydroxysyne in the treatment of generalized anxiety disorder: a 3–month double–blind study. J Clin Psychiatry 2002; 63:1020–7. 12. Lader Scotto J. A multicenter double–blind comparison of hydroxizine, buspirone and placebo in patient with generalized anxiety disorder. Psychopharmacology 1998; 139:402–6. 13. De Brabander A, Deberdt W. Effect of hydroxizyne on attention and memory. Human Psychopharmacology 1990; 357–62. 14. Samuelian J, Billardon M, Guillou N. Retentissmentsur les functions cognitives de deuxtraitmentsanxiolitiques chez des patients souffrantd'anxietegeneralisee. L'encephale 1995; 21: 147 15. Rezakov A.A. Experience of using hydroxyzine (atarax) in children and adolescents. “PHARMIndex-Practik” issue 10; 2006, pp. 37–39
Indications
Indications for use of the drug are:
- relief of psychomotor agitation, tension, irritability in mental, neurological, somatic diseases;
- symptomatic treatment of withdrawal syndrome that occurs against the background of chronic alcoholism;
- anxiety;
- providing a sedative effect during premedication;
- therapy for itchy skin.
Why and why Atarax needs to be taken is determined by the attending physician. As a rule, taking Atarax is provoked by diagnosed skin diseases, which are accompanied by severe skin itching.
Contraindications
Contraindications to the use of the drug:
- pregnancy;
- lactation period;
- porphyria;
- intolerance or hypersensitivity to the components of the drug;
- high sensitivity to cetirizine, piperazine derivatives, as well as ethylenediamine or aminophylline;
- angle-closure glaucoma;
- impaired absorption of glucose and galactose;
- hereditary galactose intolerance.
Pregnant women should not use Atarax.
Atarax is used with caution in the following cases:
- myasthenia gravis;
- prostatic hyperplasia;
- difficulty defecating and urinating;
- dementia;
- increased intraocular pressure;
- predisposition to arrhythmia and seizures.
Atarax. We treat anxiety with tranquilizers. Lecture for doctors
Lecture for doctors “Strengthening the therapeutic effects of antidepressants.” The lecture for doctors is given by a psychiatrist, psychotherapist, doctor of the highest category, professor, doctor of medical sciences Drobizhev Mikhail Yurievich
The lecture covers the following issues:
- Anxiety
- Target N3 - moderately inhibit two types of neurons that implement anxiety
- Anvifen and Atarax as anti-anxiety drugs Anvifen - moderate anti-anxiety effect
- Atarax - weak anti-anxiety effect
- Main features of Atarax Weak anti-anxiety effect
- Characterized by drowsiness, cognitive functions do not improve
- Anyone who wants to treat mild anxiety and who has access to a regular prescription
ATARAX: instructions for use
Clinical and pharmacological group Tranquilizer (anxiolytic)
Active ingredient : hydroxyzine hydrochloride (hydroxyzine)
Release form, composition and packaging Tablets, white, oblong, film-coated, with a dividing transverse score on both sides.
1 tab. — hydroxyzine hydrochloride 25 mg
Excipients: microcrystalline cellulose (Avicel PH102), colloidal silicon anhydride (Aerosil 200), magnesium stearate, lactose monohydrate, Opadry Y-1-7000 (titanium dioxide, hydroxypropyl methylcellulose 2910 5cP, macrogol 400).
25 pcs. - blisters (1) - cardboard packs.
pharmachologic effect
A derivative of diphenylmethane, it has moderate anxiolytic activity; It also has a sedative, antiemetic, antihistamine and m-anticholinergic effect. Blocks central m-cholinergic receptors and histamine H1 receptors and inhibits the activity of certain subcortical zones. Does not cause mental dependence or addiction. The clinical effect occurs 15-30 minutes after taking the drug orally.
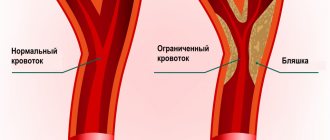
Has a positive effect on cognitive abilities, improves memory and attention. Relaxes skeletal and smooth muscles, has bronchodilator and analgesic effects, and a moderate inhibitory effect on gastric secretion. Hydroxyzine significantly reduces itching in patients with urticaria, eczema and dermatitis. With long-term use, there was no withdrawal syndrome or deterioration of cognitive functions. Polysomnography in patients with insomnia and anxiety clearly demonstrates an increase in sleep duration and a decrease in the frequency of night awakenings after a single or repeated dose of hydroxyzine at a dose of 50 mg. A decrease in muscle tension in patients with anxiety was noted when taking the drug at a dose of 50 mg 3 times a day.
Pharmacokinetics
Suction
Hydroxyzine is highly absorbed from the gastrointestinal tract. Cmax is observed 2 hours after taking the drug.
After a single dose of the drug in a single dose of 25 mg or 50 mg in adults, the plasma concentration is 30 ng/ml and 70 ng/ml, respectively.
Bioavailability when taken orally and intramuscularly is 80%.
Distribution
Hydroxyzine is more concentrated in tissues (particularly skin) than in plasma. The distribution coefficient is 7-16 l/kg.
Hydroxyzine penetrates the BBB and the placental barrier, concentrating more in the fetal tissues than in the mother's body. Metabolites are found in breast milk.
Metabolism and excretion
Hydroxyzine is metabolized in the liver. The main metabolite (45%) is cetirizine, which is a histamine H1 receptor blocker. The total clearance of hydroxyzine is 13 ml/min/kg. T1/2 in adults is 14 hours. Only 0.8% of hydroxyzine is excreted unchanged in the urine.
Pharmacokinetics in special clinical situations
In children, the total clearance is 4 times less than in adults, T1/2 in children aged 14 years is 11 hours, in children aged 1 year - 4 hours.
In elderly patients, T1/2 is 29 hours, the distribution coefficient is 22.5 l/kg.
In patients with impaired liver function, T1/2 increases to 37 hours, the concentration of metabolites in the blood serum is higher than in young patients with normal liver function. The antihistamine effect can last for 96 hours.
Indications for adults: for the relief of anxiety, psychomotor agitation, feelings of internal tension, increased irritability in neurological, mental (including generalized anxiety, adaptation disorders) and somatic diseases, chronic alcoholism; withdrawal syndrome in chronic alcoholism, accompanied by psychomotor agitation; as a sedative during premedication; skin itching (as symptomatic therapy).
Contraindications
porphyria; pregnancy; period of labor; lactation period (breastfeeding); hypersensitivity to the components of the drug; hypersensitivity to cetirizine and other piperazine derivatives, aminophylline or ethylenediamine. It is not recommended to prescribe Atarax tablets to patients with hereditary galactose intolerance, as well as impaired absorption of glucose and galactose, because The tablets contain lactose.
The drug should be prescribed with caution for myasthenia gravis, prostatic hyperplasia with clinical manifestations, difficulty urinating, constipation, increased intraocular pressure, dementia, and a tendency to seizures; with a predisposition to the development of arrhythmia; with simultaneous use of drugs that have arrhythmogenic effects; simultaneously with other CNS depressants or anticholinergics (dose reduction required). A reduction in the dose of the drug is required in patients with severe and moderate renal failure, with liver failure, and in elderly patients with decreased glomerular filtration.
Dosage
The drug is taken orally.
For the symptomatic treatment of itching in children aged 12 months to 6 years, the drug is prescribed in a daily dose of 1-2.5 mg/kg body weight in several doses; children over 6 years of age - at a dose of 1-2 mg/kg/day in several doses.
For premedication in children, the drug is prescribed at a dose of 1 mg/kg body weight 1 hour before surgery, and additionally the night before surgery.
For the symptomatic treatment of anxiety, adults are prescribed a dose of 25-100 mg/day in several doses during the day or at night. The average dose is 50 mg/day (12.5 mg in the morning, 12.5 mg in the afternoon and 25 mg at night). If necessary, the dose can be increased to 300 mg/day.
For the symptomatic treatment of itching, the initial dose is 25 mg; if necessary, the dose can be increased 4 times (25 mg 4 times a day).
The maximum single dose should not exceed 200 mg, the maximum daily dose is no more than 300 mg.
In elderly patients, the initial dose should be reduced by 2 times.
Patients with moderate to severe renal insufficiency, as well as hepatic insufficiency, require a dose reduction.
Side effects
Side effects associated with anticholinergic effects: rarely (mainly in elderly patients) - dry mouth, urinary retention, constipation, impaired accommodation.
From the central nervous system: drowsiness, general weakness (especially at the beginning of treatment), headache, dizziness. If weakness and drowsiness do not disappear after a few days from the start of therapy, the dose of the drug must be reduced. Very rarely (with significant overdose) - tremors, convulsions, disorientation.
From the cardiovascular system: arterial hypotension, tachycardia.
From the digestive system: nausea, changes in liver function tests.
Other: increased sweating, allergic reactions, fever, bronchospasm.
When using the drug in recommended doses, no clinically significant respiratory depression was observed. Involuntary motor activity (including very rare cases of tremors and convulsions), disorientation were observed with significant overdose.
Side effects observed when taking Atarax are usually mild, transient and disappear within a few days of starting treatment or after reducing the dose.
Overdose
Symptoms: increased anticholinergic effects, depression or paradoxical stimulation of the central nervous system, nausea, vomiting, involuntary motor activity, hallucinations, impaired consciousness, arrhythmia, arterial hypotension; rarely - tremors, convulsions, disorientation, which occur with a significant overdose.
Treatment: if spontaneous vomiting is absent, it is necessary to induce it artificially or perform gastric lavage. Carry out general measures aimed at maintaining the vital functions of the body, and monitor the patient until the symptoms of intoxication disappear in the next 24 hours.
If it is necessary to obtain a vasopressor effect, norepinephrine or metaramenol is prescribed. Epinephrine should not be used. There is no specific antidote. The use of hemodialysis is ineffective.
Drug interactions
Atarax potentiates the effect of drugs that depress the central nervous system, such as opioid analgesics, barbiturates, tranquilizers, hypnotics, ethanol (combinations require individual selection of drug doses).
Atarax, when used simultaneously, interferes with the pressor effect of epinephrine (adrenaline) and the anticonvulsant activity of phenytoin, and also interferes with the action of betahistine and cholinesterase blockers.
With simultaneous use, Atarax does not affect the activity of atropine, belladonna alkaloids, cardiac glycosides, antihypertensive drugs, histamine H2 receptor blockers.
Co-administration of Atarax with MAO inhibitors and anticholinergics should be avoided.
Hydroxyzine is an inhibitor of the CYP2D6 isoenzyme and, when used in high doses, may cause interactions with CYP2D6 substrates. Since hydroxyzine is metabolized in the liver, an increase in its concentration in the blood can be expected when co-administered with liver enzyme inhibitors.
special instructions
If allergy tests are necessary, Atarax should be discontinued 5 days before the test.
Patients taking Atarax should avoid drinking alcohol.
Impact on the ability to drive vehicles and machinery
Patients taking Atarax, if necessary to drive a car or operate machinery, should be warned that the drug may affect concentration and the speed of psychomotor reactions.
Pregnancy and lactation
Atarax is contraindicated for use during pregnancy and labor.
If it is necessary to use Atarax during lactation, breastfeeding should be stopped.
Use in childhood
For the symptomatic treatment of itching in children aged 12 months to 6 years, the drug is prescribed in a daily dose of 1-2.5 mg/kg body weight in several doses; children over 6 years of age - at a dose of 1-2 mg/kg/day in several doses.
For premedication in children, the drug is prescribed at a dose of 1 mg/kg body weight 1 hour before surgery, and additionally the night before surgery.
For impaired renal function
Patients with moderate to severe renal failure require a dose reduction.
For liver dysfunction
Patients with liver failure require a dose reduction.
Use in old age
A reduction in the dose of the drug is required in elderly patients with a decrease in glomerular filtration.
Conditions for dispensing from pharmacies
The drug is available with a prescription.
Storage conditions and periods
The drug should be stored out of reach of children, in a dry place at a temperature not exceeding 25°C. Shelf life: 5 years.
Side effects
Since Atarax is a drug that acts on the central nervous system, it can sometimes cause suppression of certain functions or paradoxical stimulation. Also, when taking it, negative reactions from the body may occur:
- From the cardiovascular system: blood pressure rarely decreases, heart rate increases.
- From the point of view: decreased clarity of vision, impaired accommodation.
- From the gastrointestinal tract: a feeling of dry mouth, rarely - vomiting, nausea, problems with intestinal motility and, as a result, constipation.
- From the immune system: hypersensitivity, rarely anaphylactic shock may develop.
- From the urinary system: urine retention is rarely possible.
- From the respiratory system: rarely - bronchospasm and suffocation.
- Neurological disorders: drowsiness, headache, insomnia, dizziness, rarely – convulsions.
- Mental disturbances are rare: agitation, disorientation, and hallucinations are possible.
- Skin: itching, rash, rarely - swelling.
- General disorders: weakness, fever, fatigue.
Atarax, tablets 25 mg, 25 pcs.
Manufacturer
USB Pharma S.A., Belgium
Compound
1 tablet: - hydroxyzine hydrochloride 25 mg
Excipients:
microcrystalline cellulose (Avicel PH102®),
colloidal silicon anhydride (Aerosil 200®),
magnesium stearate,
lactose monohydrate,
Opadry® Y-1-7000 (titanium dioxide, hydroxypropyl methylcellulose 2910 5cP, macrogol 400).
pharmachologic effect
Pharmgroup:
anxiolytic (tranquilizer).
Pharmaceutical action
:
A derivative of diphenylmethane, it has moderate anxiolytic activity; It also has a sedative, antiemetic, antihistamine and m-anticholinergic effect.
Blocks central m-cholinergic and H1-histamine receptors and inhibits the activity of certain subcortical zones. Does not cause mental dependence or addiction. The clinical effect occurs 15–30 minutes after ingestion of the tablets. Has a positive effect on cognitive abilities, improves memory and attention. Relaxes skeletal and smooth muscles, has bronchodilator and analgesic effects, and a moderate inhibitory effect on gastric secretion. Hydroxyzine significantly reduces itching in patients with urticaria, eczema and dermatitis.
With long-term use, there was no withdrawal syndrome or deterioration of cognitive functions. Polysomnography in patients with insomnia and anxiety clearly demonstrates an increase in sleep duration and a decrease in the frequency of night awakenings after taking hydroxyzine once or repeatedly at a dose of 50 mg. A decrease in muscle tension in patients with anxiety was noted when taking the drug at a dose of 50 mg 3 times a day.
Indications
- adults for the relief of anxiety, psychomotor agitation, feelings of internal tension, increased irritability in neurological, mental (generalized anxiety and adaptation disorder) and somatic diseases, as well as in chronic alcoholism, alcohol withdrawal syndrome, accompanied by symptoms of psychomotor agitation;
- as a sedative during premedication;
- symptomatic treatment of itching.
Contraindications
hypersensitivity to any of the components of the drug Atarax, cetirizine and other piperazine derivatives, aminophylline or ethylenediamine; porphyria; pregnancy; period of childbirth; breastfeeding period. hereditary galactose intolerance, impaired absorption of glucose-galactose (since the tablets contain lactose).
With caution: myasthenia gravis; prostatic hyperplasia with clinical manifestations, incl. difficulty urinating, constipation; increased intraocular pressure; dementia; tendency to seizures; patients prone to arrhythmia or receiving drugs that can cause arrhythmia; patients simultaneously receiving treatment with other CNS depressants or anticholinergic drugs (the dose should be reduced); patients with severe and moderate severity of renal failure, as well as liver failure (dose reduction is necessary); elderly patients (the dose is reduced in case of reduced glomerular filtration.
Side effects
They are mild and transient, usually disappearing within a few days of starting treatment or after reducing the dose.
Side effects are mainly related to CNS depression or paradoxical CNS stimulatory effects, anticholinergic activity or hypersensitivity reactions.
Anticholinergic effects: dry mouth, urinary retention, constipation or disturbance of accommodation are observed rarely and mainly in elderly patients. Drowsiness and general weakness may occur, especially at the beginning of treatment with the drug. If these effects do not disappear after a few days from the start of therapy, the dose of the drug must be reduced.
There have been reports of other side effects, such as headache, dizziness, increased sweating, hypotension, tachycardia, allergic reactions, nausea, fever, changes in liver function tests, bronchospasm. No clinically significant respiratory depression was observed when prescribed doses.
Involuntary motor activity, incl. very rare cases of tremors and convulsions, disorientation were observed with significant overdose.
Interaction
Atarax® potentiates the effect of drugs that depress the central nervous system, such as opioid analgesics, barbiturates, tranquilizers, hypnotics, ethanol (combinations require individual selection of drug doses).
Atarax®, when used simultaneously, interferes with the pressor effect of epinephrine (adrenaline) and the anticonvulsant activity of phenytoin, and also interferes with the action of betahistine and cholinesterase blockers.
With simultaneous use, Atarax® does not affect the activity of atropine, belladonna alkaloids, cardiac glycosides, antihypertensive drugs, histamine H2 receptor blockers.
Co-administration of Atarax with MAO inhibitors and anticholinergics should be avoided.
Hydroxyzine is an inhibitor of the CYP2D6 isoenzyme and, when used in high doses, may cause interactions with CYP2D6 substrates. Since hydroxyzine is metabolized in the liver, an increase in its concentration in the blood can be expected when co-administered with liver enzyme inhibitors.
How to take, course of administration and dosage
Inside.
Children: for the symptomatic treatment of itching. At the age of 12 months to 6 years - from 1 to 2.5 mg/kg/day of Atarax in several doses, from 6 years and older - from 1 to 2 mg/kg/day in several doses.
For premedication - 1 mg/kg 1 hour before surgery, and additionally the night before anesthesia.
Adults: For the symptomatic treatment of anxiety, 25–100 mg daily in divided doses throughout the day or at night. The standard dose of Atarax is 50 mg per day (12.5 mg in the morning, 12.5 mg in the afternoon and 25 mg at night).
In serious cases, the dose may be increased to 300 mg per day.
For premedication in surgical practice, 50–200 mg (1.5–2.5 mg/kg IM) is administered 1 hour before surgery.
For symptomatic treatment of itching, the initial dose is 25 mg; if necessary, the dose can be increased 4 times (25 mg 4 times a day).
In elderly patients, treatment begins with half the dose of Atarax. In case of renal and/or liver failure, doses should be reduced.
A single maximum dose should not exceed 200 mg, the maximum daily dose should not exceed 300 mg.
Overdose
A manifestation of an overdose of the drug Atarax may be a pronounced anticholinergic effect, depression or paradoxical stimulation of the central nervous system.
Symptoms (with significant overdose): nausea, vomiting, involuntary motor activity, hallucinations, impaired consciousness, arrhythmia, arterial hypotension.
Treatment: if there is no spontaneous vomiting, it is recommended to immediately lavage the stomach and induce vomiting artificially. General supportive measures are indicated, including monitoring the vital functions of the body and monitoring the patient until the symptoms of intoxication disappear and in the next 24 hours. If it is necessary to obtain a vasopressor effect, norepinephrine or metaraminol is prescribed. Epinephrine should not be prescribed. Hemodialysis is not effective. There is no specific antidote.
Special instructions
If allergy tests are necessary, Atarax should be discontinued 5 days before the test.
Since hydroxyzine can affect attention and the speed of psychomotor reactions, patients should be warned about this if it is necessary to drive a car or operate machinery.
Release form
Atarax tablets, white, oblong, film-coated, with a dividing transverse score on both sides.
Storage conditions
In a dry place, at a temperature not exceeding 25 °C
Best before date
5 years
Active substance
Hydroxyzine
Conditions for dispensing from pharmacies
On prescription
Dosage form
pills
Purpose
For children as prescribed by a doctor, For adults as prescribed by a doctor
Indications
Mental disorders, Obsessive-compulsive disorder, Allergies, Alcoholism
Information in the State Register of Medicines
Go
Barcode and weight
Barcode: 4603149000083, 5413787104512 Weight: 0.015 kg
How to take Atarax
At the pharmacy, Atarax can be purchased in two forms - a solution for intramuscular injection and tablets for oral administration. The dosage is selected by the attending physician and depends on the clinical picture of the disease, symptoms, nature of the course and the patient himself, or rather his individual reaction of the body to therapy with Atarax.
How to take Atarax correctly
Atarax in ampoules
Premedication
- children: 1 mg/kg body weight 1 hour before surgery, if necessary, the dose can be administered at night before anesthesia;
- adults: 50–200 mg 1 hour before surgery, if necessary, the same dose can be administered the night before anesthesia.
Symptomatic treatment of itching
- children 1–6 years old: 1–2.5 mg/kg per day in several doses;
- children over 6 years old: 1–2 mg/kg per day in several doses;
- adults: at the beginning of treatment - 25 mg 1 time / day, if necessary, increase the dose to 25 mg 4 times / day. In this case, the maximum dose should not exceed 300 mg per day and 200 mg at a time.
Symptomatic treatment of anxiety: morning and afternoon - 12.5 mg, at night - 25 mg (total daily dose - 50 mg).
If the need arises, the doctor can increase the daily dose to 300 mg (maximum value). But if the patient has a history of renal or liver failure, or if the patient is elderly, then the dose is reduced.
Atarax tablets
Reception during premedication and for symptomatic treatment of itching coincides with the recommendations when using Atarax injection solution.
Anxiety
- The daily dose for adults is 50 mg and, if necessary, can be increased to 300 mg. A quarter of the daily dose is taken in the morning during the day, and all that remains is taken before bed.
If the medicine is used by patients with a history of renal or liver failure, as well as people in older age groups, dosage adjustment (reduction) may be required.
Atarax for anxiety disorders (review)
Ryabokon I.V.
Anxiety is a state of fear and anxiety experienced by a person in anticipation of trouble. The causes of anxiety are varied: emotional instability, a sharp change in living conditions, the upcoming completion of a difficult task, etc. Anxiety may arise due to anticipation of a future threat (punishment or loss of loved ones). Typically, anxiety leads to defensive reactions. Anxiety is the result of frustration or its anticipation and is the primary psychological manifestation of stress. Z. Freud considered anxiety as a symptomatic manifestation of an internal emotional conflict caused by the fact that a person unconsciously suppresses sensations, feelings or impulses that are too threatening or irritating for him. With the emergence of anxiety, behavioral activity increases, the very nature of behavior changes, and additional physiological mechanisms of adaptation to changed conditions are activated.
Anxiety is a person’s tendency to experience a state of anxiety. Most often, a person’s anxiety is associated with the expectation of social consequences of his success or failure. Anxiety and anxiety are closely related to stress. On the one hand, anxious emotions are symptoms of stress. On the other hand, the initial level of anxiety determines individual sensitivity to stress. Like stress in general, the state of anxiety cannot be called unequivocally bad or good.
Sometimes anxiety is natural, adequate, and useful. Everyone feels anxious, restless or stressed in certain situations, especially if they have to do something unusual or prepare for it. For example, giving a speech in front of an audience or passing an exam. A person may feel anxious when walking down an unlit street at night or when lost in a strange city. This type of anxiety is normal and even useful, as it prompts you to prepare a speech, study the material before an exam, and think about whether you really need to go out at night all alone.
In other cases, anxiety is unnatural, pathological, inadequate, harmful. It becomes chronic, constant and begins to appear not only in stressful situations, but also for no apparent reason. Then anxiety not only does not help the person, but, on the contrary, begins to interfere with him in his daily activities.
The line between a “normal” stress response and a pathological anxiety disorder is often quite blurred, and it is difficult for a person to know when to seek professional help. These subsyndromal anxiety disorders are the most difficult to diagnose and often remain untreated, while having an extremely negative impact on the quality of life of the patient and those around him. It is believed that treatment options should be considered when anxiety about everyday events is beyond the patient's control. The following disorders may also be the reason for prescribing therapy: nervousness, fussiness, impaired concentration, irritability, sleep disturbance, symptoms of autonomic dysfunction.
In everyday medical practice, various herbal medicines, tranquilizers, barbiturates, antidepressants, and some antipsychotics are used to treat anxiety disorders.
One of the most powerful and quickly relieving sleep disorders and anxiety are benzodiazepine drugs. Among the disadvantages of treatment with benzodiazepines, the following should be mentioned: withdrawal syndrome (rapid resumption or transient increase in symptoms after discontinuation of the drug), the risk of addiction and the formation of drug dependence, impaired cognitive functions (attention, concentration, memory), and impaired coordination. Therefore, benzodiazepine drugs are not recommended to be taken for more than 2 weeks.
Hydroxyzine (Atarax) is neither a benzodiazepine nor a phenothiazine. The non-benzodiazepine anxiolytic Atarax (hydroxyzine) is a derivative of diphenylmetane, an antagonist of histamine H1 receptors.
Hydroxyzine is one of the oldest psychotropic drugs; it was introduced into clinical practice back in 1955. Atarax has a pronounced anti-anxiety, antihistamine, antipruritic and antiemetic effect. By reducing the concentration of histamine at the central level, it has the property of reducing anxiety, reducing aggressiveness and causing a persistent anxiolytic effect [2]. The drug acts within 15–30 minutes after oral administration (Cmax is noted 2 hours after taking the drug) and maintains this effect for 6–8 hours. Its main advantages are the absence of the “rebound” phenomenon, addiction (dependence), withdrawal symptoms and positive effect on cognitive function.
Hydroxyzine has been successfully used in a variety of areas of medicine: as a means of controlling tobacco smoking [3]; in pediatric dentistry [4]; for its intended purpose – for the treatment of anxiety neurosis (even in the era of the existence of such a nosological form) and for “mild” depression [5]; for behavioral and learning disorders in children [6]. Due to its antihistamine properties, hydroxyzine was used in allergology, to treat itching [7], and for urticaria pigmentosa (mastocytosis) in children [8]; in oncology [9]; in burn patients [10], in narcology [11] and in many other conditions.
Recently, there has been interest among researchers in the use of hydroxyzine in patients with generalized anxiety disorder (GAD). The prevalence of this pathology and the associated burden of social consequences in the current scientific literature appear to be quite significant. According to one review [E.G. Starostina. Generalized anxiety disorder and anxiety symptoms in general medical practice. Rus. honey. magazine 2004; 22 (222), 12: 1277] with reference to numerous foreign works, “GAD is among the top ten diseases with the greatest temporary disability and according to this indicator is on a par with coronary artery disease, diabetes, joint diseases, peptic ulcers, and mental disorders – with depression or even ahead of it.”
In a double-blind, placebo-controlled RCT for the treatment of GAD [17], the anxiolytic activity of Atarax at a dose of 50 mg (in 3 doses of 12.5 mg in the morning and afternoon plus 25 mg in the evening) was shown, which was manifested in a statistically significant, rapid and significant decrease symptoms of anxiety already at the end of the 1st week of treatment, which persisted for another 1 week after cessation of treatment (n=110; course duration 4 weeks; Hamilton-A score). In this case, there was no phenomenon of “rebound” or return of anxiety.
In another double-blind multicenter RCT [18], in which, along with placebo control, the benzodiazepine drug bromazepam was also used, it was shown that hydroxyzine used for 3 months was statistically significantly different from placebo and was as effective as the comparison drug. Moreover, with benzodiazepine, side effects of severe drowsiness were observed twice as often as with hydroxyzine (n = 334; dose of hydroxyzine 50 mg/day in 3 divided doses; bromazepam - 6 mg/day in 3 divided doses; improvement on the Hamilton-A scale >50 %; p<0.03 at the end of the 6th week and p<0.001 - after 12 weeks; the number of patients who responded to treatment: 40% at the 6th and 60% at the 12th week, respectively).
Another study [19] showed the effectiveness of Atarax (50 mg in 3 doses), comparable to that of the control buspirone (20 mg in 3 doses), with a statistically significant difference between Atarax and placebo on the 28th day of treatment (p<0.015) . There was no rebound phenomenon with abrupt withdrawal of both drugs (n=244; age 18–65 years).
In addition, one of the advantages of hydroxyzine is that, unlike benzodiazepines, it does not depress cognitive abilities [20] (triple crossover, double-blind RCT; comparing a single dose of 50 mg of hydroxyzine with a single dose of 2 mg of lorazepam and placebo; n = 9; healthy volunteers; 3-day interval before cross-over; assessment of cognitive functions 2–5 hours after taking comparator drugs).
Some studies have shown a positive effect of hydroxyzine on cognitive function [21] (comparison with lorazepam; double-blind multicenter RCT; n=30; GAD, Atarax 100 mg in 3 divided doses, lorazepam 4 mg in 3 divided doses; Beck score 28– th day of treatment). Unlike lorazepam, with the same anxiolytic activity, hydroxyzine restored cognitive function to normal limits.
Similar results were obtained in another, less conclusive study - an open RCT (A.E. Bobrov et al. Journal of Neurology and Psychiatry named after S.S. Korsakov. 1988; 2. GAD; n=50; outpatients; treatment course is 4 weeks, plus 2 weeks of follow-up).
Considering the characteristics of the drug (quick onset of action, good tolerability), lack of dependence and depression of the central nervous system make it an alternative drug to benzodiazepines in children and adolescents. In a study conducted at the Children's Psychiatry Center [23], Atarax was prescribed for various forms of mental illness in children and adolescents with manifestations of anxiety, irritability and insomnia-type sleep disorders, and its effectiveness was assessed. The study included 50 patients aged 5 to 18 years with various forms of mental illness, who were undergoing outpatient observation and treatment at the Children's Psychiatry Center. At the end of the 4th week of therapy, there was a decrease in the manifestations of anxiety and various fears noted earlier: falling asleep in the dark, staying at home in the absence of parents, fears of animals, noise of household appliances; in one case, a five-year-old boy could stay at home with a nanny without his parents (he had previously shown a pronounced affective reaction). In addition, all patients' sleep improved already in the second week of therapy, tearfulness, moodiness, and irritability were reduced. Simultaneously with the reduction of anxiety, the mood improved in 7 patients with a mixed anxious and depressive reaction caused by an adaptation disorder and with a mixed anxiety and depressive disorder, which was associated not with the direct antidepressant effect of Atarax, but with the comorbid dependence of anxiety and depression: anxiety was reduced - depression went away.
In a comparative study [22] of etifoxine and Atarax (hydroxyzine), the compared anxiolytics demonstrated high effectiveness in a wide range of psychopathological manifestations of adjustment disorders and generalized anxiety disorder. The results of therapy with etifoxine and Atarax showed the comparability of the clinical effect of the compared drugs, confirmed by a number of formalized indicators. The proportions of responders were comparable: 73.3 and 53.3% in the HARS assessment; 66.7 and 53.3% - as assessed by CGI-S for the groups receiving etifoxine and Atarax. The main clinical effect of the drugs in both groups was a decrease in the severity of manifestations of mental anxiety: the symptoms of internal tension (ethifoxine - in the 2nd week, Atarax - in the 3rd week), reactive (emotional) lability (one of the sub-items of “depressive mood”) were most quickly reduced "). In general, similar dynamics of cognitive anxiety were observed in both groups.
To summarize, we can reiterate that hydroxyzine (Atarax) has shown clear advantages over benzodiazepine anxiolytics in the treatment of anxiety disorders. Being as therapeutically effective as benzodiazepine anxiolytics, it does not produce rebound effects, does not depress cognitive function, and does not cause pathological dependence.
Literature:
1. Psychotropics 2000/2001 Lundbeck.
2. Krebs MO. Le trouble anxieux: cliniqu et implicacion neurobiologiques. La Revfue des Entretiens de Bichat 2001; 2 (5).
3. Turle G. An investigation into the therapeutic action of hydroxyzine/Atarax in the treatment of nervous disorders and the control of tobacco-habit. Brit J Psychiat 1958; 104: 82 rub. 33.
4. Lang L. An evaluation of the efficacy of hydroxyzine (atarax–vistaril) in controlling the behavior of child patients. J-Dent-Child 1965; 32, 4: 253–8)
5. R.Middlefell, K.Edwards Hydroxyzine/Atarax in the relief of tension associated with anxiety neurosis and mild depressive states. Brit J Psychiat 1959; 105:792–4.
6. Segal L, Tansley A. A clinical trial with Hydroxyzine (Atarax) on a group of maladjusted educationally subnormal children. J Mental–Science; Br J Psychiat from 1963; 1957; 103:677–81.
7. Rhoades R, Leifer K, Cohan R, Wittig H. Suppression of histamine-induced pruritus by three antihistaminic drugs. J Allergy Clin Immunol, 1975 Mar.; 55, 3: 180–5.
8. Kettelhut B, Berkebile C, Bradley D, Metcalfe D. A double-blind, placebo-controlled, crossover trial of ketotifen versus hydroxyzine in the treatment of pediatric mastocytosis. J Allergy Clin Immunol 1989 May; 83, 5: 866–70)
9. Broder L, Lean N, Hilsenbeck S. A randomized blinded clinical trial comparing delta–9–tetrahydrocannabinol (THC) and hydroxizine (HZ) as antiemetics (AE) for cancer chemotherapy (CT). PROC–AM–ASSOC–CANCER–RES; 1982; 23:514.
10. Vitale M, Fields–Blache C, Luterman. A Severe itching in the patient with burns. J burn care & rehabilitation 1991; 12, 4: 330–3.
11. Kaim S, Klett C, B. Rothfeld. Treatment of the acute alcohol withdrawal state: a comparison of four drugs. Agressologie: revue internationale de physio-biologie et de pharmacologie appliquees aux effets de l'agression, 1968; 9, 2: 305–8.
12. Chignon G. Le trouble Anxiete Generalise: du probleme diagnostique au defi therapeutique. Nervure J psychiat 1988; 11 (suppl.): 1–16.
13. Wittchen H–U, Jakobi F. Size and burden of mental disorders in Europe – a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol 2005; 15: 357–76; For details, see the February issue of our magazine).
14. Goodwin R, Gorman J. Psychopharmakologic Treatment of generalized anxiety disorder and risk of major Depression. Am J Psychiat 2002; 159:1935–7.
15. Goodwin RD, Jack M. Gorman. Treatment of generalized anxiety disorder with psychotropic drugs and the risk of major depressive disorder
16. Martin P. Coprescription, Antidepresseurs et anxiolytiques: consequences pratiques de la meilleure connaissance desmecanismes d'action putatifs des anxiolytiques. Actuel Psychiat 2001; 19 (1/2): 2–7.
17. Ferreri M, Hantouche T, M. Billardon. Interet de l'hydroxizyne dans des troubles d'anxiete generalisee: etude controlee en double aveugle versus placebo. L'encephale 1994; 20: 785–91.
18. Llorka P. et al. Efficiency and safety of hydroxysyne in the treatment of generalized anxiety disorder: a 3-month double-blind study. J Clin Psychiatry 2002; 63:1020–7.
19. Lader Scotto J. A multicenter double–blind comparison of hydroxizine, buspirone and placebo in patient with generalized anxiety disorder. Psychopharmacology 1998; 139:402–6.
20. De Brabander A, Deberdt W. Effect of hydroxizyne on attention and memory. Human Psychopharmacology 1990; 357–62.
21. Samuelian J, Billardon M, Guillou N. Retentissment sur les functions cognitives de deux traits anxiolitiques chez des patients souffrant d'anxiete generalisee. L'encephale 1995; 21:147
22. Andryushchenko A.V., Beskova D.A., Romanov D.V. Psychopharmacotherapy of generalized anxiety (experience with the use of Strezam and Atarax) Mental disorders in general medicine No. 1; pp. 33–36
23. Rezakov A.A. Experience of using hydroxyzine (atarax) in children and adolescents. "PHARMIndex-Practik" issue 10; 2006, pp.37–39
Compatibility with other drugs
A separate issue when taking Atarax is its interaction with other medications. Thus, barbiturates, tranquilizers, opioid analgesics, ethanol-containing drugs, sleeping pills and any other drugs that depress the central nervous system, when taken simultaneously with the drug Atarax, enhance the effects. That is, lethargy, indifference, drowsiness and other effects will appear several times brighter and stronger. But if it is still necessary to take everything together, then the doctor monitoring the patient will draw up a dosage regimen and select an individual dosage for each drug.
Compatibility of other drugs with Atarax
The combination of Atarax + MAO inhibitors, anticholinergics is not recommended. Atarax is able to inhibit the action of epinephrine (adrenaline) and suspend the anticonvulsant effect of phenytoin.
Atarax has a destructive effect on the metabolism of substrate drugs for uridine diphosphate and glucuronyl transferase.
If you drink Cimetidine and Atarax at the same time, the concentration of hydroxyzine in the blood plasma will increase, but on the contrary, the concentration of metabolites will decrease.
As for cardiac glycosides, atropines, antihypertensive drugs, antiallergic drugs, Atarax does not in any way affect their functionality; the pharmacological effect provided.
However, it is worth remembering that it is better not to take drugs whose side effects indicate possible arrhythmia with Atarax. When they are mixed, there is a risk of prolongation of the QT interval and the development of ventricular tachycardia of the “pirouette” type.
About anxiolytic therapy with hydroxyzine (Atarax)
Practicing doctors of various specialties have long and widely used psychotropic drugs of different classes in the combined treatment of mental disorders of a non-psychotic level, giving constant preference to benzodiazepine tranquilizers from different groups of drugs in this series. As a rule, the choice is made in favor of the most well-known of them, and this choice is mainly justified by empirical ideas about the effectiveness and relative safety of psychopharmacological drugs, the administration of which leads to a fairly rapid, although not always complete and persistent anxiolytic effect. The use of tranquilizers in order to achieve a hypnotic and anti-anxiety effect has become so firmly established in everyday practice [2,13] that drugs of this series have not only long been in the arsenal of therapeutic agents for doctors working with different groups of patients, but are also constantly on everyone’s lips. . At the same time, even doctors with insufficient clinical and therapeutic experience do not bother themselves with doubts or reasoned justification for this or that remedy and do not prescribe the drug by clarifying its properties and nuances of indications or contraindications for this type of therapy. As a recent special study showed [12], 38% of doctors trust only their own experience in using medications, although, as a rule, they do not conduct a serious analysis of the results of their prescriptions. Very rarely (8%) prescriptions or changes in treatment are based on the recommendations of experts (consultants) or the opinions of colleagues (5%), and the published results of studies, both domestic and foreign, judging by the results of a special survey, have practically no significance in the choice therapy. As the experience of joint cooperation between internists and psychiatrists shows, the greatest alertness and rigor in justifying prescriptions is demonstrated by doctors providing assistance in urgent situations, despite the fact that in these cases we are not talking about long courses. On the contrary, in the routine practice of doctors in a polyclinic and general somatic hospital, the ease of prescribing, in particular, benzodiazepine tranquilizers is not overcome by any administrative or resource restrictions, often of a temporary nature. With a general understanding of the complexities of changes in medical ideas, tolerance for the traditional inertia of clinical thinking, and the established views of medical practitioners, such a conservative idea does not meet all the attempts being made to reverse the style of passive perception of old models and views on the treatment of mental disorders of a non-psychotic level [10], especially taking into account development and emergence of new non-benzodiazepine tranquilizers and hypnotics. In recent years, a systematic scientific analysis of the use of benzodiazepine tranquilizers for anxiolytic therapy has been repeatedly undertaken [2,7]. Data on the consumption of benzodiazepines (BD) indicate that they remain the most frequently prescribed psychotropic drugs, although there is also a tendency to lose their leading role in the treatment of neurotic disorders with anxiety and other manifestations [15]. Still, at present, the proportion of patients receiving BD ranges from 52 to 76%, and most often these drugs are prescribed for the correction of dyssomnia disorders and somewhat less often as an anxiolytic agent. From 10 to 15% of the total population in different countries receive a prescription for one or another tranquilizer once a year. Anxiety conditions account for 19.2% of all benzodiazepine tranquilizer prescriptions, and are significantly more common in outpatient therapy than in inpatient settings [2]. According to the results of another study [8], tranquilizers account for 36.3% of all prescriptions in outpatient practice to patients with a depressive disorder identified during a population survey and thus not diagnosed by the attending physician. The fairly rapid achievement of anti-anxiety, primarily sedative, effect, the absence of adverse effects on a number of functional systems of the body and interaction with somatotropic drugs [7] justify the known expectations of doctors and patients, at least at the beginning of treatment. The psychotropic properties of anxiolytics are associated with their effect on the GABAergic neurotransmitter system. Due to the fact that the neurons of this system are morphologically homogeneous in different parts of the central nervous system, tranquilizers can affect most of the functional formations of the brain. In this case, anxiolytics act on areas of the brain with maximum arousal and stimulate the suppression of the activity of most neurons. This explains the relief of anxiety and somatotropic effects (in particular, reduction of vegetative symptoms). Undoubtedly, the positive experience of the widespread use of benzodiazepine tranquilizers is accompanied by the identification of a number of problems associated with the peculiarities of their pharmacological action and the development of known side effects of therapy [6]. The main ones include: – phenomena of hypersedation (daytime sleepiness, decreased level of wakefulness, impaired concentration, complaints of forgetfulness). These manifestations occur in 10% of cases and have a dose-dependent effect; – muscle relaxation (general weakness, muscle weakness) occurs in 1–2% of elderly people, much more often and often leads to falls; – so-called “behavioral toxicity” (mild impairment of cognitive functions and coordination); – “paradoxical reactions” (increased agitation); – mental and physical non-toxicomaniac dependence (can occur with long-term use and be accompanied by phenomena similar to neurotic anxiety when withdrawing from BD). For these reasons, there has been a tendency towards the loss of the dominant position of BD in the treatment of neurotic disorders; the desire to avoid side effects by shortening courses of BD therapy inevitably minimized the therapeutic effect [15]. In connection with the achievements of neuroscience, increasing knowledge about neurochemical processes in the central nervous system and modern trends in the development of drugs that increasingly selectively affect certain neurotransmitter systems, the range of anxiolytic drugs with a narrower spectrum of undesirable effects and more targeted psychotropic activity is expanding [1] . Overcoming the dichotomy of psychiatry and psychosomatic medicine in the last decades of the last century took shape in an intensively developing independent scientific direction, most systematically and comprehensively represented in the achievements of a team that unites researchers from the Department of Borderline Mental Pathology and Psychosomatics of the National Center for Mental Health of the Russian Academy of Medical Sciences and the Department of Psychiatry and Psychosomatics of the Faculty of Physiopathology and Psychosomatics of the Russian Academy of Medical Sciences. THEM. Sechenov under the leadership of Academician of the Russian Academy of Medical Sciences A.B. Smulevich. In accordance with the developed concepts [16,17], the phenomenology of psychosomatic pathology includes: © constitutional anomalies (neuropathic constitution) and mental pathology realized in the somatic sphere; © mental (organo-neurotic) somatized (somatoform) disorders that develop on pathologically altered (somatic) grounds; © mental (psychogenic) disorders provoked by somatic diseases - nosogenic reactions and personality development; © somatic pathology provoked by mental disorders (psychosomatic diseases). The clinical parameters of disorders characteristic of psychosomatic medicine in general are reflected in the most general form by psychocardiology. To date, the scientific and practical results of the joint 15-year collaboration of psychiatrists and cardiologists, recently published in the monograph by Acad. RAMS, prof. A.B. Smulevich and prof. A.L. Syrkin “Psychocardiology” [17]. Psychosomatic relationships in a cardiology clinic, according to the concept of researchers, form a continuum, at one pole of which predominantly mental disorders prevail, and at the other - cardiovascular disorders. The possibility of interpreting neurotic disorders within a wide range is proved, allowing the coexistence of cardioneurosis as an organo-neurotic disorder, on the one hand, with manifestations of other mental disorders, and on the other, with signs of undoubted somatic pathology. This approach is considered as the most promising, allowing to take into account the complexity of pathogenetic relationships, including (along with psychogenic factors) not only mental, but also somatic pathology, which is of independent importance when developing strategies and tactics of therapeutic intervention. Cardioneurotic disorders lead in frequency and account for slightly less than half of all forms of organ neuroses. In the entire sample of patients in general somatic institutions, patients with these manifestations account for 4.7%, while in the hospital - 1.8%, and in the clinic - 15.6%, that is, with a multiple increase in the frequency of cardioneurosis among the outpatient population of patients. The largest proportion of such patients are in therapeutic and cardiology departments (26 and 39%, respectively). Cardioneurotic disorders in a variety of manifestations are much more common in women (66%). The diagnostic criteria for cardioneurosis, developed jointly by cardiologists and psychiatrists, include the following signs: 1) persistent or recurrent symptoms for at least 3 months (unpleasant sensations in the heart area or cardialgia, palpitations, tendency to tachycardia, extrasystole); 2) the connection between the occurrence of symptoms and psychogenic influences or periods of hormonal changes; 3) signs of autonomic dysfunction, lability of heart rate and blood pressure; 4) nonspecific and variable ECG indicators [17]. Among the mental disorders in patients with cardioneurosis, the leading symptoms are anxiety symptoms within the framework of an anxiety-neurotic disorder or anxious depression. The most common are anxiety-phobic disorders, panic attacks and hypochondriacal phobias (65.2, 61.6, 58.0%, respectively). Symptoms of cardioneurosis may be a manifestation of a depressive state within the framework of cyclothymia, the dynamics of a personality disorder or dysthymia. Concomitant somatic pathology is detected in half of patients with cardioneurosis [17]. Among comorbid somatic pathologies, diseases of the cardiovascular system predominate in frequency, usually in the initial stages and with subclinical manifestations. Anxiety states often develop spontaneously, while attacks of angina are provoked, as a rule, by physical activity. A combination of these forms of pathology is possible, as a result of which the clinical symptoms of exacerbation of coronary artery disease appear to be inappropriately more severe in comparison with objectively detected signs of ischemia. Nosogenic reactions in cardiac patients are considered as an independent form of psychopathological disorder. The formation of nosogenies of the hyper- and hyponosognosic type involves: information about the diagnosis, clinical features of somatic disease and comorbid mental pathology, personal and constitutional characteristics, age, gender and social factors. The frequency of nosogenic reactions in inpatients with coronary artery disease is 28.2%, ranking first among other forms of comorbid mental pathology identified in this group of patients. Non-psychotic disorders in patients who have undergone CABG surgery are considered as very special forms of reactions and personality development [14]. The prevalence and severity of anxiety disorders in patients of general somatic, and especially cardiological practice, determines the need for anxiolytic therapy. Special studies have examined the need for the prescription of psychopharmacological agents and indications for this type of treatment in patients in general somatic institutions. In determining the relevant indicators, two calculation methods were used - according to the actual prescription and according to expert assessment of the indications for the use of certain psychotropic drugs [7,8,17]. It was found that they are prescribed to almost half of the patients (49.3%), while in 37.5% they are tranquilizers. On average in a hospital, the prescription of psychotropic drugs is 0.8 drugs per 1 patient (in general therapeutic departments - 1.3, in cardiology departments - 1.2, and in cardiac intensive care departments this figure is even higher). Psychotropic drugs are prescribed by cardiologists in 82% of cases and only in 14% by consultation with a psychiatrist. Among the medications consumed, tranquilizers predominate (62.3%). Expert assessment indicates that more than two thirds of cardiac patients (67.2%) require psychotropic medications. Anxiolytic therapy with tranquilizers is carried out for somatoform disorders, organ neuroses (cardio- and angioneuroses, etc.), psychogenic reactions and the development of nosogenies, with a predominance in the clinical picture of somatized anxiety, phobias, algia, hysteriform and vegetative manifestations and other manifestations of neurotic hypochondria [14, 17]. In combination with antidepressants, tranquilizers are indicated for depressed patients to quickly reduce symptoms of anxiety and sleep disorders. In combined therapy of comorbid somatic and mental pathology of a non-psychotic level, the somatotropic, including cardiotropic, effect of anxiolytics is used [7]. As a result, the proportion of respondents increases significantly (up to 54%). Although benzodiazepine tranquilizers retain their position among the most frequently prescribed drugs in anxiolytic therapy, recently non-benzodiazepine anxiolytics, which lack a number of properties that cause the undesirable effects of tranquilizer therapy, have attracted increasing attention from researchers and doctors. In addition, the search for new medications for the treatment of anxiety disorders remains relevant due to the clinical and pathogenetic diversity of these conditions and the constant need for the development of differentiated therapy with drugs that have the most selective effect on anxiety symptoms. These drugs include hydroxyzine (Atarax). Hydroxyzine is not a benzodiazepine or phenothiazine. In the 60s of the 20th century, a number of clinical studies when prescribing the drug in doses from 100 mg to 400 mg revealed its anxiolytic properties, but only 30 years later the effectiveness of Atarax in generalized anxiety disorder was proven [19,20]. It was found that in terms of the speed of onset of the anti-anxiety effect, hydroxyzine is not inferior to benzodiazepines, increases the duration of the REM sleep phase and eliminates dissomnia disorders, reduces the manifestations of tension and stress, and anxiety symptoms. At the same time, good tolerance of cognitive functions to its action was found, the absence of an amnestic effect and dependence on its use. Thus, the administration of hydroxyzine represents a therapeutic alternative to benzodiazepine tranquilizers in the treatment of anxiety disorders of various origins. Hydroxyzine in its chemical structure is a derivative of diphenylmethane. The pharmacokinetic properties of the drug ensure its rapid absorption from the gastrointestinal tract. The maximum concentration in blood plasma is achieved after 2 hours, in tissues - at a higher level. The drug penetrates the blood-brain barrier and the placenta, accumulating more in fetal tissues than in maternal tissues. Hydroxyzine is metabolized in the liver. Its main metabolite is an H1 blocker. The antihistamine effect occurs within an hour after ingestion. Less than 1% of the drug is excreted unchanged by the kidneys. The half-life depends on the age of the patients (from 7 hours in children to 20 hours in adults and 29 hours in the elderly and elderly). In case of overdose, the biotransformation of hydroxyzine occurs in a different way. In patients with liver disease, the half-life is extended to 37 hours, and the antihistamine effect is extended to 96 hours. The onset of the psychotropic effect of hydroxyzine is detected 5–10 minutes after intramuscular administration and 30–40 minutes after oral administration. The drug also has antispasmodic, sympathicolytic, bronchodilator and antiemetic effects, significantly reduces itching in patients with urticaria, eczema, and dermatitis. Hydroxyzine prevents the development of the pressor effect of adrenaline, the anticonvulsant activity of phenytoin and anticholinesterase drugs, but does not change the effect of atropine, belladonna alkaloids, digitalis, antihypertensive drugs, H2-antihistamines, and weakens the gastrointestinal side effects of theophylline and H2-agonists. Inhibitors of liver enzymes are potentially capable of increasing the concentration of hydroxyzine in the blood. In connection with the indicated properties, the drug is not prescribed simultaneously with MAO inhibitors, and when an overdose for lifting pressure, only norepinephrine is used, but not adrenaline. Hydroxine in ordinary dosages does not cause clinically significant respiratory depression (as opposed to the possibility of such an effect in benzodiazepines). Atarax is produced in three drug forms: in 25 mg tablets, in a solution for injection (only intramuscular!) - in ampoules of 2 ml (in 1 ml of 50 mg), as well as in the form of syrup (0.02%) in the bottles 20 ml with a content of 2 mg of the drug in 1 ml. Thus, the possibility of alternative oral methods of introducing atarax is given [3.16.17]. In psychiatric practice, Atarax is prescribed in doses from 50 mg to 100 mg per day, divided into two or three doses. Sometimes it is possible to increase the dose up to 300 mg per day. The maximum single dose is 200 mg, the maximum daily dose is 300 mg. An elderly patients are prescribed a half dose of the drug. For children, the dose of atarax is calculated by body weight (1-2 mg per kg of weight in several receptions per day). Domestic researchers have studied the effectiveness of anxiolytic therapy with hydroxyzine both in psychiatric and in general social practice. Based on the material of 50 patients (the average age of 42 years) according to the results of 4 -heat treatment with hydroxyzine in various alarming and neurotic disorders, significant reduction of the symptoms of anxiety was noted [4]. In 66% of observations, the results are regarded as excellent and good, unsatisfactory result was obtained only in 10%. The most pronounced decrease in the severity of anxiety (along two alarm scales - Hamilton and Fard) is registered with a generalized alarming disorder, and less distinct - with maladaptation reactions. However, by the end of the therapeutic course, leveling of differences in the level of anxiety between groups of patients with different genesis of anxious symptoms was noted. Significant changes in the state were noted after two weeks of treatment with the initial detection of the sedative effect and the rapid attachment of an anxiolytic effect itself. At the end of the relatively short -term course, the therapeutic effect was preserved. As the most important feature, the absence of phenomena of psychological and physical dependence on the use of hydroxyzine was noted. In somatic practice, the psychotropic activity of hydroxyzine was studied in patients with cardio -European disorders underwent examination and treatment in a cardiological hospital and in a general -power clinic [9]. The routine purpose of thymoanaleptics and tranquilizers was ineffective and was limited to contraindications from the cardiovascular system and age -related restrictions (the average age of patients of 59 years). In a group of 39 patients, by the 14th day of therapy, hydroxyzine turned out to be 36% of responders, and 67% of responders by the 28th day. The response to therapy was higher with the predominance of somatized anxiety in the structure of cardiourosis. Gidoxin discovered compliance with the requirements for anxiolytics during the treatment of anxiety disorders, comorbid cardiovascular diseases. A positive effect on functional disorders by the cardiovascular system (tachycardia, cardialgia, a sensation of heartbeat, and pulsation of blood vessels) was noted. There were no manifestations of the "behavioral toxicity" characteristic of benzodiazepine tranquilizers, and the abolition syndrome. Hydroxine was well tolerated by patients with coronary heart disease, conditions after acute myocardial infarction and did not find negative interaction with the basic therapy of cardiovascular disease. The most important feature of the psychotropic activity of hydroxyzine, in contrast to benzodiazepine tranquilizers, is the absence of a negative effect on cognitive functions [5,19,20]. In a special study [5], the state of cognitive functioning was studied in patients who received hydroxyzine. The dynamic assessment of cognitive functions was carried out using tests of memorization of 10 words, the dough of the numbers, the test of repertoire grilles, the attention test (“flickering”) and iconograms. The results of the study showed that hydroxyzine does not cause inhibition and weakening of memory. On the contrary, test results demonstrated improvement, pace of thinking, improving short -term memory and normalizing important aspects of perception and assessment of reality. It was revealed that the therapeutic activity of hydroxyzine is manifested unequally depending on the characteristics of the cognitive style in the patents, which is associated with the selectivity of the anxiolytic effect of hydroxyzine. The prospects of the use of hydroxyzine are considered in order to prevent chronicity of neurotic conditions with anxious symptoms, as well as an agent with preventive, contributive properties. Hydoxizine finds its application in psychiatry and in a number of other indications, but using its anxiolytic properties. The drug is prescribed as a drug that improves sleep [3]. A comparative study of the effectiveness of modern antidepressants and hydroxyzine in the treatment of anxious and depressive disorders on the material of patients of the general somatic clinic [18] confirmed the anxiolytic properties of the drug, but showed only partial relief of depressive symptoms in hydraulic monotoxizine monotherapy. It is noted that the improvement in the mental state, achieved at the intake of the drug, was also preserved at the end of treatment with hydroxyzine in 25% of patients. The feasibility of the use of hydroxyzine as a means of premedication during electricity therapy (EST) has been proved. Due to the often experienced fear of the procedure, such patients were previously prescribed tranquilizers or neuroleptics in combination with cholinolytics. Meanwhile, it is known that benzodiazepines lower the convulsive readiness of the brain, can cause respiratory holding, which has a negative effect in this type of therapy of mental disorders resistant to psychopharmacotherapy. An hour before the EST intramuscularly 20 patients were administered hydroxyzine at a dose of 100 mg. After 15 minutes, a sedative and transcoving effect came, a feeling of fear, anxiety and a sense of tension disappeared. The premedication of hydroxyzine did not affect the conduct of anesthesia and the nature of the caused convulsive syndrome. There were no complications due to the use of hydroxyzine. The drug is considered as a useful alternative to benzodiazepines for stopping anxiety in anticipation of EST session [11]. The unique features of the anxiolytic action of the atarax, the rapid onset of the therapeutic effect, the lack of muscle relaxation, pronounced sedation and “behavioral toxicity” along with the lack of negative effects on cognitive functions make it possible to recommend the drug to use in the widest circle of anxious disorders in various clinical situations. The ability to avoid side effects of benzodiazepine tranquilizers justifies the prescription of atarax as a drug of choice in cardiourotic disorders of various genesis and other organic neurosis (in particular, in the skin clinic, taking into account the powerful antipruritic effect of the drug). The use of the somatotropic effect of hydroxyzine in relation to the functional disorders of the cardiovascular system substantiates its use in difficult conditions of comorbid somatic pathology. Cautions relate to the simultaneous purpose of antiarrhythmics. Due to the features of pharmacokinetics, the drug is contraindicated in porphyria and is not recommended for use during pregnancy, in childbirth, and breastfeeding. Knowing all the features of psychotropic and somatotropic activity of hydroxyzine (Atarax) along with the accumulation of their own clinical experience and regular familiarization with the results of research are the necessary basis for the rational application of this effective and safe anxiolytic in the practice of psychiatrists and internists. The community of professional goals of clinicians of various specialties in relation to patients whose condition includes comorbid somatic and mental pathology that does not imply an alternative separation as in terms of diagnosis. and in the aspect of therapy, contributes to progress in the understanding of the pathogenesis of somatopsychic and psychosomatic relationships in their natural unity.
Literature 1. Avedisova A.S., Borodin V.I. Adverse events in pharmacotherapy of borderline mental disorders. Psychiatry and Psychopharmacotherapy, 2003, vol. 5, no. 3, pp. 96–100. 2. Avedisova A.S., Yastrebov D.V., Kostycheva E.A. et al. Ibid., 2005, volume 7, no. 2, pp. 63–68. 3. Arana J., Rosenbaum J. Pharmacotherapy of mental disorders. Moscow. Publishing house Binom, 2004, p. 309. 4. Bobrov A.E., Belyanchikova M.A., Gladyshev O.A. et al. The drug atarax in the outpatient treatment of anxiety. Journal neuropathol. and psychiatrist. them. S.S. Korsakova, 1998, volume 98, issue. 2, pp. 31–33. 5. Bobrov A.E., Kulygina M.A., Belyanchikova M.A. et al. The effect of the drug atarax on cognitive functions in the treatment of anxiety disorders. Psychiatry and psychopharmacotherapy, 2000, volume 2, no. 1, pp. 23–28. 6. Borodin V.I. Side effects of tranquilizers and their role in borderline psychiatry. Ibid., 2000, volume 2, no. 3, pp. 72–74. 7. Drobizhev M.Yu. Psychopharmacotherapy in the general somatic network (somatotropic effects, compatibility with somatotropic drugs). Ibid., 2000, volume 2, no. 2, pp. 49 – 52. 8. Drobizhev M.Yu. The practice of using antidepressants in the treatment of depression in psychiatry and the general medical network (review of the results of pharmacoepidemiological studies). Ibid., 2004, volume 6, no. 5, pp. 221–223. 9. Drobizhev M.Yu., Ivanov S.V., Lebedeva O.I. et al. Therapy of cardioneurotic disorders in the general medical network (experience of using atarax). In the book: Anxiety and obsessions. M., 1998, pp. 286–295. 10. Kornetov N.A. Comorbidity of somatic diseases and depressive disorders: overcoming psychosomatic dualism. In the book: X11 Russian National Congress “Man and Medicine”. Current issues in cardiology, neurology and psychiatry. M., 2005, pp. 226–244. 11. Kostitsyn N.V., Ilyin S.A., Tsukarze E.E. et al. About the experience of using hydroxyzine (atarax) as a premedication during ECT. In the book: Materials of the XIth Congress of Psychiatrists of Russia. November 15 – 18, 2005 M., 2005, pp. 273–274. 12. Mosolov S.N. Controversial and little-studied issues of the practical use of antipsychotic pharmacotherapy in patients with schizophrenia (analysis of the results of an interactive survey of doctors). Journal Psychiatry, 2006, No. 3, in press. 13. Pogosova G.V., Romasenko L.V. Diagnosis and treatment of depression in patients with cardiovascular diseases (results of a multicenter prospective study COORDINATE). Psychiatry and psychopharmacotherapy, 2006, volume 8, no. 1, pp. 47–50. 14. Samushiya M.A. Approaches to pharmacotherapy of pathological dynamics of personality disorders at the stage of outpatient rehabilitation after coronary artery bypass surgery. Journal Psychiatry, 2005, no. 2, pp. 20–26. 15. Sergeev I.I. Psychiatry and psychopharmacotherapy, 2003, volume 5, no. 6, pp. 230–235. 16. Smulevich A.B. Depression in somatic and mental illnesses. MIA. Moscow, 2003, pp. 238–240. 17. Smulevich A.B., Syrkin A.L. Psychocardiology. MIA. Moscow, 2005, 778 pp. 18. Chernetsov M.Yu. Comparative effectiveness of treatment of anxiety and depressive disorders with modern antidepressants and the atypical tranquilizer hydroxyzine in patients of the psychotherapeutic office of a city clinic. In the book: Mater. X! At the Congress of Russian Psychiatrists. November 15–18, 2005 M., 2005, pp. 293–294. 19., Recent clinical trials of hydroxyzine in generalized anxiety disorder. Acta psychiat. scand., 1998, 98, Suppl. 393, pp. 102–108/ 20. Hantouche E.–G., Ferreri M. Efficacy of hydroxyzine in generalized anxiety. Psychiatry and Psychopharmacotherapy, 2000, volume 2, 3;, pp. 124–125.
Atarax and alcohol
Drinking alcohol is prohibited while taking Atarax medication
During therapy with the drug, drinking alcohol is prohibited, as alcohol enhances the effect of the drug and provokes adverse reactions. That is, the central nervous system is depressed, the state of intoxication increases, blood pressure decreases, and allergic reactions appear. With all this, there is a high risk of severe intoxication of the body, which can lead to death.
Treatment of phobias and fears: which methods are useful and which are harmful
So, avoidant behavior is harmful, neurosis will only grow. But if you simply expose your psyche to the “scenery” where you are anxious, and wait until everything passes, then, firstly, this is not pleasant, and secondly, you will probably not be able to meet the necessary conditions for the psyche to be overloaded. The anxiety state should go away (or greatly decrease) in the situation in which it began. This is one of the necessary conditions.
Without this, at best, there will be less fear, but you will still be tense and anxious. Therefore, it is important that you calm yourself down correctly, for example, with relaxation techniques, correct explanations to yourself of the nature of the attack and its consequences...
Incorrect/harmful ways to stop anxiety include :
- trying to avoid the situation
- turning to medication or seeking help from loved ones and doctors (trying to make sure everything is okay, for example, in case of panic, measuring blood pressure),
- for social fears - attempts to make sure (by assessing the reaction to your behavior) that the attitude towards you has not changed.
The tactic of “being in an alarming situation” can be implemented in two ways. Gradually immersing yourself in more and more alarming circumstances (if you are afraid of being far from home, you need to gradually, from day to day, increase the distance; if you are afraid of flying, first learn to calmly watch videos of airplane flights, then go to the airport, and then already flying).
From our point of view, such a tactic of gradually immersing oneself (desensitization) loses the second, when a person goes straight into an alarming situation. This way you can retrain your psyche much faster, because the main thing is to be able to cope with fear, stop being afraid of it and avoid it. If you do not face these experiences during therapy, then important experiences will not appear. But remember, you have to have the tools/techniques to help yourself through the situation and not just try to calm yourself down by willpower. Techniques and methods can be combined, the main thing is that it is comfortable and effective.
So, let's say you've worked through your fears and the mechanisms that support them (avoidance is just one of them). If you have what are called simple phobias (when there is only one situation or object that causes fear, for example, fear of riding in an elevator, in a car, flying on an airplane), then it is quite possible that the techniques described above will be enough to make more of these Don't be afraid of situations.
Atarax for neuroses and panic attacks
Neuroses are a fairly common diagnosis. This is a reversible neuropsychic disorder, which is provoked by constant stress, chronic fatigue, tension and anxiety. Neuroses are often accompanied by panic attacks. A panic attack is a state of sudden and extremely intense attack of fear or anxiety. Refers to neurotic diseases.
For such conditions, the doctor may prescribe Atarax. The main purpose of this tranquilizer is to calm and relieve anxiety. The product must be used strictly as prescribed by the doctor in the prescribed dosage and regularity. Atarax suppresses the activity of certain areas of the brain, relieving tension and panic attacks.
Panic attacks. Modern diagnostic methods.
Only a qualified neurologist-vegetologist can diagnose panic disorder, which manifests itself as panic attacks, identify its symptoms and prescribe optimal treatment.
At the initial examination, the vegetarian doctor must examine the patient’s normal reflexes, his muscular system, sensory organs, cognitive functions (memory, speech, perception), assess the general psycho-emotional state of the patient, taking into account all his complaints in order to collect a complete picture of the disease.
Next, there are several methods for diagnosing autonomic nervous disorder. One of them is the study of heart rate variability.
The patient performs a simple load: first he lies on his back, and after a few minutes he gets to his feet. In this way, we simulate a standard everyday situation when the minimum load is placed on our body. During this time, sensors attached to the patient's chest record the rhythm of his heart, and the doctor then compares the changes in rhythm in both positions. Such a study shows how adapted the human body is to the usual minimum load, which our autonomic nervous system normally copes with every day without the slightest difficulty.
How it works?
In a healthy state, our body responds adequately to any “stress”, any load (mental, physical, emotional). Therefore, when a healthy person gets up, the sympathetic part of the autonomic nervous system is activated in his body and the hormone adrenaline is produced, which means the heartbeat quickens. When a person lies down, his body should normally be in the mood for rest and relaxation. At the physiological level, this manifests itself as follows: the parasympathetic department of the autonomic nervous system becomes active and the hormone acetylcholine is released, which extinguishes the activity of adrenaline, and a phase of relaxation and replenishment of the body’s reserves begins.
But in patients with symptoms of panic attacks, an abnormal change in heart rhythms is observed: that is, when a person lies down, his pulse quickens and becomes faster and faster. That is, when a person gives his body the command to tune in to rest, the body understands the opposite - and prepares to run a short distance race. This is why people with disorders of the autonomic nervous system so often cannot sleep at night and never feel rested and alert.
Thus, the doctor concludes that the harmonious functioning of the sympathetic and parasympathetic parts of the nervous system is disrupted. This means you can move on to the next stage of the examination.
Among the innovative methods for diagnosing panic disorder are studies of the autonomic nervous system using infrared thermography. In an infrared image, a thermal imager clearly shows in which nodes (ganglia) of the autonomic nervous system the work is disrupted. It is with these vegetative nodes that the neurologist-vegetologist will subsequently work.
“Serious scientific research over the last decade has shown the high reliability and reliability of thermography. This allows this method to be used in medical practice to make a diagnosis in complex cases,” James Mercer, Professor, President of the European Thermography Society (EAT).
| Fig. 1 – Thermal image before treatment of panic attacks and VSD – the functioning of the vegetative node in the cervical region is disrupted (colors – red and orange) | Fig. 2 - Thermal image of the same patient after treatment of panic attacks and VSD - the temperature in the vegetative node of the cervical spine has returned to normal (colors - blue and green) |
After treatment, you can take a repeat infrared photo, in which you will notice progress from the completed course. Areas with abnormal temperatures (bright red or dark blue) will change color in the image because their temperature regime is closer to normal.
Analogs of the drug Atarax
In the pharmacy you can find the following analogues of the drug: Hydroxyzine, Phenazepam, Grandaxin, Anvifen.
Analogs of the drug Atarax
Remember that the prescription of an analogue or replacement of one drug with another is made exclusively by the attending physician, who can correlate the nature of the disease, the desired effect of taking the drug, contraindications, adverse reactions and dosage.
Atarax is sometimes compared to Phenibut. But this is not entirely true.
Atarax or Phenibut?
Phenibut is a nootropic drug that improves cognitive abilities and has a mild tranquilizing effect. This drug effectively relieves anxiety, psycho-emotional stress, and improves sleep. But Atarax is a tranquilizer, most often used to relieve itching, reduce anxiety and psychomotor agitation.
The effect of atarax on depression
Marya
922 views
September 28, 2021
I have been treated for depression for a long time and without success. The last time the doctor prescribed atarax, stopping Phenibut. I felt even worse and I returned the phenibut myself after 5 days. The doctor increased the dose of Atarax and left Phenibut. I've been taking this for two days, but there is no improvement. Can this treatment work over time, or, since everything is bad, is it not suitable? Before this, treatment with the following drugs did not work for me: - serenata with phenibut (7 months of treatment there was apathy, all feelings disappeared, decreased libido, after stopping taking it, gradually on the doctor’s recommendation, the terrible condition returned and I could not go to the psychiatrist again for a year), - azafen and phenibut (from the beginning of taking the condition worsened and was bad all the time, for more than a month, although sometimes it became better without pills, there were good days), - mirtazapine (from half a pill a nightmare began to happen to me - rage, aggression, tears, something happened panic attack, passed within a day), - Grandaxin, Phenibut and Picamilon (I started taking this during a more or less calm period, so at first everything was fine, then it started to get worse, the doctor stopped Picamilon and increased Grandaxin to 3 tablets a day, and it started nightmare, terrible aggression constantly), - atarax (at first the doctor prescribed 1 tablet in the evening, after stopping phenibut, from the next day I practically didn’t live at all, in the morning tears began, unwillingness to live, weakness, I couldn’t do anything, I didn’t go anywhere, I couldn’t plan something to improve the situation, then after 5 days I thought of returning Phenibut, 3 tablets a day, it became not so bad, but still bad, after increasing the dose of Atarax to 3 tablets, there has been no improvement for two days, although they write that atarax acts immediately. My symptoms: anxiety, depression, reluctance to live, frequent tears, hysterics, fits of rage, aggression, apathy, inability to take any action. All this has always been with me, it seems to me, since childhood, it worsened in adolescence, after 30 years I started doing yoga, and the symptoms went away for more than 7 years, they returned in 2017 after the birth of a child. After treatment with serenata, feelings for all of the above disappeared, only feelings of grief and anger remained. And I also have nervous overeating (my doctor, it seems to me, doesn’t pay any attention to these complaints at all), I eat even when I don’t feel like it, I have no appetite, it doesn’t taste good - it doesn’t feel mentally better for long, especially from anything fatty and spicy , flour. Physically, this worsens the condition - I have constant heartburn, pain in the stomach and sides, heaviness in the stomach, nausea, I am constantly gaining weight, to make it easier, I drink activated charcoal and laxative teas. It seems to me that my doctor does not understand the seriousness of what is happening to me. And I can’t describe everything “in colors,” because I might cry, and I can’t express emotions in front of strangers; if I cry, I’ll never be able to communicate with this doctor.
The question is closed
depression
psychiatrist
atarax
treatment doesn't help