Vascular tone is the tension of blood vessels, supported by smooth muscles, an important factor in the blood supply to internal organs, one of the tools for general blood circulation. Vascular tone is influenced by the endothelium, the inner layer of blood vessels. Very thin (one cell thick), but plays a significant role in regulating vascular and cardiac tone, as well as in angiogenesis (formation of new vessels) and immune defense.
The fact that the endothelium is formed by a single layer of flat mesenchymal cells should seem to mean its insignificance, “microscopicity”. In fact, it is the largest organ in humans, present in all tissues. It affects blood clotting, kidney filtration, brain nutrition, and many other processes.
How does the endothelium affect vascular tone?
Among the products of endothelial activity, nitric oxide (NO) attracts attention. It regulates vascular tone. The production of nitric oxide increases with increasing pressure at a given vascular site. Blood pressure may rise due to increased physical activity or under the influence of certain hormones (for example, acetylcholine).
Increased pressure on the vessel wall activates a special set of enzymes called endothelial nitric oxide synthase (eNOS). These enzymes spur increased production of NO. Nitric oxide molecules are freely released through cell membranes and penetrate into smooth muscle. Under the influence of NO, muscle tissue relaxes - the walls of blood vessels, without encountering resistance from smooth muscles, expand, and the pressure inside these vessels drops.
A decrease in pressure weakens eNOS activity in the endothelium. Less nitric oxide is released - the vascular muscles tense again, maintaining the pressure at the working level.
What normalizes vascular regulation in VSD
Hardening, moderate regular physical activity, and massage help to gradually improve the regulation of blood vessels.
Hardening with cold water should begin with the feet and face. The first 3-4 times - 30 seconds each, then gradually increasing the time of douches to 5 minutes and involving a larger area of the body. To enhance the effect, do contrasting douses, 2-3 changes of cold and hot water, always ending with cold. It is better to start tempering with water in the summer. Hardening is especially effective as a prevention of vascular regulation disorders in children with a tendency to VSD. Before starting hardening procedures, be sure to consult your pediatrician.
A restorative massage improves vascular regulation in all organs, as it activates reflex mechanisms through the skin and muscles. The most effective courses are 7-10 sessions every three months.
Sufficient physical activity would be daily gymnastics lasting 15-20 minutes, aimed at improving flexibility and muscle strength, as well as walking for 30 minutes. The need to expand and contract in response to adequate impulses gradually reinforces the coordinated response of the vessels.
But initially, in the human body with uncoordinated autonomic regulation, there are changes at the cellular level that disrupt energy synthesis. The amino acids glycine, cystine and glutamic acid help return metabolic processes in the cell to normal. They are directly involved in cellular respiration and activate it when there is insufficient activity. Eltacin® contains all three amino acids that are regularly needed by people with VSD.
Muscular regulation of vascular tone
The actively maintained tension assigned to the vessel segment by smooth muscles resists surges in blood pressure and does not allow changes in the internal lumens of the vessels - and, consequently, their capacity. This stabilizes blood circulation within an organ or in a separate area of internal tissue. Regardless of pressure surges, the blood supply here remains uniform.
To ensure such regulation, both parasympathetic nerve connections and myogenic mechanisms are involved. The subtleties of paracrine secretion also have an effect.
Paracrine is the third type of secretion, along with endocrine and exocrine.
- Endocrine cells, which are part of the endocrine glands, produce hormones that are released into the blood. They spread through the circulatory system and act within the body.
- Exocrine cells that make up the exocrine glands produce substances that are secreted outward (sweat, saliva, tears) or into internal cavities (for example, pancreatic juices secreted by the pancreas into the intestines).
- Paracrine cells secrete substances that are directly consumed by neighboring cells.
Such close transmission is important, for example, for the development of a receptor response of local cells to the effects of regulatory hormones delivered along with the blood flow.
Brakes and accelerators of vascular tone
Hormones produced by the adrenal medulla circulating along with the blood are important for maintaining tone (especially of peripheral vessels). Adrenaline is well known. But to maintain vascular tone, norepinephrine, which is the biological precursor of adrenaline, is more important. It has a more active effect on blood vessels - but is much gentler on the heart, bronchi and intestines, and does not harm metabolism.
Norepinephrine regulates both blood pressure and peripheral vascular resistance. If the position of the body changes abruptly (for example, a person is lying down and suddenly stands up), the amount of norepinephrine increases many times. It strongly constricts the blood vessels - this maintains the pressure inside the arteries, which, in theory, should drop when the body is transferred from a horizontal to a vertical position (it is one thing if the blood spreads horizontally, another thing when it needs to be pumped upward).
An increased level of norepinephrine affects the vascular muscles - it stabilizes the blood vessels. But with an increase in its level, the reaction of presynaptic adrenergic receptors slows down - which immediately leads to a sharp decrease in the secretion of norepinephrine. The pressure in the arteries is regulated, and there is no longer a need for smooth muscles to compress the vessels. Consequently, there is no need for norepinephrine - it “calms down”. Self-regulation of pressure is due to self-regulation of functions for the production of norepinephrine.
This is a very complex biochemical balance; its maintenance involves not only the hormones dopamine and tyrazine, from which norepinephrine is synthesized, but also adenosine, acetylchodine, histamine, serotonin, prostaglandin, and angeotensin. Moreover, if some hormones (angeotensin) spur the synthesis of norepinephrine, others (prostaglandin, etc.), on the contrary, inhibit it. The process develops cyclically, under the influence of brakes and accelerators.
This “device” is very important for vascular areas that are characterized by frequent and sudden changes in pressure.
The reaction of smooth muscles that regulate pressure in blood vessels is also ensured by the content of ion exchange. The positive ions of potassium and calcium are of particular importance. Their complex transformations in interaction with arachidonic acid and substances stimulate contraction (contraction) or relaxation of vascular muscles, adapting to pressure surges.
Vascular stenosis
Atherosclerosis
Diabetes
Ulcer
5391 12 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vascular stenosis: causes, symptoms, diagnosis and treatment methods.
Definition
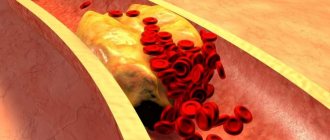
Vascular stenosis (Greek στενός - “narrow, cramped”) is a partial or complete persistent narrowing of the lumen of blood vessels with limitation or complete cessation of blood flow.
Causes of vascular stenosis
Depending on which vessels are affected, a distinction is made between stenosis of arterial vessels (aorta, arteries, arterioles) and stenosis of venous vessels (superior vena cava, inferior vena cava, veins, venules).
Vascular stenosis can be either congenital or acquired.
The main cause of acquired stenosis of the aorta, arteries of the lower extremities, and coronary arteries of the heart is atherosclerosis, a systemic metabolic disease with predominant damage to the vascular wall. The degree of narrowing of the artery and its length may vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, as a result, the blood clotting process is activated and a blood clot is formed.
Blockage of the vessel can lead to ischemia or necrosis of the tissue or organ.
Risk factors for the development of atherosclerosis include:
- male gender;
- elderly age;
- smoking;
- dyslipidemia (violation of the normal ratio of blood lipids);
- diabetes,
- arterial hypertension,
- increased blood homocysteine;
- elevated levels of C-reactive protein (CRP);
- increased blood viscosity and hypercoagulable states;
- chronic renal failure.
Another disease leading to arterial stenosis is obliterating endarteritis (spontaneous gangrene) - a chronic disease of peripheral blood vessels (mainly affecting the arteries of the feet and legs).
Mostly men under the age of 25-40 are affected. Those at risk include smokers, as well as people with frostbite on their feet. Diabetic angiopathy, characterized by damage to both small vessels and large and medium-sized arteries, develops in patients with diabetes mellitus. In diabetic macroangiopathy, when large blood vessels are affected, changes characteristic of obliterating atherosclerosis are found in the wall of the great vessels. With microangiopathies, when small blood vessels are affected, thickening of the walls of microvasculature vessels (arterioles, capillaries, venules) occurs, which leads to a narrowing of the lumen and deterioration of the blood supply to organs and tissues.
Coarctation of the aorta (congenital segmental narrowing of part of the aorta that obstructs blood flow) occurs as a result of improper fusion of the aortic arches in the embryonic period. The length of the narrowing is usually 1-2 cm. The ascending aorta and branches of the aortic arch expand, their diameter increases significantly, and the walls of the arteries participating in the collateral circulation become thinner. Two modes of blood circulation are formed in the systemic circle: up to the point of obstruction to blood flow there is arterial hypertension, and distal (or below) there is hypotension.
Venous stenosis most often occurs as a result of direct damage to the vascular wall during catheter insertion and is then aggravated by the constant presence of a foreign body and mechanical irritation. Inflammation and activation of the blood coagulation system are observed in the vessel wall. These changes lead to proliferation (multiplication) of smooth muscle cells, thickening of the vein wall, and the formation of microthrombi.
Thus, risk factors for the development of central venous stenosis are: the use of a central venous catheter, infections associated with the installation of a catheter, and concomitant diseases.
Systemic vasculitis, tumor diseases and other causes of vascular stenosis are detected much less frequently.
Classification of the disease
According to the type of blood vessels:
- arterial stenosis;
- venous stenosis
Due to the occurrence:
- congenital;
- acquired.
By localization:
- Stenosis of the arteries of the lower extremities.
- Stenosis of the carotid (carotid) and cerebral arteries.
- Stenoses of the arteries of internal organs:
- renal arteries,
- mesenteric arteries etc.
- Aortic stenosis.
- Stenosis of coronary vessels.
By caliber of damage:
- stenosis of large vessels (aorta and its branches);
- stenosis of medium-diameter vessels;
- stenosis of small vessels (arterioles and capillaries).
Symptoms of vascular stenosis
Damage to the blood vessels of the brain is one of the main causes of mortality and disability in the population. 2/3 of ischemic strokes are associated with narrowing and deformation of the carotid arteries.
The risk of developing ischemic stroke is directly related to the degree of narrowing of the artery lumen.
Occlusion (closure) of the internal carotid artery leads to the development of stroke in 40% of cases.
Damages to the blood vessels of the brain can occur in several forms:
- The asymptomatic form is characterized by the absence of focal and cerebral neurological symptoms (impaired consciousness, headache, vomiting, slow pulse).
- Discirculatory encephalopathy is characterized by a predominance of general cerebral symptoms; focal neurological symptoms are absent or appear in a very mild form.
- Transient ischemic attacks manifest themselves in the form of transient disorders of cerebral circulation of the ischemic type and are accompanied by the appearance of focal neurological symptoms that resolve within 24 hours.
- The consequences of a minor stroke are an acute ischemic cerebrovascular accident with the development of neurological symptoms, which almost completely regress within a month as a result of conservative therapy.
- The consequences of a completed stroke are an acute ischemic disorder of cerebral circulation, accompanied by the development of persistent focal neurological and cerebral symptoms.
- Ischemic stroke is damage to brain tissue with disruption of its functions due to obstruction or cessation of blood flow.
Atheroslerotic lesion of the coronary arteries of the heart is manifested by angina pain, but can sometimes be perceived by the patient as discomfort, a feeling of heaviness, compression, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum; it can radiate (give) to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes. Pain with angina pectoris usually lasts from 1 to 15 minutes. Occurs during significant physical or emotional stress. After taking nitroglycerin or stopping the exercise, the pain stops. As angina progresses, an attack may occur with minimal exertion and then at rest.
The main symptom of renal artery stenosis is a persistent increase in blood pressure, which is difficult to respond to drug therapy. Approximately 90% of cases of renal artery stenosis are caused by atherosclerosis; in 10% of cases, stenosis occurs due to fibromuscular dysplasia, a group of diseases that affect the walls of the arterial vessel.
With renal artery stenosis, the blood supply to the kidney tissue is reduced, hormonal factors (renin-angiotensin-aldosterone system) that regulate blood volume and blood pressure are activated, and the development of chronic kidney disease is accelerated.
Stenosing damage to the vessels supplying blood to the abdominal organs (mesenteric arteries) is more often observed in middle-aged and elderly people and manifests itself as chronic abdominal ischemia syndrome, so the main complaint of patients is pain, which appears after 20-25 minutes. after eating, lasts 1-2 hours and usually subsides on its own. The pain can be localized in the epigastric region, directly under the xiphoid process, and radiate to the right hypochondrium or spread from the periumbilical region throughout the abdomen. Some patients note a feeling of constant heaviness in the abdomen, and vomiting is rarely observed.
Other symptoms of chronic abdominal ischemia are intestinal dysfunction, expressed by disturbances in its motor, secretory, absorption functions, and progressive weight loss.
Obliterating atherosclerosis of the aorta and main arteries of the lower extremities is more common in men over 40 years of age and deprives them of their ability to work. The process can be localized in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal).
Small atherosclerotic lesions of the arteries of the lower extremities may not be clinically manifest. With continued vasoconstriction, intermittent claudication occurs, which is manifested by discomfort or pain in the muscles of the lower limb during physical activity. Damage to the terminal aorta and iliac arteries can cause pain in the buttocks, thigh, and calf. Impaired patency of the femoral-popliteal segment is characterized by pain in the calf. Occlusion of the arteries of the leg usually causes pain in the calf, foot, absence or decrease in skin sensitivity in them.
With obliterating endarteritis, trophic disorders are observed (cracks, dry skin, brittle nails, ulcers), intermittent claudication, leg pain, necrosis and gangrene of the limb.
In the generalized form of obliterating endarteritis or atherosclerosis, not only the vessels of the extremities are affected, but the visceral branches of the abdominal aorta, branches of the aortic arch, cerebral and coronary arteries.
The clinical picture of diabetic macroangiopathy consists of the clinical picture of microangiopathy and atherosclerosis of the great vessels, but is characterized by a more severe and progressive course, often ending in gangrene.
The clinical picture of diabetic microangiopathy of the lower extremities is similar to that of obliterating endarteritis.
With coarctation of the aorta, symptoms depend on the severity of the disease. In the case of significant narrowing of the aorta, the parents of the newborn pay attention to the pale skin, sweating, and difficulty breathing of the child. In older children and adults, the symptoms are usually mild: high blood pressure, headache, cold extremities, nosebleeds.
Stenosis of the central veins is clinically manifested by swelling of the extremities, pain in them and trophic changes (cyanosis, thinning of the skin, cracks, ulcers, etc.).
Diagnosis of vascular stenosis
Diagnosis of the disease is based on the analysis of patient complaints, medical history data, clinical picture, data from laboratory and instrumental research methods.
To clarify the cause of vascular stenosis, the following may be recommended:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);
Regulation of vascular tone through surrounding tissue
The neighboring tissue, which is supplied with blood through these vessels, also participates in pressure regulation. Metabolic factors that arise in the tissue during energy production or, conversely, during its consumption, affect blood vessels. The channel for such an effect is either the endothelium or vascular smooth muscle. Reactions of the endothelium and smooth muscles lead to the expansion or contraction of blood vessels, which normalizes the pressure inside them.
In addition to direct metabolic products, blood vessels can also be affected by other factors related to tissue functions. For example, skeletal muscle secretes the enzymes nitric oxide (NO synthase) and cyclooxygenase (COX). This is in addition to "pure" nitric oxide and prostaglandins, which are also typical of skeletal muscle. During heavy physical activity (that is, with regular tension of the striated muscles), these products are released in particularly large quantities, can reach local vessels, affect their tension or elastic relaxation of the walls, the width of the internal lumen, and pressure.
The extent of this influence (significant or insignificant) is not yet known to pathologists. Various hypotheses have been put forward - but be that as it may, the influence of skeletal muscles on the regulation of vascular tone cannot be excluded.
Moreover, new factors of such influence are constantly being identified. Thus, it became known that certain cells that make up the heart muscle (cardiomyocytes) also regulate vascular tone in their own way. These cells also secrete nitric oxide (NO), which spreads through the internal tissues to the vessels, primarily the coronary vessels. Thus, the heart regulates the pressure inside the vessels not only by supplying blood, but also additionally, through nitric oxide, making the lumens of the vessels optimal for a specific level of blood flow.
How to normalize cerebral vascular tone
To normalize the activity of blood vessels that supply the brain with oxygen, you need a balanced diet, an active and healthy lifestyle, good sleep, moderate physical activity, and hardening.
At home, you can temporarily relieve the painful and unpleasant sensations associated with the occurrence of spasms, but treatment of cerebral vessels must be started as early as possible to prevent the occurrence of a stroke.
You can consult and get recommendations from highly professional specialists at Minimax. For the Minimax company, the health and well-being of clients is the most important priority and goal of its activities.