Psychomotor agitation occurs during acute mental disorders and is manifested by increased motor activity, which can be accompanied by confusion, anxiety, aggressiveness, fun, hallucinations, confusion, delirium, etc. Read more about what this condition is, why it can occur and how it is treated will be discussed later in the article.
Main signs of psychomotor agitation
The state of psychomotor agitation is characterized by an acute onset, a pronounced disturbance of consciousness and motor restlessness (this can be either fussiness or destructive impulsive actions). The patient may experience euphoria or, on the contrary, anxiety and fear.
His movements acquire a chaotic, inadequate character, they may be accompanied by speech excitement - verbosity, sometimes in the form of a continuous stream of words with shouting of individual sounds or phrases. The patient may be haunted by hallucinations, he experiences clouding of consciousness, and his thinking becomes accelerated and disorganized (dissociative). Aggression occurs, directed both at others and at oneself (suicidal attempts). By the way, the patient has no criticism of his condition.
As is clear from the listed symptoms, the patient’s well-being is dangerous and requires urgent medical attention. But what could lead to this state of affairs?
Symptoms of nervous excitement.
Perhaps the main symptom of nervous excitability
is insomnia, especially if a person has difficulty falling asleep for three to four hours, without finding a comfortable sleeping position, or loss of sleep until the morning in the middle of the night's rest.
In addition, nervous excitement
is characterized by other symptoms, which include a disorder of the motor ability of the eyeballs, lack of orientation in space and time, loss of symmetry of the facial muscles, awkward and uncollected movements, frequent headaches, and delayed intellectual development.
Causes of psychomotor agitation
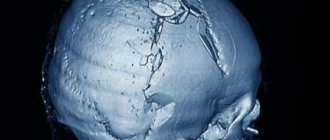
Acute psychomotor agitation can be provoked by a variety of reasons, both severe stress and organic brain damage (for example, epilepsy).
Most often it occurs:
- when a mentally healthy person remains in a state of panic for a long time or as a result of a life-threatening situation he has suffered (for example, after a car accident, so-called reactive psychosis may develop);
- for acute or chronic alcohol intoxication, as well as for poisoning with caffeine, quinine, atropine, etc.;
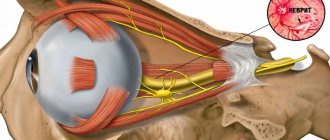
- after emerging from a comatose state or after traumatic brain injuries that provoked pathological damage to areas of the brain;
- may be a consequence of damage to the central nervous system by toxins, as a result of a severe infectious disease;
- with hysteria;
- often occurs in mental illnesses: schizophrenia, depressive psychosis, manic agitation or bipolar affective disorder.
Network congestion
Figure 3. Structure of memantine. Memantine is a derivative of the hydrocarbon adamantane (not to be confused with adamantine). Drawing from Wikipedia.
In a normally functioning brain, signals from neurons are distributed evenly across all other cells. Neurotransmitters are released in the required quantities, and there are no damaged cells. However, after a stroke (acute lesion) or during dementia (a long-term process), glutamate begins to be released from neurons into the surrounding space. It stimulates the NMDA receptors of other neurons, and calcium flows into these neurons. The influx of calcium triggers a number of pathological mechanisms, which ultimately leads to the death of the neuron. The process of cell damage due to the release of large amounts of endogenous toxin (in this case, glutamate) is called excitotoxicity.
Figure 4. Effect of memantine in Alzheimer's dementia. Memantine reduces the intensity of excitatory signals that come from cortical neurons to the Meynert nucleus. The acetylcholine neurons that make up this structure regulate attention and a number of other cognitive functions. Reducing excess activation of Meynert's nucleus leads to a decrease in symptoms of dementia. Figure from [6].
In order to prevent the development of excitotoxicity or reduce its impact on the course of the disease, memantine can be prescribed. Memantine is a very attractive NMDA receptor antagonist molecule (Fig. 3). Most often, this drug is prescribed for vascular dementia and dementia due to Alzheimer's disease. Normally, NMDA receptors are blocked by magnesium ions, but when stimulated by glutamate, these ions are released from the receptor, and calcium begins to enter the cell. Memantine blocks the receptor and prevents the passage of calcium ions into the neuron - the drug exerts its neuroprotective effect by reducing the overall electrical “noise” in cell signals. In Alzheimer's dementia, in addition to glutamate-mediated problems, the level of acetylcholine, a neurotransmitter involved in processes such as memory, learning and attention, decreases. Because of this feature of Alzheimer's disease, psychiatrists and neurologists use inhibitors of acetylcholinesterase, an enzyme that breaks down acetylcholine in the synaptic cleft, for treatment. The use of this group of drugs increases the content of acetylcholine in the brain and normalizes the patient’s condition [5]. Experts recommend the combined administration of memantine and acetylcholinesterase inhibitors to more effectively combat dementia in Alzheimer's disease [6]. When these drugs are used together, there is an impact on two mechanisms of disease development at once (Fig. 4).
Dementia is a long-term brain disorder in which neurons die slowly. And there are diseases that lead to rapid and large-scale damage to nervous tissue. Excitotoxicity is an important component of nerve cell damage in stroke. For this reason, in cases of cerebrovascular accidents, the use of memantine may be justified, but research on this topic is just beginning. Currently, there is work done on mice showing that administration of memantine at a dose of 0.2 mg/kg per day reduces the volume of brain damage and improves the prognosis of stroke [7]. Perhaps further work on this topic will improve the treatment of strokes in humans.
Degrees of severity of psychomotor agitation
In medicine, psychomotor agitation is divided into three degrees of severity.
- Mild degree. Patients in this case only look unusually animated.
- The average degree is expressed in manifestations of lack of purpose in their speech and actions. Actions become unexpected, pronounced affective disorders appear (gaiety, anger, melancholy, malice, etc.).
- A sharp degree of excitement is manifested by extreme chaotic speech and movements, as well as clouding of consciousness.
By the way, how this excitement manifests itself depends to a large extent on the age of the patient. Thus, in childhood or old age it is accompanied by monotonous speech or motor acts.
In children, this is monotonous crying, screaming, laughing or repeating the same questions, rocking, grimacing or smacking is possible. And in elderly patients, excitement manifests itself as fussiness, with an air of businesslike concern and complacent talkativeness. But in such situations, manifestations of irritability or anxiety, accompanied by grumpiness, are also common.
Types of psychomotor agitation
Depending on the nature of the patient’s excitation, different types of this condition are differentiated.
- Hallucinatory-delusional arousal – characterized by feelings of fear, anxiety, confusion or anger and tension. Patients can talk to an invisible interlocutor, answer their questions, listen to something, and in other cases - attack imaginary enemies or, on the contrary, flee from them, not understanding the road and obvious obstacles.
- Catatonic psychomotor agitation - its symptoms manifest themselves in the randomness and lack of purposefulness of the patient's movements - they are sudden, meaningless and impulsive, with transitions from excitement to stupor. The patient is foolish, grimaces, behaves ridiculously and mannered.
- Manic excitement is expressed by transitions from gaiety to anger, irritability and malice. The patient cannot sit still - he sings, dances, interferes in everything, takes on everything and does not complete anything. He speaks quickly, continuously, constantly changing the topic and not finishing sentences. He clearly overestimates his capabilities, can express ideas of greatness, and show aggression when objecting.
Several more types of psychomotor agitation
In addition to those listed above, there are several other types of psychomotor agitation that can develop in both a healthy person and someone with organic brain damage.
- Thus, epileptic agitation is characteristic of the twilight state of consciousness in patients with epilepsy. It is accompanied by an angry-aggressive affect, complete disorientation, and the impossibility of contact. Its beginning and end, as a rule, are sudden, and the condition can reach a high degree of danger for others, since the patient can attack them and cause severe damage, as well as destroy everything that he encounters along the way.
- Psychogenic psychomotor agitation occurs immediately after acute stressful situations (disaster, wreck, etc.). It is expressed by varying degrees of motor restlessness. This can be monotonous excitement with inarticulate sounds, or chaotic excitement with panic, flight, self-mutilation, and attempted suicide. Often excitement gives way to stupor. By the way, during mass disasters, a similar state can affect large groups of people, becoming common.
- Psychopathic arousal is superficially similar to psychogenic, since it also occurs under the influence of external factors, but the strength of the response in this case, as a rule, does not correspond to the cause that caused it. This condition is associated with the psychopathic characteristics of the patient’s character.
Molecules and bonds
Glutamate (glutamic acid) is one of the 20 essential amino acids. In addition to participating in protein synthesis, it can serve as a neurotransmitter - a substance that transmits a signal from one nerve cell to another in the synaptic cleft. It should be taken into account that glutamate, which is in food, does not penetrate the blood-brain barrier, that is, it does not have a direct effect on the brain. Glutamate is formed in the cells of our body from α-ketoglutarate by transamination. An amino group is transferred from alanine or aspartate, replacing the ketone radical of α-ketoglutarate (Figure 1). As a result, we get glutamate and pyruvate or oxaloacetic acid (depending on the amino group donor). The last two substances are involved in many important processes: oxaloacetic acid, for example, is one of the metabolites in the great and terrible Krebs cycle. The destruction of glutamate occurs with the help of the enzyme glutamate dehydrogenase, and during the reaction the already familiar α-ketoglutarate and ammonia are formed.
Figure 1. Glutamate synthesis. Glutamate is formed from α-ketoglutarate by replacing the keto group with an amino group. When carrying out the reaction in cells, nicotinamide adenine dinucleotide phosphate (NADP) is consumed. Figure from lecturer.ukdw.ac.id.
Glutamate, like most other mediators, has two types of receptors - ionotropic (which open a membrane pore for ions in response to the addition of a ligand) and metabotropic (which, when a ligand attaches, causes metabolic changes in the cell). The group of ionotropic receptors is divided into three families: NMDA receptors, AMPA receptors and kainic acid receptors. NMDA receptors are so called because their selective agonist, a substance that selectively stimulates these receptors, is N-methyl-D-aspartate (NMDA). In the case of AMPA receptors, this agonist is α-aminomethylisoxazolepropionic acid, and kainate receptors are selectively stimulated by kainic acid. This substance is found in red algae and is used in neuroscience research to model epilepsy and Alzheimer's disease. Recently, δ receptors have also been added to ionotropic receptors: they are located on Purkinje cells in the mammalian cerebellum. Stimulation of the “classical” - NMDA-, AMPA- and kainate - receptors leads to the fact that potassium begins to leave the cell, and calcium and sodium enter the cell. During these processes, excitation occurs in the neuron and an action potential is triggered. Metabotropic receptors are associated with the G-protein system and participate in the processes of neuroplasticity [1]. Neuroplasticity refers to the ability of nerve cells to form new connections with each other or destroy them. Also included in the concept of neuroplasticity is the ability of synapses to change the amount of neurotransmitter released depending on what behavioral acts and mental processes are occurring at the moment and with what frequency.
The glutamate system is nonspecific: almost the entire brain “works” on glutamic acid. Other neurotransmitter systems described in previous articles had more or less narrow specificity - for example, dopamine influenced our movements and motivation [2]. In the case of glutamate, this does not happen - its influence on processes inside the brain is too broad and indiscriminate. It is difficult to single out any specific function other than exciting. For this reason, we have to talk about the glutamate system as a collection of a large number of connections in the brain. This collection is called a connectome. The human brain contains a huge number of neurons, which form an even larger number of connections among themselves. Compiling a human connectome is a task that is currently beyond the capabilities of science. However, the connectome of the worm Caenorhabditis elegans has already been described [3] (Fig. 2). Fans of the connectome idea argue that human connectomes record our identity: our personality and memory. In their opinion, our “I” is hidden in the totality of all connections. “Signalers” also believe that after describing all the neural connections, we will be able to understand the cause of many mental and neurological disorders, and therefore will be able to successfully treat them.
Figure 2. Connectome of the nematode Caenorhabditis elegans Each neuron of the worm has its own name, and all connections between neurons are taken into account and plotted on the diagram. As a result, the diagram turns out to be more confusing than a map of the Tokyo subway. Picture from connectomethebook.com.
It seems to me that this idea is promising. In a simplified form, connections between neurons can be represented in the form of wires, complex cables connecting one neuron to another. If these connections are damaged—the signal is distorted, the wires are broken—the coherent functioning of the brain may be disrupted. Such diseases that occur when there is a failure in neural communication channels are called connectopathies. The term is new, but it hides pathological processes already known to scientists. If you want to learn more about connectomes, I recommend reading Sebastian Seung’s book “Connectome. How the brain makes us what we are" [4].
How to provide emergency care for acute psychomotor agitation
If a person exhibits psychomotor agitation, emergency assistance is necessary immediately, since the patient can injure himself and others. To do this, all strangers are asked to leave the room where he is located.
They communicate with the patient calmly and confidently. It should be isolated in a separate room, which is first inspected: windows and doors are closed, sharp objects and anything that can cause a blow are removed. A psychiatric team is urgently called.
Before her arrival, you should try to distract the patient (this advice does not apply to the twilight state, since the patient is not contactable), and, if necessary, immobilize.
Providing assistance in immobilizing the patient
Psychomotor agitation, the symptoms of which were discussed above, often requires the use of restraint measures. This usually requires the help of 3-4 people. They approach from behind and from the sides, hold the patient's arms pressed to the chest and sharply pick him up under the knees, thus placing him on a bed or couch, previously moved away from the wall so that it can be approached from 2 sides.
If the patient resists by waving an object, then assistants are recommended to hold blankets, pillows or mattresses in front of them. One of them should throw a blanket over the patient's face, this will help put him on the bed. Sometimes you have to hold your head, for which you throw a towel (preferably damp) over your forehead and pull it to the bed by the ends.
It is important to be careful when holding it to avoid causing damage.
Features of providing assistance with psychomotor agitation
Drug assistance for psychomotor agitation should be provided in a hospital setting. For the period while the patient is transported there, and for the time until the drugs begin to take effect, temporary use of restraint is permitted (which is recorded in medical documents). In this case, the following mandatory rules are observed:
- when applying restraint measures, use only soft materials (towels, sheets, fabric belts, etc.);
- securely fix each limb and shoulder girdle, since otherwise the patient can easily free himself;
- compression of nerve trunks and blood vessels should not be allowed, because this can lead to dangerous conditions;
- The fixed patient is not left unattended.
After the effect of neuroleptics, he is released from fixation, but observation should be continued, since the condition remains unstable and a new attack of excitement may occur.
Voices in my head
Schizophrenia is another disease in which targeting the brain's glutamate system is a new and promising treatment option. Currently, the main cause of the development of schizophrenia is considered to be a violation of dopamine transmission in the brain. An excess of dopamine in some parts of the nervous system leads to delusions and hallucinations, while a deficiency in others leads to apathy, depression and lack of motivation. Antipsychotics—drugs that block dopamine receptors—are good for hallucinations and delusions, but have problems with another group of symptoms. The limited clinical effect of antipsychotics indicates that other neurotransmitter systems may be involved in the development of schizophrenia.
If the glutamate system is involved in schizophrenia, then this could be tested even in healthy people. If healthy subjects are administered drugs that block the action of glutamate (ketamine, amphetamine), they develop symptoms of schizophrenia [8]. The administration of ketamine to patients with schizophrenia led to the re-emergence of psychosis with the repetition of symptoms typical for the patient, that is, ketamine did not cause “just psychosis”, but returned the hallucinations and delusions that were there before [9]. This contradiction between the two hypotheses complicates the already complex picture of the neurobiological basis of schizophrenia. Psychotic symptoms with ketamine administration can be explained by its ability to influence dopamine receptors. Another explanation could be that dopamine and glutamate neurons are capable of influencing the striatum. This part of the brain is actively involved in the “production” of hallucinations [10].
The most common hallucinations in patients with schizophrenia are auditory: the patient hears “voices” in his head. The voice can scold and comment on what is happening around, including the patient’s actions. One of my patients had “voices” reading store signs on the street she was walking; another heard a voice say: “Get your pension and let’s go to the cafe.” There is currently a theory that explains the emergence of such voices. Let's imagine that the patient is walking down the street. He sees a sign, and the brain automatically “reads” it. With increased activity in the temporal lobe, which is responsible for auditory perception, the patient experiences auditory sensations. They could be suppressed due to the normal functioning of areas of the frontal cortex, but this does not happen due to a decrease in their activity (Fig. 5). Excessive activity in the auditory cortex may be caused by hyperfunction of the glutamate (excitatory) system or a defect in the GABAergic structures responsible for normal inhibition in the human brain. Most likely, insufficient activity of the frontal lobe in the case of schizophrenia is also associated with an imbalance of neurotransmitters. Inconsistency in actions leads to the fact that a person begins to hear “voices” that clearly relate to the environment or convey his thoughts. Very often we “speak” our thoughts in our heads, which can also be the source of “voices” in the brain of a person with schizophrenia [11].
Figure 5. Occurrence of auditory hallucinations in the brain of a patient with schizophrenia. The primary sensation of automatically “reading” signs or having thoughts, located in the temporal cortex (1), is not suppressed by the frontal cortex (2). The parietal cortex (3) picks up the emerging pattern of activity in the brain and shifts the focus of activity to it. As a result, a person begins to hear a “voice”. Figure from [12].
This concludes our journey into the world of neurotransmitters. We met the motivating dopamine, the calming γ-aminobutyric acid, and four more heroes of our brain. Be interested in your brain - because, as the title of Dick Swaab's book says, we are our brains .
Treatment of psychomotor agitation
To relieve the severity of an attack, a patient with any psychosis is given sedatives: “Seduxen” - intravenously, “Barbital-sodium” - intramuscularly, “Aminazine” (iv or i.m.). If the patient can take drugs orally, then he is prescribed Phenobarbital, Seduxen or Aminazine tablets.
The antipsychotics Clozapine, Zuk-lopentixol and Levomepromazine are no less effective. It is very important to monitor the patient’s blood pressure, since these drugs can cause a decrease in it.
In a somatic hospital, treatment of psychomotor agitation is also carried out with drugs used for anesthesia (Droperidol and sodium hydroxybutyrate solution with glucose) with mandatory monitoring of respiration and blood pressure. And for weakened or elderly patients, tranquilizers are used: Tiapride, Diazepam, Midazolam.
Literature
- Meldrum B. S. (2000). Glutamate as a neurotransmitter in the brain: review of physiology and pathology. J. Nutr. 130 , 1007S–1015S;
- Dopamine diseases;
- Varshney LR, Chen BL, Paniagua E, Hall DH, Chklovskii DB (2011). Structural properties of the Caenorhabditis elegans neuronal network. PLoS Comput. Biol. 7 (2), e1001066;
- Seung S. Connectome. How the brain makes us who we are. M.: Binom, 2014 - 440 pp.;
- The molecule of sanity;
- Parsons C. G., Danysz W., Dekundy A., Pulte I. (2013). Memantine and cholinesterase inhibitors: complementary mechanisms in the treatment of Alzheimer's disease. Neurotox. Res. 24, 358–369;
- Trotman M., Vermehren P., Gibson C. L., Fern R. (2015). The dichotomy of memantine treatment for ischemic stroke: dose-dependent protective and detrimental effects. J. Cereb. Blood Flow Metab. 35, 230–239;
- Krystal JH, Perry EB Jr, Gueorguieva R, Belger A, Madonick SH, Abi-Dargham A et al. (2005). Comparative and interactive human psychopharmacologic effects of ketamine and amphetamine. Implications for glutamatergic and dopaminergic model psychoses and cognitive function. Arch. Gen. Psychiatry. 62, 985–995;
- Lahti A. C., Koffel B., LaPorte D., Tamminga C. A. (1995). Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. Neuropsychopharmacology 13, 9–19;
- Rolland B., Jardri R., Amad A., Thomas P., Cottencin O., Bordet R. (2014). Pharmacology of hallucinations: several mechanisms for one single symptom? Biomed. Res. Int. 2014 , 307106. doi: 10.1155/2014/307106;
- Hugdahl K. (2015). Auditory hallucinations: A review of the ERC “VOICE” project. World J. Psychiatr. 5, 193–209;
- Hugdahl K., Løberg E.-M., Nygård M. (2009). Left temporal lobe structural and functional abnormality underlying auditory hallucinations in schizophrenia. Front. Neurosci. 3, 34–45..
Use of drugs depending on the type of psychosis
As a rule, a newly admitted patient is prescribed general sedatives, but after the diagnosis has been clarified, further relief of psychomotor agitation will directly depend on its type. Thus, for hallucinatory-delusional excitation, the drugs “Haloperidol” and “Stelazine” are prescribed, and for manic arousal, the drugs “Clopixol” and “Lithium Oxybutyrate” are effective. The reactive state is relieved with the drugs "Aminazin", "Tizercin" or "Phenazepam", and catotonic agitation is cured with the drug "Mazhepril".
Specialized medications are combined, if necessary, with general sedatives, adjusting the dose.
Cupping and treatment options
This mental disorder is not a safe manifestation of psychiatric symptoms in any case. It necessarily poses a danger either for the individual with psychomotor agitation and/or for the environment. It is a very debilitating phenomenon because it has high and inadequate neurotransmitter activity. This phenomenon is stopped in stationary conditions due to the danger of its manifestations for the environment.
Depending on the root cause that caused psychomotor agitation, the accompanying symptoms and approaches to relief vary. Vivid aggressive symptoms with tendencies towards self-harm or external aggression towards the environment most actively require relief. Sometimes there is even a need to record such patients in an examination ward in acute psychiatric wards.
Sometimes, before treating such agitated patients, it is necessary to first catch and detain them. This is not always an easy task, especially when the patient is carrying dangerous items. This requires qualified assistance from trained personnel. In psychiatry there are a large number of ways to catch such patients. But if such an incident with a violent individual occurred outside the walls of a psychiatric hospital, then the most correct and deliberate step would be to call the police, since a doctor should never risk his life so recklessly.
In the relief of psychomotor agitation, it makes sense to talk about the drugs that are used, depending on the underlying pathology that provoked it. For schizophrenia, antipsychotics are used: Rispolept, Soleron, Quetiapine, Solex, Rispaxol. In addition, it is necessary to use correctors to prevent stiffness: Cyclodol, Calcium gluconate. Supportive psychotherapeutic groups can also be used.
In bipolar disorder, excitation can manifest itself in both phases, which greatly influences the selection of the drug. Thymostabilizers are used stably: Valprocom, Depakin, Litosan, lithium carbonate, Lamotrigine.
For depression, it is necessary to use antidepressants: Fluoxetine, Paroxetine, Amitriptyline, Miaser, Imipramine.
Antipsychotics are also used for mania: Ziprasidone, Aripiprazole, Sertindole, Olanzapine, Zyprexa.
For epilepsy, it is necessary to use antiepileptic drugs, and on a regular basis; they also have normotimic properties: Valprocom, Carbamazepine, Depakine.
In case of psychotrauma, the effects of tranquilizing therapy are sufficient: Gidazepam, Phenazepam, Lorazepam, Midazepam, Nozepam. In addition, mandatory psychotherapy is subsequently indicated to help overcome this condition and prevent consequences and neurotic pathologies.