Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is glossopharyngeal neuralgia?
If the cranial nerve is affected by a quarter on one side, and paroxysms of pain appear in the tonsils, soft palate, pharynx and ear, then the patient may have neuralgia of the glossopharyngeal nerve. With this pathology, a violation of the taste perception of the posterior third of the tongue, on the affected side, is detected. Hypersalivation and decreased reflex of the palate and pharynx are also noted. To make a diagnosis, an examination by a neurologist or dentist is required. CT and MRI of the brain are indicated as hardware diagnostic methods. In most cases, treatment is conservative, including:
- Anticonvulsants;
- Analgesics;
- Sleeping pills and sedatives;
- Vitamin therapy;
- Physiotherapy;
- General strengthening procedures.
Diagnosis and treatment of neuralgia of the cranial nerves
Neuralgia is diagnosed by a neurologist; to exclude diseases of the oral cavity, ear, nose and throat, consultations with specialized specialists may be required: otolaryngologist, ophthalmologist and dentist. In order to identify the cause of secondary neuritis, high-tech CT or MRI studies, echo and electroencephalography are prescribed.
The main method of treating cranial neuralgia is conservative therapy and in most cases recovery occurs within 2–3 weeks; in severe cases, the recovery period takes several months. If there is compression of the nerve and muscle paresis, surgery may be required.
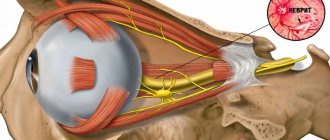
Structure of the glossopharyngeal nerve
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Trigeminal neuralgia - symptoms and treatment
There are two types of pain due to trigeminal neuralgia:
- constant, dull, periodically intensifying pain without wide irradiation, arising in the area of distribution of one or another branch of the nerve and not accompanied by pronounced autonomic reactions;
- pain of a paroxysmal nature, lasting from several minutes to several hours.[4][5]
The intensity of the attacks varies: from mild but frequent, lasting a few seconds, to strong and unbearable, lasting for minutes and causing severe suffering.
Attacks often occur spontaneously, without any irritants, or as a result of hard and cold food getting into the mouth, touching, drafts, hypothermia under air conditioning, jaw movements, etc.
The attack usually begins with pain in one branch of the nerve - the site of the primary lesion, then the pain spreads to other branches, often radiating to the back of the head, to the ear nerves, to the neck and even to the area of the thoracic nerves.
Severe attacks are usually accompanied by autonomic reflex reactions: redness of the face, lacrimation, runny nose, drooling, sometimes swelling of the cheeks, eyelids, and slight swelling of half the nose.
The patient's suffering is manifested by general anxiety, rubbing the painful area with his hand, putting pressure on this area, and smacking his lips. This layering of new stimuli obviously accelerates the moment of the onset of an inhibitory state in the center of pain perception, which usually gives way to an attack.
As motor manifestations in connection with a painful attack, tic-like muscle twitching or spasmodic contractions occur. The maximum twitching or contraction of the muscles corresponds mainly to the zones from which the pain begins, i.e., to the sites of primary damage.
With long-term disease, graying of the scalp hair on the affected side is sometimes observed.
Sometimes paroxysmal neuralgia is accompanied by a rash of herpes zoster (herpes zoster), located according to the primary lesions of certain branches, sometimes affecting the corneal mucosa.
Periods of exacerbations may alternate with periods of remission, which last for months, sometimes years.
Outside of an attack, usually no disorders are observed: no pain points, no objective sensitivity disorders. Sometimes you can notice a decrease in pain sensitivity, mainly in the area of the branch that was the site of the primary lesion. Less commonly, decreased sensitivity is found in the area of all branches of the trigeminal nerve. In some cases, outside of attacks, patients experience mild dull pain. Pain occurs at any time, but more often during sleep.[6][7]
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Medical Internet conferences
Damage to the recurrent nerve as a postoperative complication after surgery on the thyroid gland
Kiseleva E.V.
Scientific supervisor: Doctor of Medical Sciences, Associate Professor Kuligin A.V.
GBOU VPO Saratov State Medical University named after. IN AND. Razumovsky Ministry of Health of the Russian Federation
Department of Emergency and Anesthesiology and Resuscitation Care
The majority of thyroid lesions require surgical treatment, one of the common complications (20%) of which is injury to the recurrent laryngeal nerve.
Purpose of the study. Optimization of diagnosis of damage to the recurrent laryngeal nerve in the postoperative period in patients after surgery on the thyroid gland from the position of an anesthesiologist
Materials and methods. Articles and reports of doctors involved in the diagnosis of intraoperative damage to the recurrent nerve during surgery on the thyroid gland were analyzed. An analysis of diagnostic methods for the identified complication was carried out.
Results. According to the literature, the frequency of this complication varies widely from 0.2 to 15%. Of the data provided by surgeons, it was 3.7%, otolaryngologists - 4.2%, anesthesiologists - 5.7%. In 15%, the identified complication required a tracheostomy. The most common injury to the recurrent nerve was observed during thyroidectomy. Most cases of damage to the recurrent nerve are not diagnosed intraoperatively, and suspicion arises in the immediate postoperative period, with the development of a characteristic clinical picture. Patients complained of difficulty breathing, phonation disturbances, and difficulty speaking. The reliability of these data was influenced by which specialist made the diagnosis of this complication: the operating surgeon, otorhinolaryngologist, or anesthesiologist-resuscitator, as well as based on the clinical picture alone or using instrumental research methods, the diagnosis was established. Treatment of the resulting complication proceeded according to standard generally accepted methods, ending in 77% with complete recovery of patients, but depended on the degree of nerve damage.
Conclusions. An analysis of the literature studied shows that the diagnosis of damage to the recurrent nerve in 80% of cases occurs after surgery and awakening of the patient. The diagnosis is based on the developing clinical picture. Treatment of the identified complication depends on the degree of nerve damage and the severity of clinical symptoms. To optimize the diagnostic search for damage to the recurrent nerve, it is necessary to improve intraoperative diagnostics on the part of the anesthesiologist and otorhinolaryngologist.
Therapy
To treat neuralgia of the glossopharyngeal nerve, conservative therapy is prescribed. The only exception is if the underlying cause is tumors and hypertrophy of the styloid process, leading to compression of the nerve. In these cases, surgery is indicated.
To relieve pain, a 10% solution of cocaine is prescribed, which is applied to the root of the tongue and pharynx. This allows you to eliminate paroxysms for 6-7 hours. If this remedy turns out to be ineffective, a 1-2% novocaine solution is injected into the root of the tongue. Non-narcotic analgesics and anticonvulsants are also prescribed internally. If the pain syndrome is pronounced, it is advisable to prescribe sedatives, hypnotics, antipsychotic medications and antidepressants. AFT, multivitamin complexes and FiBS are used as general strengthening agents.
Among the physiotherapeutic procedures that have proven effectiveness are:
- SMT on the area of the larynx and tonsils;
- Diadynamic therapy;
- Galvanization.