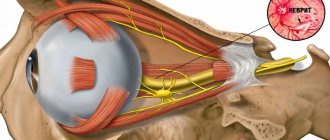
The external, otherwise called lateral, cutaneous nerve of the thigh is formed by nerve fibers emerging from the second and third lumbar spinal roots (LII-LIII, L2-L3). Rushing along the iliacus muscle, it passes under the inguinal (pupart) ligament and extends to the anterior outer femoral surface. In this area, closer to the pelvis, the nerve branches.
The lateral cutaneous nerve of the thigh consists only of sensory fibers, so when it is damaged, muscle function is not impaired.
Neuritis of the lateral cutaneous nerve of the thigh is its inflammatory lesion, the main symptom of which is pain - neuralgia.
Neuropathy of the external cutaneous nerve of the thigh
Neuropathy of the external cutaneous nerve of the thigh: this disease is expressed by damage to the lateral cutaneous nerve of the thigh in the groin area. The most common cause is age-related changes in the body. Neuropathy of the external cutaneous nerve of the thigh expresses itself as a disorder of the sensitivity of the skin, pain and numbness, and walking impairment may occur. The doctor makes a diagnosis after a full examination, and therapy is carried out using medications and physiotherapeutic methods.
NEUROPATHY OF THE PUDENTAL NERVE (nervus (n) pudendus) - pudendoneuropathy
The nerve provides sensitivity in the anus and perineum, is responsible for the work (innervates) the muscles of the perineum, bladder (located in the bladder) and urethral (in the urethra) sphincters (muscles responsible for holding urine).
Neuropathy is manifested by: unilateral pain in the perineal area, sometimes in its anterior parts: in women - in the vaginal area, in men - in the scrotum; sometimes in the posterior regions - in the area of the anus and rectum (anorectal), in the coccyx and buttocks.
In addition to pain, unpleasant sensations of numbness, tingling, and burning may occur in these same areas. Pain and discomfort increase when sitting and decrease when standing.
There may be short delays in urination.
Upon examination, no changes in the perineal area are detected.
Information about the disease
This disease was first described back in 1895 by a neurologist from Russia V.K. Roth and a doctor from Germany M. Bernhardt. Thus, neuropathy of the external cutaneous nerve of the thigh has another name - Bernhardt-Roth disease. Most patients with this diagnosis are over 50 years of age, and the majority are men. Sometimes neuropathy of the external cutaneous nerve of the thigh occurs in pregnant women in the last trimester of pregnancy.
It is worth noting that neuropathy is mostly unilateral, but bilateral nerve destruction can also occur (20%). It is assumed that the pathology can be inherited.
Causes of neuropathy of the external cutaneous nerve of the thigh
The most common cause of the disease is pressure on a nerve in the pelvic area. The pathology can be provoked by the use of a corset, too tight underwear, tight belts, pregnancy or excessive weight. Fractures, injuries, spinal diseases, and neuro-reflex abnormalities can also have an effect. All this leads to irreversible transformations, which involve further rubbing of the nerve against the ligament when a person bends over or moves the hip.
Compression of the lateral cutaneous nerve occurs at the level of the iliacus muscle. Among the root causes may be a hematoma in the abdominal cavity, varicose veins, inflammatory processes, surgery or tumors. The disease can develop against the background of bad habits, such as alcoholism, and other diseases (diabetes mellitus, infections, rheumatism).
Loss of sensation in limbs
Acute loss of sensation in individual limbs can be established in longitudinal zones corresponding to individual nerve roots, or in various areas innervated by individual nerves. The roots are usually damaged as a result of injury by osteophytes of the vertebrae due to spondylosis or herniated disc protrusion. The brachial plexus can be damaged by local trauma (during surgery or an accident involving the shoulder joint area, including birth injuries) and can then become inflamed. The lumbosacral plexus can be damaged during surgery when a retroperitoneal hematoma develops. Peripheral nerves are sensitive to injury or compression in certain classic areas, such as the elbow for the ulnar nerve, the wrist for the median nerve, the knee for the peroneal nerve, and the medial malleolus for the tibial nerve.
Nerve roots
In the upper extremities, reduction or loss of pain and tactile sensation in the first digit and radial surface of the hand raises suspicion of a lesion of the C6 root . A decrease in pain sensitivity on the fourth and fifth fingers, as well as on the ulnar surface of the forearm, indicates damage to the C8 root . If reduced pain sensitivity is detected on the second and third fingers, and sometimes on the radial surface of the fourth finger, it is necessary to think about damage to the C7 root .
In the lower extremities, acute loss of pain and tactile sensation due to damage to the L1 root appears as a longitudinal zone at the level of the groin, which distally reaches the innervation areas of the L2 and L3 , involving the anterior surface of the thigh, and proximally extending over the buttocks. Sensory deficits along the medial and lateral aspect of the tibia indicate involvement of the L4 and L5 . and S2 nerve roots in the pathological process is manifested by a decrease in sensitivity along the back of the thigh and lower leg.
Peripheral nerves
Axillary nerve. localized sensory deficits may be encountered , raising the suspicion of peripheral nerve damage.
The following injuries can lead to damage to the axillary nerve:
- shoulder dislocation;
- damage to the humerus;
- prolonged pressure, stretching, or traction on the arm during anesthesia or sleep.
Localized deficits in pain and tactile sensation over the lower part of the deltoid muscle allow the doctor to easily recognize such a lesion.
Median nerve. Reduction or loss of sensation on the palmar surface of the first three fingers and half of the fourth finger, as well as on the dorsum of the terminal phalanges of the second and third fingers and half of the fourth finger indicates damage to the median nerve.
Acute loss of sensation in the zone of innervation of the median nerve is caused mainly by the following injuries:
- hand lesions;
- lesions of the forearm;
- lesions of the wrist and hand, including puncture and bullet wounds.
Interventions requiring the insertion of needles , especially into the cubital fossa , can also result in median nerve damage that manifests as sensory deficits and pain, often with a burning, causalgic component.
Prolonged compression during anesthesia or sleep can also cause acute injury to the median nerve, manifesting as sensory and motor deficits.
Numbness and tingling along the median nerve, which awakens the patient during sleep and resolves with shaking of the arm and hand, are classic symptoms of carpal tunnel syndrome , usually resulting from repetitive circular movements of the wrist. Patients with diabetes, hypothyroidism, arthritis or acromegaly, and pregnant women are especially prone to developing carpal tunnel syndrome.
Ulnar nerve. Acute sensitivity disorder, indicating damage to the ulnar nerve, is manifested by paresthesia, followed by a decrease in tactile and pain sensitivity on the fifth and ulnar surface of the fourth finger, as well as the ulnar part of the hand to the wrist.
The most common causes leading to damage to the ulnar nerve are:
- fractures and dislocations in the shoulder joint affecting the elbow;
- lacerations;
- pressure on the nerve during anesthesia or while intoxicated.
Radial nerve. In patients with acute radial nerve lesions, sensory deficits may be found on the back of the arm if the nerve is damaged in the axilla. Damage to the radial nerve proximal to the spiral groove of the humerus results in decreased sensation on the distal extensor surface of the forearm. The superficial branch of the radial nerve gives rise to the dorsal digital nerve in the distal forearm, innervating the skin of the dorsal and radial surfaces of the hand and the dorsum of the first four fingers. The radial nerve appears to be the most commonly injured peripheral nerve.
The most common causes of radial nerve injury include:
- shoulder dislocations and fractures;
- prolonged pressure on the nerve (especially in the nerve groove);
- radial neck fractures.
Femoral nerve. Acute damage to the femoral nerve is manifested by a decrease in sensitivity on the anterior and medial surface of the thigh and in the zone of innervation of the hidden nerve (n. saphenus) on the medial surface of the lower leg.
Acute femoral nerve injury can occur as a result of the following injuries:
- fractures of the pelvic and femur bones;
- hip dislocation;
- pressure or traction during hysterectomy;
- delivery using forceps;
- hematoma pressure in the area of the iliopsoas muscle or in the groin.
Paresthesia and loss of sensation in the area of innervation of the hidden nerve can occur as a result of its damage on the medial surface of the knee during medial arthrotomy or during surgical interventions ( coronary artery bypass grafting ).
Obturator nerve. Sensory loss due to obturator nerve injury is detected in a small area of skin on the medial thigh.
The nerve can be damaged in the following situations:
- during surgical interventions on the hip and pelvic organs;
- in cases of obturator hernia;
- secondary to hematoma of the iliopsoas muscle.
Lateral femoral cutaneous nerve. The sudden onset of tingling, numbness or discomfort on the lateral and anterolateral thigh is typical of the lateral femoral cutaneous nerve (meralgia paresthetica). Hyperesthesia is replaced by hypoesthesia. The discomfort or pain may be bilateral.
This nerve can be damaged in the following cases:
- due to compression by the inguinal ligament;
- with hemorrhage in the iliopsoas muscle;
- when obese patients wear too tight clothes.
Sciatic nerve. Acute sensitivity disorders, involving the outer surface of the leg, as well as the dorsal, plantar and inner surfaces of the foot, appear with acute lesions of the sciatic nerve. The distribution of sensory deficits reflects the areas of cutaneous sensation provided by the two branches of the sciatic nerve: the peroneal and tibial nerves .
Acute sciatic nerve injury can occur when:
- fractures or dislocations of the hip;
- operations on the hip joint;
- other pathological conditions of the pelvic organs, including gunshot wounds or injections into areas close to the sciatic nerve.
Peroneal nerve. When the common peroneal nerve is damaged at the level of the head of the fibula, sensitivity is impaired on the lateral surface of the leg and the dorsum of the foot. Sometimes only the superficial branch of the peroneal nerve is damaged, which is manifested by a decrease in pain and tactile sensitivity in the more distal parts of the lateral surface of the leg. When the deep branches of the peroneal nerve are affected, a small area of skin between the first and second toes may be identified with decreased sensitivity to pain and touch.
Most peroneal nerve injuries are traumatic in nature and are usually caused by:
- pressure applied to the upper and outer surfaces of the leg;
- stretching in the hip and knee joints;
- surgical operations in the knee joint.
Tibial nerve. Acute injury to the tibial nerve leads to sensory disturbances on the lateral surface of the posterior part of the leg, innervated by its branch, the medial sural cutaneous nerve. Additional branches of the tibial nerve supply the skin of the lateral heel, the lateral aspect of the foot (sural nerve), and the sole, with the medial two-thirds of the plantar being innervated by the median plantar nerve and the lateral third by the lateral plantar nerve.
The tibial nerve is most often damaged in the popliteal fossa, at the level of the ankle joint or foot.
Damage to the tarsal tunnel, where the nerve crosses the medial malleolus, causes loss of sensation in the toes and dorsum of the foot.
Plexopathy.
Acute sensorimotor deficits indicating multiple nerve damage in a separate upper or lower extremity raise the suspicion of plexopathy .
Brachial plexus plexopathy. The acute appearance of a feeling of tingling, numbness and pain, followed after a few hours or days, as a rule, by muscle weakness and patch-type hypoesthesia in the area of the shoulder girdle and proximal muscles of the shoulder, is typical for damage to the brachial plexus (amyotrophic neuralgia). Acute brachial plexopathy may be caused by trauma in which the arm is excessively abducted, or may occur secondary to tractional movements of the arms, including injuries during childbirth. Damage to the brachial plexus can occur in epidemic form.
Brachial plexus plexopathy can develop after:
- infections;
- vaccinations;
- parenteral administration of serums;
- may occur as a complication of coronary artery bypass grafting.
In some patients, no apparent cause for plexopathy can be identified.
Plexopathy of the lumbosacral plexus is recognized by sensorimotor deficits and pain in the lower extremities. In acute lumbar plexus plexopathy , a common cause, in addition to trauma, is retroperitoneal hemorrhage.
Symptoms of the disease
In most cases, changes in the body manifest themselves gradually. Initially, numbness may occur in areas of the skin on the side of the thigh, then spread to the front. A sensitivity disorder occurs - sensations of burning, coolness, tingling, etc. occur. At the initial stage of the disease, these manifestations are temporary, but with the development of pathology they become permanent. There is pain and difficulty walking. In certain cases, hair loss and thinning of the skin may occur.
Treatment of pudendal nerve neuropathies
Therapeutic and diagnostic blockades
Conservative treatment is aimed primarily at removing tension (decompression) of the nerve in “critical zones” and restoring normal trophism.
The first stage is recommended to carry out therapeutic and diagnostic blockades of these very problem areas, which we talked about at the very beginning (areas of ligaments and muscles).
The most common are blockades with local anesthetic (lidocaine, bupivacaine) and glucocorticoid (betamethasone).
Transvertebral magnetic neuromodulation
Within the walls of our center, a unique method of treating neuropathic pain has been developed and adapted. It is highly effective for true pudendal nerve neuropathy and is used in parallel with blockades. The deep impact of a directed magnetic pulse with a certain frequency on the area where the pudendal nerve exits the spine (level S2-S3) allows you to “reset” the innervation and break the vicious circle of pain. The course of treatment with magnetic neuromodulation ranges from 10 to 15 sessions, depending on the severity of the disease.
Botulinum therapy.
Indicated in the presence of muscular-tonic syndrome, when the muscle needs to be relaxed. Botulinum toxin type A is successfully used specifically to target this pathological component.
When used correctly (according to indications and with good navigation via ultrasound), the risks of complications are minimal.
Transcranial magnetic neuromodulation
The newest method of influencing brain structures.
In Russia, we are leaders in the use of neuromodulation of the central and peripheral nervous system for the treatment of pelvic floor dysfunction and chronic pelvic pain syndrome. This technique is aimed at eliminating central sensitization - a condition that develops during a long course of the disease, when the patient did not receive adequate treatment in time.
Remember, even with a prolonged course of the disease there is a way out!
Manual therapy.
The main goal of treatment by an osteopathic neurologist is to eliminate biomechanical disorders and pathological changes in soft tissue structures.
When a person has a sore muscle, he tries to reflexively “save” it by changing his position, sitting or walking. This leads to the fact that these structures, which bear an additional “volume of work,” begin to experience additional stress and get sick. And this only strengthens the vicious circle of disease development. With the help of manual techniques, it is possible to return to its place what has been displaced and is involved in the pathological process.
Pudendal nerve neuropathy: a patient’s history of recovery
Diagnosis and treatment of the disease
The diagnosis is made after all studies and collection of anamnesis of the disease. Consultation with additional specialists such as an orthopedist may be required. X-rays of the spine, ultrasound, CT, electromyography, and electroneurography are performed.
Treatment of neuropathy of the external cutaneous nerve of the thigh is carried out only in a combination of medication and physiotherapeutic, as well as reflexology methods. It is very important to eliminate the root cause of the disease.
Drugs are prescribed to reduce pain, anti-inflammatory drugs, analgesics, and sometimes it is necessary to resort to the administration of anesthetics. Vasoactive agents and metabolic pharmaceuticals are used. Physiotherapy and reflexology are provided. Sometimes it is necessary to resort to surgery, which involves decompressing the nerve.