Etiology and pathogenesis
There are several theories of the etiology of NLN: vascular, inflammatory, infectious, etc. However, in most cases (up to 75%), the causes of the development of NLN remain completely unclear (idiopathic neuropathy, or Bell's palsy).
The pathogenesis of idiopathic neuropathy is explained by the fact that cooling causes vascular disorders in the nerve trunk (spasm, ischemia, edema) that impair its function. A developmental anomaly is also important – congenital narrowness of the facial nerve canal [2].
Secondary NLNs are observed in various infectious diseases (syphilis, tuberculosis, Lyme disease, HIV infection, polio, encephalitis), tumors of the lower surface of the brain and the cerebellopontine angle, meningeal carcinomatosis, cerebrovascular accidents in the brain stem, fractures of the base of the skull and the pyramid of the temporal bone , inflammatory diseases of the parotid gland, acute and more often chronic otitis, during hypertensive cerebral crises, with sarcoidosis, collagenosis, amyloidosis, Guillain-Barré syndrome, multiple sclerosis [3].
There are cases of congenital paralysis of the facial muscles innervated by the facial nerve (Moebius syndrome), and hereditary and family cases are also described, apparently associated with a genetically determined anomaly of the facial nerve canal [3].
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Topical diagnosis
Topical diagnosis of NLN is based on its different structure at different levels, therefore, a change in the nerve proximal to the origin of a certain branch causes a loss of the corresponding function, and with a distal change, the function is preserved. This is the basis for the diagnosis of neuropathy along the canal of the facial nerve, where three branches depart from the nerve: the greater petrosal nerve, which supplies fibers to the lacrimal gland, the stapedius nerve, which innervates the stapedius muscle, and the chorda tympani, which provides taste innervation to the anterior 2/3 of the tongue. Determining the degree of neuropathy is based on identifying complete or partial loss of functions of the facial nerve and the dynamics of the development of symptoms.
Disturbances in the motor function of the nerve can be determined visually by facial asymmetry. With significant damage to the nerve, a picture of peripheral paralysis develops: the face is mask-like, the corner of the mouth is lowered, the palpebral fissure is open, the eyebrow is lowered, motionless.
To determine the autonomic function of the facial nerve, the functions of tear and salivation are examined. Tear production is examined using the Schirmer test (ribbons of filter or litmus paper are inserted into the lower fornix of the conjunctiva of the eye of the subject, resulting in lacrimation; the intensity of tear production is determined by the length of the wet paper in millimeters). Salivation is examined by radiometric determination of the concentration ability of the salivary glands and determination of the intensity of salivation by the amount of saliva received (while the patient under study is sucking a slice of lemon, saliva is collected separately for a minute from the pre-catheterized right and left parotid ducts). The study of taste sensitivity in the anterior 2/3 of the tongue is carried out using the method of chemical density testing, in which the thresholds of the main taste sensations (sweet, salty, sour and bitter) are determined by applying appropriate solutions to the tongue.
Symptoms
Symptoms of facial neuropathy make it possible to immediately suspect the disease. Signs arise from the affected nerve. Patients note:
- acute pain: it usually begins in the ear area and gradually spreads throughout the face and begins to radiate to the occipital region;
- intense lacrimation, less often dry mucous membranes of the eyes;
- discomfort or ringing in the ear due to sharp sounds;
- disturbance of the sense of taste in the anterior parts of the tongue.
As the disease progresses, signs of damage to the motor fibers of the nerve appear:
- smoothness of skin folds, especially nasolabial folds;
- swelling of the cheek when exhaling or trying to pronounce a consonant sound;
- lack of complete closure of the eyelids, rotation of the eyeball upward and outward (lagophthalmos);
- leakage of fluid from the corner of the mouth;
- food getting stuck between the gum and cheek when eating;
- limitation of facial expressions: the patient cannot frown or smile.
If the cause of neuropathy is an infectious process, the characteristic signs are accompanied by symptoms of general intoxication:
- high body temperature;
- headache;
- nausea and vomiting;
- weakness.
Clinic
The development of the disease is often preceded by general or local hypothermia, especially of the head. Symptoms of a general illness (fever, general weakness) are not typical for idiopathic NLN; if they occur, it is important to exclude secondary LLN (especially those developing against the background of infections). The clinical picture of the disease is represented by acutely developed weakness of the facial muscles, the maximum of which is achieved within several hours or one day. Slowly increasing paresis of facial muscles (FMP; over weeks or months) is not typical for idiopathic NLN; most of such cases are subject to differential diagnosis with a space-occupying process.
The main symptoms of NLN are caused by PMM of the upper and lower half of the face (prosopoplegia). Already at rest, the mask-like appearance of the corresponding half of the face (the face of the sphinx) attracts attention - the eye is wide open, almost does not blink; forehead without wrinkles; the nasolabial fold is smoothed; the eyebrow and corner of the mouth are lowered. The patient cannot frown, raise his eyebrows, when closing his eyes the eyelids do not close completely, the palpebral fissure gapes (lagophthalmos), when trying to close the eye, the eyeball rises upward and deviates outward (Bell's phenomenon), while the sclera is not completely covered. When smiling or laughing, half of the face is motionless; when grinning, the mouth deviates to the healthy side; when puffing out the cheeks, the diseased side “sails.” While eating, food gets stuck between the cheek and teeth, saliva and liquid food are poorly retained in the mouth, the patient cannot spit or whistle. During the acute period, the patient clearly pronounces labial sounds (b, m). Due to the slight displacement of the mouth, the protruding tongue may deviate slightly in the healthy direction.
Often, motor disturbances appear simultaneously with movement disorders, and sometimes they are preceded by usually mild and short-lived pain in the area of the mastoid process and the auricle. Other disorders may also be observed due to changes in the sweat, salivary and taste fibers of the nerve trunk, extending into the facial nerve canal at its different levels. When the facial nerve changes in the canal above the origin of the greater petrosal nerve, in addition to paralysis of the facial muscles, there is a lack of lacrimation (dry eye), sweating (dry skin of half the face), unilateral loss of taste in the anterior 2/3 of the tongue, strong, unpleasant perception of ordinary sounds (hyperacusis) . With damage below the origin of the petrosal nerve, increased lacrimation is observed, because due to the weakness of the lower eyelid, tears do not enter the lacrimal canal, but flow out, as well as taste disorders and hyperacusis. With a change below the stapedius nerve, hyperacusis does not occur; with a lesion below the origin of the chorda tympani, there are no disorders noted above, but lacrimation persists.
Lacrimation caused by weakness of the orbicularis oculi muscle is observed in 2/3 of patients with NLN; dry eye occurs much less frequently due to the involvement of lacrimal fibers. About a third of patients note a distorted, unpleasantly enhanced perception of sounds (hyperacusis) on the affected side, associated with paresis of m. stapedius Taste disturbance on the anterior 2/3 of the tongue on the affected side occurs in approximately half of the patients.
When the function of the facial nerve is impaired at the level of the geniculate ganglion, Ramsay Hunt syndrome is observed - a combination of peripheral paralysis of the facial muscles with herpetic rashes and excruciating pain in the area of the auricle, tympanic cavity, the back of the palate and the anterior half of the tongue [4].
NLN can sometimes be bilateral (diplegia facialis). Acute bilateral paralysis of facial muscles can develop with Guillain–Barré syndrome, tick-borne borreliosis (Lyme disease), tuberculous meningitis, sarcoidosis, and meningeal carcinomatosis [2, 3].
An important diagnostic and prognostic value is the study of electrical excitability of the nerve, which reveals a partial or complete reaction of degeneration, and complete is a prognostically unfavorable sign. An electromyographic study makes it possible to judge the speed of impulses along the facial nerve and its branches, as well as changes in the nucleus of the nerve.
Peripheral paralysis of the facial muscles should be distinguished from central paralysis associated with the involvement of the corticonuclear fibers of the bridge, in which the electrical excitability of the facial nerve is not qualitatively changed.
Purely clinical signs are also important in diagnosis. With NLN, the upper and lower groups of facial muscles are involved to the same extent. With central paralysis, the muscles of the lower half of the face suffer significantly more; paralysis of the muscles of the upper facial group is almost absent. The muscles of the upper parts of the face are innervated from that part of the facial nerve nucleus that receives bilateral corticonuclear pons fibers.
As a rule, the course and prognosis of idiopathic NLN are favorable. Mild cases are observed with complete restoration of facial movements within 2–3 weeks, moderate cases last about 2 months, sometimes recovery occurs only after 56 months. First, the function of the muscles of the upper half of the face is restored, then the lower half.
Most cases end with complete recovery with restoration of the functions of the facial muscles; in some cases, minimal residual symptoms remain, and in some patients, recovery is incomplete with the formation of contractures of the facial muscles and pathological synkinesis. Complete restoration of facial muscles is observed in approximately 70% of cases. The incidence of complications, in particular secondary contracture of facial muscles, is quite high and, according to various estimates, can range from 7.5 to 73.0% of cases [3]. The reason for the development of contractures of facial muscles after undergoing NLN is assumed to be the formation of the ephaptic region, where a kind of “artificial synapse” arises, transmitting impulses from one fiber to another. Postparalytic contracture is characterized by three main signs: persistent, painful tension of paretic facial muscles, the appearance of pathological synkinesis (conjugal movements), clonic-tonic spasms, tics, hyperkinesis in individual facial muscles [3].
Typically, signs of contracture appear within 3 to 6 months after the onset of NLN. Factors that provoke the occurrence of contracture of the facial muscles are long-term use of electrical procedures, early administration of anticholinesterase drugs (neostigmine methyl sulfate, galantamine), and excessively strong impact on the facial muscles during therapeutic exercises and massage [3]. With contracture, the palpebral fissure narrows on the affected side, the corner of the mouth is pulled up, and the nasolabial fold on the healthy side is smoothed out. During the study, it is established that the side on which differentiated movements are difficult has been changed. Pathological synkinesis is observed: eyelid-labial (when the eyes are closed, the forehead wrinkles and the corner of the mouth rises), eyelid-nasal (when the eyes are closed, the wing of the nose rises). When smiling, laughing, or showing teeth, an even greater narrowing of the palpebral fissure occurs at the same time, the eye may close, and when closing the eyes, the corner of the mouth tightens. More than 10 types of synkinesis have been described for contracture of facial muscles. Tics appear in the corners of the mouth, orbicularis oculi muscle, and cheeks. Mild synkinesis and isolated tic-like twitches may persist after complete restoration of the function of the facial muscles. Recurrences of LLN are possible both on the same and on the other side. They are rare and in some cases they are more severe, in others they are milder than the initial disease. With repeated episodes of PMM, a thorough examination of the patient is necessary to identify more severe diseases (carcinomatosis of the meninges, tuberculosis, sarcoidosis, etc.).
Complications
Regeneration of nerve cells and fibers is a very slow process, so therapeutic measures
are significantly delayed and labor-intensive. It is important that the specialist immediately selects the correct therapeutic tactics and draws up a personal program, and that the patient strictly follows medical recommendations.
Otherwise, significant deterioration and aggravation of the disease may occur, which are listed:
- weakening and reduction in the volume of muscle tissue, atrophy that develops 12 months after the onset of pathology is irreversible;
- tightening and loss of elasticity of facial wrinkles, contracture is accompanied by painful sensations and weakened pulsation, severe spasms and tugging of the affected facial area occur;
- involuntary muscle twitching, that is, the patient cannot control rhythmic contractions;
- conjunctivitis;
- facial synkinesis.
Differential diagnosis
Paralysis of facial muscles is not difficult to establish; it is more difficult to differentiate primary from secondary NLN. Combined neuropathy of the facial and other cranial nerves (impaired sensitivity in the face, weakness of masticatory muscles, noise in the ear, hearing loss, oculomotor and vestibular disorders), pyramidal and other conduction disorders indicate the secondary nature of the disease. In all cases of LPN, an otoneurological examination should be performed. Otitis is especially chronic and may be accompanied by NLN in the canal. Primary neuropathy may be indicated by the acute development of the disease, the connection of its occurrence with cooling - in some cases after a sore throat or flu. To identify early signs of contractures, a study of the state of electrical excitability of the facial nerve is performed.
It is important to differentiate idiopathic NLN from corticonuclear disorders and exclude secondary forms of facial neuropathy. Idiopathic LLN is usually unilateral. In most cases, the PMM is rough and equally expressed in all muscles. The absence of paresis of the orbicularis oculi and forehead muscles (or the obvious predominance of muscle weakness of the lower half of the face) suggests corticonuclear disorders, which are also accompanied by deviation of the tongue and, as a rule, more or less pronounced motor disturbances or increased reflexes and pyramidal signs in the ipsilateral limbs. The superciliary reflex does not disappear with central PMM. In addition, in the case of corticonuclear disorders, dissociation is possible between voluntary and emotionally regulated (smile, laugh, cry, etc.) contractions of the facial muscles. For example, with predominantly cortical disorders, the patient may have pronounced facial asymmetry with voluntary baring of teeth, while when laughing, the face is almost symmetrical (with deep subcortical lesions, the opposite situation is possible).
Partial PMM (eg, weakness of only the orbicularis oculi muscle or the buccal muscle) is uncommon in idiopathic LLN. Most of these cases are associated with tumors of the parotid gland (or other space-occupying processes in this area), causing compression of individual branches of the facial nerve.
Differential diagnosis for NLN should be made with Lyme disease and Melkersson–Rosenthal syndrome. Lyme disease is a common cause of LFN in endemic areas. Although NLN is one of the most common clinical manifestations of Lyme disease, it is rarely observed as the only manifestation of the disease; other symptoms (intoxication, skin rashes, joint changes) are more often present. Epidemiological history data are also important (stay in an endemic area, tick bite or the possibility of one). The diagnosis is confirmed using serological tests (enzyme immunoassay).
Melkersson–Rosenthal syndrome is a recurrent NPL (often with a change in the side of the lesion) in combination with a folded tongue, granulomatous cheilitis, swelling of the face and lips. The syndrome is caused by angiotrophic edema, which causes compression of the nerve in the canal. After each episode, there is a spontaneous, but usually incomplete restoration of the function of the facial muscles. Autosomal dominant inheritance is assumed.
Autotransplantation as an option for returning to normal life
The essence of this procedure is plastic surgery of the facial nerve. The material itself (graft) is taken from the patient’s leg. The latter is used as a binding material without rejection, to which the facial nerve of the healthy half of the face is sewn at two points.
Ultimately, the nerve impulse of the healthy half of the face is the only one for all facial muscles, providing real symmetrical movements. Subsequently, after a few years, the patient can undergo laser removal of scar tissue.
Facial nerve damage
There are injuries to the facial nerve due to fractures of the base of the skull, injuries to the parotid region, surgical interventions on the ear, salivary gland and total removal of acoustic neuromas. In case of fractures of the base of the skull, the nerve is damaged at the junction of the horizontal part of the facial nerve canal into the vertical one. The degree of nerve damage varies. When it ruptures, early paralysis of the facial muscles develops; when the nerve swells or the blood circulation in it is disrupted, late paralysis occurs, appearing 10–14 days after the injury.
During ear surgeries, nerve damage can be primary or secondary, when the nerve is compressed by bone fragments or hematoma; open when the integrity of the facial nerve canal is violated and closed. During operations on the parotid gland or injuries to this area, the extracranial part of the nerve distal to the stylomastoid process is damaged. During total removal of acoustic neuromas, the facial nerve is damaged along its path from the brain stem to the internal auditory canal.
Experts' forecast
In 80% of cases, the client completes the full course of treatment and makes a full recovery. Such a positive picture is only possible if there are no associated complications, which include:
- otitis;
- mumps;
- herpes.
Full rehabilitation can take up to several years, which significantly complicates the quality of life of some patients. Cases of complete recovery after 3 months are much less common. A similar scenario is possible only when damage to the facial nerve occurs at its exit from the skull.
Treatment
Conservative treatment
Treatment for NLN is usually carried out on an outpatient basis. Hospitalization may be indicated if the diagnosis is uncertain in order to conduct an in-depth examination in a hospital, as well as in cases where surgical treatment is planned.
The basis of treatment in the acute period is corticosteroids, which are prescribed in high doses in a short course, for example, prednisolone 1 mg/kg/day orally for 7 days, followed by a rapid dose reduction every 2–3 days. The benefits of high-dose intravenous corticosteroids (250–1000 mg/day) for 3–5 days have not been proven. Therapy should be started as early as possible (immediately after diagnosis) regardless of the severity of paresis; the best results were obtained when taking prednisolone in the first 24 hours from the development of NLN. The course of treatment is 2–3 weeks [1, 3].
Taking into account the possible etiological role of the herpes simplex virus in the development of idiopathic NLN, it is recommended to prescribe acyclovir (400–800 mg 5 times a day), valacyclovir (500–1000 mg 3 times a day) or famciclovir (500 mg 3 times a day) in combination with a corticosteroid ) within 7 days [4]. These antiviral drugs are undoubtedly indicated for Ramsay Hunt syndrome (or the appearance of signs of an active herpetic infection).
In the acute period, furosemide, pentoxifylline, acetylsalicylic acid, nicotinic acid, Eufillin, ipidacrine, and applications of a 33% dimethyl sulfoxide solution to the area of the stylomastoid foramen are also used. In case of severe or prolonged pain, non-steroidal anti-inflammatory drugs are prescribed. It is also possible to use ipidacrine at a dosage of 20–60 mg/day.
To prevent the development of keratitis in case of incomplete closure or dryness of the eye, it is recommended to instill moisturizing eye drops (with methylcellulose) throughout the day, wear safety glasses during the day, and apply an eye patch at night. These activities are carried out until the eye begins to close voluntarily and the blink reflex is restored.
Data on the effectiveness of physical therapy treatments are limited. There is evidence that exercises for facial muscles using electromyographic biofeedback lead to improved functional outcome and a decrease in the frequency of pathological synkinesis. The effectiveness of acupuncture, electrical stimulation and other methods has not been proven. However, these methods are widely used in everyday clinical practice.
Physiotherapy begins from the first days of the disease. Its task in the early period is to provide anti-inflammatory, decongestant, vasodilating, analgesic effects. For this purpose, light heat from a Minin or Sollux lamp is used on half the face, from the 5th–7th day - an UHF (ultra-high frequency) electric field in an oligothermic dosage or microwave therapy in the centimeter wave range on the area where the nerve exits or the mastoid process, massage of the cervical-collar zones, sometimes acupuncture. From the 10th to 12th day, in case of severe asymmetry of the face, adhesive bandages are used on the altered half of the face to normalize proprioceptive impulses. If there are foci of chronic infection in the area of the nasal pharynx (chronic tonsillitis, pharyngitis), their sanitation is carried out during this period - inhalation therapy, currents and fields of HF (high frequency), UHF, microwave (ultra high frequency), local UV (ultraviolet) irradiation. Subsequently, in the absence of signs of contracture, physiotherapy is carried out using intensive methods and mainly on the changed half of the face: ultrasound or hydrocortisone phonophoresis, Trilon B phonophoresis (EDTA Na4), electrophoresis of medicinal substances (neostigmine methyl sulfate), galvanization, electrical stimulation of the facial muscles, collar muscles, 4–5 weeks heat treatment (mud, paraffin, ozokerite applications), laser magnetic therapy.
In severe NLN, electrophoresis of anticholinesterase drugs and electrical nerve stimulation are used under the “cover” of carbamazepine at a dose of 100–200 mg 3 times a day to prevent the development of contracture of facial muscles.
In case of early electrodiagnostic signs of contracture, it is recommended to act on the segmental reflex zone (cervical-collar zone). For this purpose, phonophoresis of hydrocortisone, metamizole sodium (Analgin) or aminophylline (Eufillin) is used, depending on the cause and symptoms of the disease, sinusoidal modulated or diadynamic currents to the area of the upper cervical sympathetic node or to the cervical spine with small local electrodes (current strength in vascular origin diseases up to moderate vibration), massage of the cervical-collar area; from the 4th–5th week, heat treatment on the cervical-collar area (mud, paraffin or ozokerite applications), general mineral baths (chloride, radon, sulfide) and pulsed currents. Phonophoresis and pulsed currents can be alternated with heat therapy and general baths. It is not recommended to use contact electrical procedures (galvanization, electrophoresis of medicinal substances using the Bergonier half-mask technique, electrical stimulation), facial massage, intensive ultrasound (large area head, continuous mode, long courses), since they can increase contracture.
Therapeutic exercises for NLN begin 10–12 days from the onset of the disease. It helps improve trophic processes in paretic muscles and develop new motor conditioned reflex connections. Therapeutic gymnastics includes three main elements: positional treatment, passive and active movements. Positional treatment restores facial symmetry by bringing the attachment points of paretic muscles closer together using adhesive tape. It is carried out daily for 2–4 weeks for 1–2 hours 2 times a day. At the same time, it is necessary to begin passive gymnastics under visual control (in front of a mirror). The method of passive movements is as follows: the patient’s index finger is placed on the motor point of the muscle (points for electrodiagnostics), and at a slow pace the finger moves only in one direction. Passive movements for all modified facial muscles are carried out 2 times daily (5–10 movements for each muscle).
Active gymnastics begins when small voluntary movements appear. It is also carried out under visual control (in front of a mirror) and is carried out simultaneously for paretic and healthy muscles. First, individual muscles are trained, isolated movements are developed, then they move on to training more complex facial movements. If the volume of active movements is insufficient, the patient should help voluntary movements with his fingers in the same way as is done with passive gymnastics. Active gymnastics is carried out daily, 2 times a day.
After 10–12 days from the onset of the disease, massage begins in order to improve trophic processes and strengthen facial muscles on the affected side. It is carried out simultaneously symmetrically on both halves of the face, following massage lines and using stroking techniques, light kneading, and vibration. In cases of vascular origin, massage begins from the collar area.
With the development of contracture of the facial muscles, treatment with positioning with stretching of spastic muscles, special therapeutic exercises aimed at combating friendly movements and stretching of spastic muscles are indicated. Chewing is recommended only on the healthy side.
In case of secondary LLN, treatment of the underlying disease and restorative therapy of motor disorders is carried out according to indications.
Surgical treatment
If conservative therapy is unsuccessful, the question of surgical treatment is raised. Surgical intervention is performed depending on the location of the damage to the facial nerve: in the cranial cavity, in the pyramid of the temporal bone, or extracranially.
If during removal of acoustic neuromas the distal and proximal ends of the damaged facial nerve are preserved, an end-to-end intracranial suture of the nerve is used. When the facial nerve is damaged during basal skull fractures and during otiatric surgery, it is decompressed by removing the outer bony wall of the facial nerve canal, using an end-to-end suture of the nerve, and replacing the facial nerve defect with a nerve graft. When surgery or nerve injury occurs in the parotid area, an attempt may be made to find the ends of the cut nerve and suture it or perform plastic surgery. If surgical intervention is impossible for intracranial nerve damage, plastic surgery is used, the essence of which is to connect the peripheral end of the facial nerve (recipient) with the nearby motor nerve (donor).
The accessory, phrenic and hypoglossal nerves are used as donor nerves. Most authors prefer anastomosis of the facial nerve with the hypoglossal nerve or, if technically possible, with its descending branch. The operation consists of isolating the trunk of the facial nerve at the stylomastoid process and dissecting the nerve at the temporal bone itself. Sometimes it is advisable to widen the stylomastoid foramen by removing a small portion of the mastoid process (Taylor operation). The donor nerve is then isolated and dissected so that its central end can be connected to the peripheral end of the facial nerve. The suture of the nerves is performed using an operating microscope and microsurgical instruments. The same operations can be used for LLN that is resistant to conservative treatment. 3–4 months after the operation, the first movements of the facial muscles on the side of the injury appear that are friendly to the function of the donor nerve.
Rehabilitation treatment
Rehabilitation treatment for NLN includes a set of measures: drug treatment (vitamin B1, neostigmine methyl sulfate, ipidacrine in standard dosages), physiotherapeutic procedures (faradization, ultrasound), massage. To reduce the traction of the muscles of the healthy side and stretch the muscles of the affected side of the face, adhesive skin tension is used. Great importance is attached to therapeutic exercises and active facial exercises of the patient in front of the mirror.
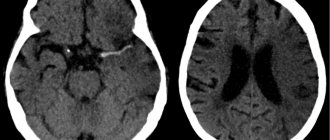
During the first month, it is advisable to carry out repeated examinations weekly (with corticosteroid therapy, examinations are required every week), then once every 3 months. The effectiveness and tolerability of treatment and the degree of restoration of facial movements are assessed. In the absence of positive dynamics within 3 months, an in-depth examination (including magnetic resonance imaging) is necessary to exclude other diseases, and it is also indicated if any new neurological symptoms appear. The duration of follow-up is usually 12–18 months.
In conclusion, it should be noted that in addition to drug and non-drug methods of treating NLN, it is extremely important to establish contact with the patient, who must be briefly informed about the essence of the disease, while focusing his attention on a favorable prognosis for life. When prescribing corticosteroids, the patient should be warned about the possible side effects of short-term therapy (mood changes, fluid retention, sleep disturbances). In case of severe paresis of the orbicularis oculi muscle, it is important to warn the patient about the need to protect the eye as much as possible from any damage and if any signs of keratitis (pain, redness) appear, immediately consult an ophthalmologist.
Diagnostics
Neurological disorders characteristic of facial neuropathy can also occur with other diseases, in particular with stroke. That is why, if any similar symptoms occur, you should urgently consult a neurologist.
Diagnosis of pathology includes:
- collection of complaints;
- taking an anamnesis, during which the doctor clarifies the time and circumstances of the onset of symptoms, records previous and chronic diseases, injuries and other important details;
- neurological examination, during which a specialist checks skin sensitivity, motor function, muscle strength, quality of reflexes, functioning of the central nervous system, etc.;
- tests: general blood and urine analysis, biochemical blood test with mandatory determination of glucose levels, determination of antigens and antibodies to infectious diseases if their presence is suspected;
- X-ray of the chest organs: allows you to diagnose tuberculosis, tumors;
- MRI or CT scan of the brain: helps visualize tumors, areas of acute ischemia, hemorrhages, consequences of injuries and strokes;
- CT scan of the temporal bone;
- electroneuromyography: assessment of the speed of impulse transmission along nerve fibers and muscles, allows you to determine the level of damage and severity of the disease;
- consultations with specialists: therapist, otorhinolaryngologist, endocrinologist, infectious disease specialist, if necessary.
The list of studies can be adjusted depending on the specific clinical situation.
Prevention
Compliance with the rules for the prevention of facial nerve neuropathy can reduce the likelihood of pathology occurring. This is especially true if there is an increased risk of developing the disease. Doctors recommend:
- avoid hypothermia and facial injuries;
- observe safety precautions at work to prevent eye damage;
- consult a doctor in time for infections and otitis media;
- control blood sugar levels;
- promptly diagnose and treat chronic diseases.