Our clinic is engaged in examination, treatment and rehabilitation measures for pinched, inflammation and injuries of the nerves of the legs (sciatic, tibial, peroneal and their branches). You will need to be examined by a neurologist. if any studies have been previously performed, be sure to take their results for consultation, incl. the x-rays themselves . If the studies have not been performed, we will do everything necessary in our clinic or with our colleagues in other clinics.
- What are the causes of damage to the tibial and peroneal nerves?
- Symptoms of Tibial and Peroneal Nerve Suffering
- Diagnosis of neuropathies of the tibial and peroneal nerves
- Treatment of damage to the tibial and peroneal nerves at the Echinacea clinic
- When is surgery necessary?
How the treatment will be structured:
- Let's establish the location and cause of nerve damage. We perform electromyography of the peroneal, tibial and other leg nerves and ultrasound of the nerves. The potential benefit of non-surgical treatment or strict indications for surgery (risk of complete nerve loss) can be determined using needle myography.
- We will find out and discuss with you the possibility of non-surgical treatment and the prospects for restoring nerve function. Medicines can be used here, incl. administration of anti-inflammatory and absorbable drugs directly to the point of compression or damage to the nerve. For the rehabilitation treatment of the sciatic, tibial and peroneal nerves, magnetic stimulation of the nerves of the legs is very effective: improvement is noticeable immediately or several days after the procedure.
- If the chances of restoring the peroneal or tibial nerve without surgery are low, we recommend surgical treatment . We perform most of the operations on an outpatient basis. You will be able to go home on the day of surgery. The budget for surgery without hospitalization is significantly less. If hospitalization is required, we will refer you to a trusted specialist. After surgical treatment, we will offer a course of rehabilitation treatment.
What is peroneal nerve tunnel neuropathy?
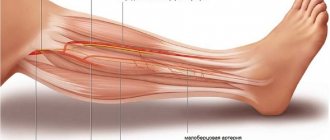
From the lumbar and sacral roots, a powerful trunk of the sciatic nerve is formed, the largest in length and diameter in the human body. Following down from the lumbar region in the popliteal fossa (sometimes in the thigh), the sciatic nerve divides into two large branches: the tibial nerve and the common peroneal nerve.
Next, the trunk of the peroneal nerve bends around the fibula below its head, passing between the bundles of the peroneal muscle, and is divided into terminal branches. We will not go into the intricacies of anatomy; clinically important is the place where the nerve passes near the head of the fibula in the musculofibular canal; here it is most vulnerable, since it is located superficially and next to the bone. Trauma to the nerve in this place leads to the formation of tunnel neuropathy.
Diagnostics
Tibial nerve neuropathy belongs to the group of mononeuropathy of the extremities. The clinical picture of the pathology is characteristic of dysfunctions of the musculoskeletal system and is of a traumatic nature, and therefore is subject to joint observation and control by specialists in the field of neurology and traumatology.
The first step in making a diagnosis is to question the patient about injuries to the lower extremities, working conditions, as well as the characteristics of the clinical picture and the presence of other diseases that may affect the normal functioning of the nervous system. After this, the patient is examined to identify atrophic and neurotrophic changes in the lower leg and foot.
Based on the data obtained, an initial diagnosis is made, which is confirmed by instrumental studies using one of the following methods:
- ultrasound diagnostics of the lower extremities;
- electromyography is a research method that allows you to determine the performance of the muscular system of the lower leg and foot;
- X-ray diagnostics if indicated, for example, for fractures;
- trigger point blockade is a therapeutic and prophylactic method that involves administering a medication to the affected areas of the lower extremities, which makes it possible to determine the degree of nerve damage;
- CT and MRI are used as additional diagnostic methods when using other methods there is insufficient data to make a diagnosis.
Causes of peroneal nerve neuropathy
The causes of neuropathy can be judged by the names that different authors have used to call peroneal nerve tunnel syndrome: sleep paralysis, fashion model syndrome, tulip digger's paralysis. Let us list them in detail.
- Direct injury (fracture of the head of the fibula, dislocation of the knee joint) or traumatic injury when the foot is twisted, accompanied by tension on the peroneal nerve and its damage.
- Compression paralysis is compression of the nerve in the head of the fibula caused by external factors.
- by this mechanism, the nerve can be compressed during sleep or in an unconscious state (sleep paralysis) if the outer surface of the lower leg comes into contact with the hard frame of the bed;
- when sitting cross-legged for a long time - a position in which podium stars often pose in front of the camera (mannequin syndrome);
- compression of the nerve with a plaster cast or splint in the upper third of the leg;
- activities that require prolonged periods of kneeling or squatting (tulip bulb digger paralysis);
- compression of the nerve when wearing high narrow shoes (leather boots);
- a sharp decrease in body weight with loss of the protective subcutaneous fat layer can lead to compression of the peroneal nerve even with slight external compression
- Anterior tibial syndrome or anterior tibial muscle compartment syndrome. In this condition, caused by a fracture of the leg bones, arterial thrombosis or muscle strain due to prolonged walking, severe swelling of the soft tissues of the leg occurs and almost inevitable compression of the peroneal nerve
- Nerve damage during surgery (surgery for a popliteal artery aneurysm or a woman staying in a gynecological chair for a long time during surgery)
- Space-occupying formations in the knee area (Baker's cyst, knee ganglion)
- Genetic predisposition (familial cases of peroneal tunnel neuropathy have been described in the medical literature)
- Concomitant somatic diseases predisposing to the development of tunnel neuropathies (diabetes mellitus, polyarteritis nodosa)
Separately, it is necessary to highlight damage to the fibers of the peroneal nerve as part of the spinal roots or the sciatic nerve, when the traumatic factor acts at a higher level, and the clinical manifestations correspond to damage to the nerve in the upper third of the leg. Such manifestations may occur when:
- herniated intervertebral disc L4-L5 with compression of the fifth lumbar root, which is called vertebrogenic pseudoneuropathy of the peroneal nerve
- compression of the fifth lumbar root during childbirth due to compression by the fetal head
- non-compliance with the rules for intramuscular injections in the gluteal region and injury to the sciatic nerve
- traumatization of the fibers of the peroneal nerve, which are part of the sciatic nerve, when reducing a dislocated hip joint or performing total hip replacement
Any damage to the neural structures that form the peroneal nerve leads to an increased risk of injury at the level of the lower leg, even with minor external influences.
Symptoms
Neuropathy is accompanied by a clinical picture of severity, which depends on the degree of damage to the nerve fibers.
Nerve dysfunction can be recognized by impaired flexion of the foot and motor ability of the fingers. When walking, the foot is placed incorrectly - the emphasis is on the heel. The muscular system of the lower leg and foot shows signs of obvious atrophy and deformation.
In the case of traumatic origin of neuropathy, swelling forms in the ankle area, blood flow is disrupted, tissue sensitivity increases, and there is severe pain, which intensifies when the damaged areas are touched.
If the cause of nerve neuropathy is endocrine disorders or infectious lesions, the patient loses sensation in the lower extremity area of the leg and foot. The pain syndrome persists and can have a different nature and severity. The pain intensifies with walking and physical activity. The patient may experience involuntary contractions of individual muscles or a convulsive syndrome involving the lower limbs.
In addition, the patient is concerned about neurotrophic disorders, such as dryness of the epidermis in the lower legs and feet, keratinization of the upper layer of the dermis, brittle nails, pallor of the skin and a decrease in local temperature, increased sweating.
How to diagnose the disease?
Tunnel neuropathy of the peroneal nerve can be suspected based on typical complaints (weakness of the lower leg muscles, numbness of the outer surface of the lower leg and dorsum of the foot, burning shooting pain in the leg below the knee level). The diagnosis can be confirmed using stimulation electroneuromyography (ENMG).
This study allows using an electric current to “ring” the sciatic, tibial and peroneal nerves along their entire length and identify the local area of damage. In the place where the nerve is subjected to mechanical compression, its myelin sheath is damaged, which leads to a decrease in the speed of propagation of the nerve impulse along this segment of the nerve trunk.
It is this parameter during ENMG that is the most informative for establishing the diagnosis of tunnel neuropathy.
When is surgery necessary?
In case of nerve injury, it is very important to decide in a timely manner whether conservative or surgical treatment is advisable. The answer to this question can be obtained after conducting needle myography, which will answer the question of what is the degree of damage to the nerve and whether it has a tendency to recover. If during this study it turns out that at least partially the nerve is preserved, we carry out active conservative treatment, after which we must repeat the study to make sure that the treatment had an effect . If, during needle myography, it turns out that the nerve is completely damaged and its restoration is impossible, we resort to the help of a neurosurgeon who suturing the nerve or releasing it from significantly narrowed canals. Then we perform the entire range of restoration procedures.
Various Treatment Methods
Pharmacotherapy
To restore the myelin sheath of the nerve, alpha-lipoic acid preparations (thioctacid, berlition, espalipon) are prescribed. Among other neurometabolic drugs, a combination of B vitamins (milgamma, combilipen, neuromultivit) is traditionally used or a combination drug is prescribed - Keltican, registered in Russia as a dietary supplement.
The use of non-steroidal anti-inflammatory drugs for peroneal nerve neuropathy is ineffective, since the cause of persistent pain is not so much inflammation of the soft tissues as damage to the nerve itself. This pain is neuropathic and requires the prescription of drugs from other groups: anticonvulsants (gabapentin, Lyrica, Finlepsin); antidepressants (amitriptyline, Cymbalta, Ixel).
Peroneal nerve block
If pharmacotherapy is insufficiently effective, a nerve block in the area of the head of the fibula can be used. A local anesthetic (lidocaine solution) is administered in combination with a hormonal drug (diprospan, dexamethasone). The clinical effect occurs after a single procedure. If necessary, a series of blockades can be performed while pain persists.
Surgical intervention
Surgical intervention is performed:
- in the presence of a formation in the soft tissues of the knee area, causing compression of the peroneal nerve (Baker's cyst, ganglion of the knee joint)
- in case of injury that leads to damage to the nerve trunk
- with anterior muscle compartment syndrome of the lower leg
Orthopedic correction
To prevent ankle sprains, a special orthosis is used to fix the foot. All factors that can lead to compression of the nerve in the upper third of the leg are excluded (narrow high shoes, prolonged squatting or cross-legged)
Symptoms of the disease
Pathology can manifest itself in different ways; if the pathology is acute, then the symptoms appear sharply, but if the disease is chronic, the clinic progresses. In general, the development of the disease may be indicated by:
- disorder of extension of the foot and fingers;
- man walking. The patient has to strongly bend his leg at the knee joint;
- lowering the foot onto the toes, and then onto the rest of the foot;
- inability or difficulty walking on your heels or raising the edge of the sole;
- pain on the outer part of the foot or lower leg;
- sensory disorders;
- amyotrophy.