Table 2 Psychophysiological characteristics and prognosis of conditions occurring with disorders of consciousness
| State | Self-centeredness | Sleep-wake cycle | Feeling pain and suffering | Forecast |
| Persistent vegetative state | Absent | Saved | No | Depends on the reason |
| Coma | Absent | Absent | No | Recovery of consciousness Persistent vegetative state Death within 2-4 weeks |
| Brain death | Absent | Absent | No | No recovery |
| Locked-in syndrome* | Saved | Saved | Yes | Recovery is unlikely, persistent tetraplegia, with good care, patients live a long time |
| Akinetic mutism** | Absent | Saved | Yes | Recovery is extremely unlikely (depending on the cause). |
| Dementia | Preserved, but lost in later stages | Saved | Yes. In later stages it is lost. | Progressive deterioration. Rate of progression depends on cause |
*Locked-in person syndrome is characterized by anarthria and tetraplegia, with preservation of the main manifestations of consciousness; this condition should be clearly distinguished from other types of disorders of consciousness.
**Akinetic mutism: refers to the condition originally described by Cairns (1941), complete wakefulness with absence or weakness of speech activity and voluntary movements. These patients show signs of conscious behavior, but the desire or attempts to speak or move are grossly disorganized. A large number of clinical and pathological variants of this condition have been described. Most often, akinetic mutism occurs with bilateral damage to the reticulocortical and limbic-cortical connections in the central part of the brain, extending from the paramedian areas of the reticular formation to the midbrain and diencephalon, basal and medial areas of the frontal lobes (Plum & Posner, 1980). N Engl J Med 1994; 330:1499. quoted from https://www.uptodate.com/contents/approach-to-the-adult-patient-with-syncope-in-the-emergency-department
Determining whether a patient belongs to any of the groups is important for prognosis, development of approaches to treatment, distribution of resources, and resolution of medico-legal issues.
Consequences of traumatic brain injury
Traumatic brain injuries can cause serious damage to a person’s nervous system, so even a minor concussion of mild severity should be taken seriously. The consequences of a traumatic brain injury can be unpredictable, so do not put off visiting a specialist. He will determine the degree and type of the disease and prescribe a treatment regimen. Among other medical institutions, the Research Institute named after. Burdenko, specializing in brain pathologies.
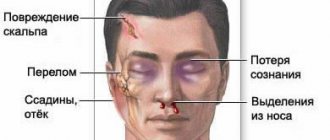
Types of traumatic brain injuries and main symptoms
All head injuries can be divided into several main types and types. First of all, they are divided according to biomechanics: shock-anti-shock injury with the passage of a shock wave through the entire brain, accelerated-decelerated when the cerebral hemispheres are displaced towards the trunk, combined, or simultaneous impact of the first types. Traumatic brain injuries are also divided according to the type of injury - focal, diffuse and combined, according to the genesis of the injury - primary and secondary lesions. Among the types of TBI, one can distinguish isolated injuries without damage inside the skull, combined, characterized by the presence of intracranial lesions as a result of mechanical impact, and combined.
By their nature, injuries can be closed, as a result of which the scalp is not damaged, open penetrating without damaging the dura mater of the brain, and open penetrating with damage to this membrane. The effects of severe traumatic brain injury can be unpredictable, and its symptoms differ from milder injuries. Most often, nausea, vomiting and dizziness appear in the first minutes after injury, while the consequences of a closed head injury are often less noticeable, and the consequences of an open head injury can be much more complex.
Clinical examination of the patient
Recommendations for assessing response in neurocognitive disorders
- Adequate stimulation is carried out only when it is certain that the patient's level of wakefulness is maximum.
- It is necessary to eliminate the causes that cause quantitative disorders of consciousness (taking sedatives, epileptic seizures).
- Attempts to elicit a response to verbal stimulation should not be aimed at eliciting movements, which are often performed reflexively.
- Research into the ability to carry out commands should include the types of motor activity available to the patient.
- Many different behavioral responses must be examined using a diverse range of stimuli.
- The study should be carried out in a calm environment.
- Initial estimates should be verified repeatedly using multiple re-assessments and acceptable response measurement approaches.
- Specific quantification techniques and tools may be useful.
A systematic approach to assessing patients with impaired consciousness includes the following steps:
Assessment of the functioning of the brain stem and other subcortical formations
- Pupillary reactions, blink reflex to visual stimuli.
- Eye movements, gaze deviations.
- Oculovestibular reflexes (oculocephalic reflex, calorimetric test).
- Corneal reflexes.
- Vomiting reflex.
- Breathing pattern.
- Decerebrate postures.
- Other postural reflexes, assessment of muscle tone.
Assessment of cortical functions
- Evaluation of voluntary actions
- Purposeful complex movements (including isolated motor control involving the cortex) compared with postural (decortication, decerebrate) or reflexive or stereotyped, monotonous (subcortical structures mediated) movements. Note: Pilon & Sullivan note different profiles of postural tone relationships for VS and SMS. Patients with VS exhibit classic decerebrate, decortication, and hypotonic postural features, whereas patients with SMS exhibit symmetrical or asymmetrical global flexor postures. However, there is no characteristic reflex posture with absolute diagnostic significance for separating these two groups.
- Involuntary vocal and verbal activity.
- Eye movements (signs of fixation of gaze or tracking of an object, differentiated from involuntary eye movements not related to the stimulus, or fixed gaze); responses to artificial or natural external stimuli.
- Tracking or fixating the gaze on various stimuli (use objects that do not make sounds: family photos, pictures of faces, money, mirror)
- Verbal stimulation (patient's name, commands, greeting): Begin with simple commands that encourage actions within the patient's ability.
- Eye commands: “look here”, “blink twice”.
- Commands for limbs: “show thumb”, “show 2 fingers”, “raise your hand”.
- Commands for the oral muscles: “open your mouth”, “show your tongue”
- Commands for the whole body or axial muscles: “turn your head”, “lean forward”.
- Ask the patient to stop the movement or hold the limb to highlight spontaneous repetitive movements.
- Painful stimulation.
- Assess the localization and purposefulness of defensive reactions, compare them with reflexive and generalized, stereotypical movements, evaluate facial expression
- Responses to random external stimuli.
- Assess attempts to grasp or perform actions with objects surrounding the patient (clothing, objects at hand).
- Observe changes in facial expression as you respond to stimuli such as a familiar voice, dialogue, pictures, music, etc.
- Notice attempts at purposeful movement in bed, in a chair, and while walking.
- Note gestures when communicating emotionally (yes/no signals).
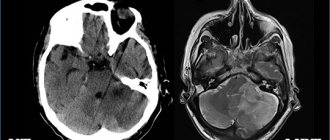
Diagnosis and consequences of traumatic brain injuries
To avoid the severe consequences of TBI, it is necessary to conduct a timely examination that will identify the type of injury and the degree of influence of external factors on the brain. The main feature of most traumatic brain injuries is the likelihood of secondary brain damage, and even with mild damage, you can rest assured only after a long period of time has passed, since the undesirable consequences of TBI and complications can appear a year later or much later.
Particularly undesirable consequences of traumatic brain injury are cystic-glial changes in the brain, as a consequence of TBI. In this case, the proliferation of glia occurs, and this is brain tissue. The consequences of a TBI can be different - from complete recovery to moderate and severe disability, when the patient becomes bedridden. Some patients fall into a vegetative state (no longer show signs of life), and local outcomes are not uncommon.
Consequences of a concussion
Consequences of a concussion
may appear after a few years, significantly complicating normal life. The hardest thing is for those who, for one reason or another, did not seek medical help in time for a timely diagnosis of the problems that arose.
Short-term disorders
In most cases, after a concussion, a person is bothered by certain symptoms, which most often disappear within a month after a head injury, subject to adequate treatment and compliance with the recommended regimen. Such consequences that occur in the near future after injury include:
- Intense headaches of a migraine or liquorodynamic nature. In most cases, cephalalgia persists during the first two weeks after injury, in case of severe injuries - a little longer.
Headache after a concussion in those who also suffer from hypertension is particularly intense
- Difficulty concentrating, absent-mindedness, memory impairment.
- Attacks of dizziness, often interfering with the patient’s normal movement.
- Nausea; sometimes – vomiting, which does not bring relief.
- Difficulty with reading and writing.
- Drowsiness, general weakness, fatigue.
All of these symptoms are characteristic of the recovery period and are associated with pathological changes resulting from the blow - swelling of brain tissue, destruction of neural connections and asthenia.
If unpleasant symptoms have not disappeared after 3 weeks, you should re-visit a neurologist to determine the cause of this disorder, since it is possible that long-term consequences of a concussion have developed that require special treatment.
Long-term consequences of TBILong-term consequences of TBI
The set of symptoms that occur several weeks, months or even years later and are associated with a concussion is usually called the long-term consequences of the injury. Common consequences are:
- Post-concussion syndrome.
- Vegetative-vascular dystonia.
- Epileptic seizures.
- Cognitive disorders.
- Personality changes.
Post-commotion syndromePost-commotion syndrome
Post-concussion syndrome (from the Latin “commotio” - concussion) is considered a common pathology after traumatic brain injury. Most often it occurs in the absence of diagnosis and adequate treatment of concussion.
The first unpleasant symptoms develop after several months, sometimes years, and it is always very difficult to get rid of them.
The main manifestations of post-concussion syndrome:
- Frequent, pronounced headaches of the migraine type, with various variants possible in the form of ophthalmoplegic or basilar migraine.
- Frequent attacks of dizziness.
- Sleep disorders including insomnia.
- Anxiety, excessive worry for no apparent reason.
- Decreased performance.
- Problems concentrating.
- High fatigue with usual loads.
Basilar migraine gets its name from the basilar artery, which supplies the brain stem, cerebellum, and occipital lobe of the brain.
Ostcommotion syndrome can significantly worsen the quality of life, and a complete cure is very difficult to achieve - simple symptomatic therapy is most often used.
Post-traumatic epilepsy Post-traumatic epilepsy
Sometimes a mild blow is enough to cause an epileptic focus in the brain, if a person has a genetic predisposition to the development of epilepsy. In this case, trauma acts as a provoking factor. The first seizures can occur several months or years after a concussion, causing difficulties in diagnosing and identifying the cause-and-effect relationship of the disease.
Personality and Behavioral ChangesPersonality and Behavioral Changes
Head trauma is often the cause of behavioral changes. A person may become irritable, aggressive, and touchy. A bad mood with depressive pessimistic thoughts predominates. The slightest irritating factors put a person into a state of passion and cause outbursts of anger. Such people just as easily enter a state of euphoria, often without reason.
A concussion aggravates all negative character traits, and it has been proven that with a blow to the frontal part, changes appear earlier.
Cognitive disordersCognitive disorders
Cognitive disorders include weakening of memory, high fatigue during mental activity, difficulties in perceiving and remembering new information.
Often after a head injury with a concussion, memory impairment is observed.
Often, after a concussion, a person loses part of his knowledge, his vocabulary becomes smaller.
VSD vegetative-vascular dystoniaVSD (vegetative-vascular dystonia)
Sometimes head trauma acts as a provoking factor in the occurrence of autonomic disorders. A person begins to feel attacks of headache, shortness of breath, tachycardia, and a feeling of suffocation. During an attack, sweating increases, the stomach hurts, nausea, dizziness are noted, and blood pressure often drops or, on the contrary, increases.
Other consequencesOther consequences
In addition to those listed, other unpleasant long-term consequences of a concussion are possible, but they develop much less frequently than others. It can be:
- Psychoses, neuroses, paranoid states.
- Inadequate perception by the body of alcoholic beverages, in which poisoning, intoxication and alcoholic delirium more often occur after previously habitual doses.
- Increased production of cerebrospinal fluid, which entails an increase in the level of intracranial pressure and the occurrence of corresponding unpleasant symptoms.
- Reduced cerebrospinal fluid production - in this case, on the contrary, cerebrospinal fluid is produced in insufficient quantities, which entails the development of chronic fatigue, dizziness, apathy and headaches.
To summarize, we can conclude that concussion should not be neglected. Even a mild degree of the disease requires compliance with a special regime, since it is possible that unpleasant symptoms will develop, which are very difficult to get rid of in the future. Timely diagnosis and proper treatment will help avoid consequences and allow the patient to get back on his feet faster.
« Back to previous page