Everyone in their circle of friends has a person who constantly complains about their health: they have a stabbing pain, they are sick, or they simply don’t feel well. But no matter how many times he goes to doctors, no one finds a specific reason for this condition. He’s pretending, we think. But don't rush to conclusions. These symptoms may be a sign of a somatoform nervous system disorder. It does not have an organic background, but leads to a mental imbalance of the individual.
Why does the disorder develop?
Somatoform disorder is a disease of a psychological nature in which the symptoms of damage to internal organs are functional, not organic.
Such dysfunction is detected in 0.5% of the world's population, and it affects mainly women. The reason lies, first of all, in the psychological state of a person.
The first group of factors influencing the occurrence of the syndrome is heredity and character traits. For example, people with asthenoneurotic and hysterical types of character are more likely to develop it. They are characterized by hypersensitivity, timid or demonstrative behavior. Such people are characterized by rapid nervous exhaustion; as a rule, they are pessimistic.
The second group is psychogenic traumatic external influences. These include acute stress factors, when a powerful psychological blow at once leads to a disorder of nervous activity. This could be the loss of a loved one, a decrease in social status, or a situation of severe fear.
Chronic stress occurs as a result of systematic mental and physical overstrain, lack of positive emotions, unmet needs and excessive demands on oneself.
It is worth noting that somatoform disorder very often develops in people who are emotionally stingy, hide their feelings, and do not know how to express them. And since emotions need a way out in any case, they find it in this unique way. A similar state can accompany members of religious families, where an atmosphere of strict morality reigns.
Other factors that provoke the disorder include complicated pregnancy, trauma, infections, and some somatic diseases.
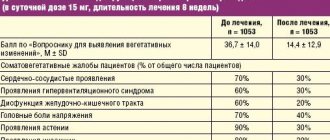
Treatment of somatoform disorder
Treatment of somatoform disorder is long-term and carried out comprehensively, combining drug treatment and psychotherapy. Psychotherapy helps the patient reconsider his beliefs and physical sensations, and learn to cope with stress and anxiety. Pharmacotherapy eliminates anxiety and corrects mood. Drugs are selected according to the clinical picture.
At the Alter Mental Health Center, the method of psychotherapy is selected taking into account the form and severity of the somatoform disorder. Often used in treatment are cognitive-behavioral and dynamic therapy, training in relaxation skills, and group classes to improve communication and social skills.
Lack of timely treatment can lead to loss of performance, problems in social relationships, and the risk of developing concomitant mental disorders increases.
If you notice signs of somatoform disorder in yourself or your family, we will provide you with qualified assistance, of high quality and at an affordable price. Our clinic is located in the center of Moscow, on Vsevolozhsky Lane, next to the Kropotkinskaya metro station. The specialists at the Alter Mental Health Center are interested in your speedy recovery.
Signs of illness
Symptoms of somatoform disorder are quite varied and manifest themselves in malfunctions of almost all body systems.
| System | Symptoms |
| Cardiovascular | Arrhythmias, sharp increases and decreases in blood pressure, pain and discomfort in the heart area. |
| Respiratory | Hyperventilation syndrome: shortness of breath, feeling of lack of air, dizziness. |
| Digestive | Irritable bowel syndrome: bloating, abdominal pain, diarrhea. Digestive disorders: poor appetite, nausea, vomiting, difficulty swallowing, feeling of a lump in the throat |
| urinary system | Frequent urination, pain when passing urine. |
| Genital area | Decreased libido, inability to achieve orgasm. Vaginismus in women; in men – weak erection, impaired ejaculation. |
| Other symptoms | Increased sweating of the palms and feet, chills, hyperthermia. |
As a rule, several symptoms associated with different systems occur simultaneously.
There are the following types of this disorder:
- hypochondriacal;
- somatized;
- somatoform dysfunction of the autonomic nervous system (SDVNS);
- chronic somatoform pain disorder;
- undifferentiated somatoform disorder.
Patients with somatoform dysfunction are distinguished by several features. This includes a peculiar, emotional or overly specific narrative about one’s condition. For example, a man comes to a cardiologist with pain and discomfort in his heart. But at the same time, he speaks not only about their character, but also about the fact that they cause him a lot of inconvenience. Such attacks occur at work, at the moment when he is supposed to make a report on his achievements. As a result, he cannot concentrate, paying all attention to his heart.
The reason here is this aspect: perhaps the man is psychologically not ready to talk about his work (for example, due to his failures), and the heart is assigned to the extreme. And it is precisely this that reacts to this stressor in order to divert attention from it.
Other distinguishing features are:
- exaggeration of pathological sensations;
- denial of the role of psychological factors in their development;
- increased irritability towards others.
Associated mental disorders
Somatoform dysfunction is accompanied by other mental disorders.
The disease is often accompanied by phobic disorders . Characterized by fear of death, agoraphobia, cancerophobia, fear of blushing.
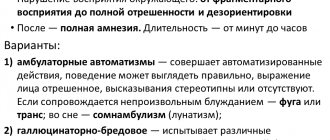
Panic attacks are an extremely common companion to the disorder. It is caused by a state of extreme fear and emotional stress. Characterized by an increase in the intensity of symptoms of the disease. It often provokes the development of depersonalization, fear of loss of consciousness, madness, and death.
Generalized anxiety disorder causes extreme tension, anxiety, and fears about the future. In addition to the characteristic manifestations of the disease, it contributes to the development of ideological and emotional phenomena. Worried about dizziness, weakness, feeling of lightheadedness. It is possible to develop derealization, when existing objects seem unreal, as well as depersonalization. The individual becomes hypersensitive, reacts sharply to extraneous stimuli, expecting danger.
Hypochondriacal dysfunction
Hypochondriacal disorder is characterized by a person's extreme concern about his or her health. He is sure that he is developing a severe, sometimes fatal disease. But their types may vary from case to case. One time the patient thinks that he has cancer, another time it is a severe heart pathology, etc.
The degree of sensation also changes. Either it seems to the individual that he is on the verge of death, then the manifestations become quite bearable.
It has been established that about 14% of patients visiting doctors of various specialties suffer from hypochondria. Most often it occurs in childhood and adolescence, as well as in mature people.
Basically, the patient is accompanied by the following symptoms:
- from the cardiovascular system - pain in the heart, disruptions in its functioning. The patient's conclusion is heart defects, heart attack;
- from the digestive system - abdominal pain, diarrhea, constipation. Conclusion – stomach and intestinal cancer;
- on the part of the excretory system – fear of uncontrolled urination, and therefore patients even limit leaving the house. Pain in the lower abdomen.
Important criteria for recognizing pathology are the presence of senestopathies and mood disorders.
Senestopathies are manifested by unusual and painful tactile sensations. This may be itching and burning, a feeling of cold, compression and constriction, pulsation of blood in the vessels, twisting, displacement and other similar phenomena.
Mood disorders manifest themselves in increased anxiety, sadness, melancholy, and a feeling of hopelessness. Patients focus only on themselves, and do not hear others at all. At the same time, they believe that no one needs them, everyone has abandoned them.
Such people systematically seek help from doctors. And if a specific disease is not found, they insist on re-examination.
The following nuances will help determine pathology:
- constant belief that a person has a serious illness, often with other concomitant illnesses. And even numerous normal examination results cannot convince them;
- lack of trust in doctors, despite their regular visits;
- the activity of such a patient is not aimed at alleviating the condition, but at confirming the presence of a progressive pathology;
- constant concentration on your illness;
- independent diagnosis.
As hypochondria worsens, it can develop into a paranoid state or hypochondriacal depression.
The diagnosis of hypochondriacal disorder is made when schizophrenia and schizotypal disorders, bipolar affective disorder are excluded.
Hypochondriacs are often found among famous people. Actor and director Woody Allen is one of them. One day, his illness saved him from food poisoning. The entire crew ate pizza, which only he refused due to concerns about his health. As a result, everyone except him developed an eating disorder.
Somatoform disorders
Characterized by “physical pathological symptoms that resemble a somatic disease, but there are no organic manifestations that could be attributed to a medically known disease” (Kaplan, Sadok, 1994). The DSM-III-R and DSM-IV list seven types of somatoform disorders:
- somatization disorder
- conversion,
- somatoform pain disorder,
- hypochondria,
- body dysmorphic disorder,
- undifferentiated somatoform disorder
- somatoform disorder, not elsewhere classified.
The term “somatization” was introduced into medical practice as an alternative to the concept of “conversion” (Dmitrieva, 1998); it is noted that in domestic psychiatry, somatoform disorders are considered within the framework of psychogenic diseases and the dynamics of constitutional-personal pathology, and their genesis is associated mainly with the influence of psychogenic and constitutional factors. It is emphasized that, conceptually, somatoform disorders are closely related to hypochondria, as well as anxiety, depression and hysteria. According to ICD-10, the main symptom of somatoform disorders is the repeated occurrence in the patient of physical symptoms that are not objectively related to physical disorders.
The patient, for his part, constantly demands more and more medical examinations in order to identify just such a connection, not wanting to accept the idea of the psychological conditionality of his illness. Somatoform in ICD-10 include: 1) somatization disorder, 2) undifferentiated somatoform disorder, 3) hypochondriacal disorder, 4) somatoform autonomic dysfunction of the heart and cardiovascular system, upper and lower gastrointestinal tract, respiratory and urogenital systems, another organ and system; 5) chronic somatoform pain disorder, 6) other somatoform disorders, and 7) unspecified somatoform disorder. The phenomena of conversion have been transferred to the group of dissociative disorders, but even there, due to the polysemy of the term, its use is not recommended. “Body dysmorphophobia” is also excluded; more precisely, non-delusional dysmorphophobia is included under the heading “hypochondriacal disorder”.
| | To accurately understand whether we are dealing with a somatomorphic disorder or a somatic disease, a complete comprehensive diagnosis is necessary |
A.B. Smulevich (1999) holds a different position. As a general term, he prefers the term “psychosomatic disorders,” including in the latter group the following disorders: 1) somatized mental reactions, or somatoform disorders, 2) “psychogenic reactions, or nosogenies,” and 3) “reactions of the type of symptomatic lability,” where “ we are talking about a psychogenically provoked manifestation or exacerbation of manifestations of a somatic disease.” The author includes conversion and somatization disorders, chronic somatoform pain disorder, somatopathies and somatotonia as somatoform disorders. A.B. Smulevich considers conversions to be those provoked by psychological stress in the sensitive and voluntary motor spheres, unstable algias and more complex “bodily fantasies” in the form of a “ball”, “nail”, “hoop” and “coma”. In his opinion, such disorders last no more than four months. He classifies as somatized, lasting up to six months, “polymorphic pathological bodily sensations” (however in the form of various algia), vegetative crises and dysfunction of internal organs.
By chronic somatoform pain disorder, the author understands persistent, painful, unchangeable in localization and intensity “idiopathic algias.” Somatopathy is “a variant of asthenic psychopathy,” and somatotonia “refers to pathocharacterological anomalies of the sthenic, expansive type.” Describing six types of personality reactions to illness, he evaluates them both in terms of nosognosia (hyper- and hyponosognosia) and by the nature of the disorder (neurotic, affective, pathocharacterological syndromes). Mentioning psychosomatic pathology, the author is no longer talking about reactions, not about provocation or exacerbation of a somatic illness under the influence of psychogenics, but about chronic somatic diseases, a “significant pathogenic role” in the development of which is played by traumatic events.
There are significant contradictions and ambiguities in the positions presented here. In empirical terms, the position of G.I. Kaplan and B.J. Sadok looks more preferable, and we will turn to it when describing the following disorders.
1. Disorder in the form of somatization. “Somatization disorder is a chronic syndrome consisting of many somatic symptoms that cannot be explained medically and that are associated with difficult feelings and the desire to get help from a doctor.” It manifests itself with a variety of somatic complaints, begins before the age of 30, and lasts for several years. Patients may believe that they are suffering from a physical illness.
The diagnosis is valid if 13 or more symptoms are detected from the 35 described below. The symptom is significant if a) there is no organic pathology, and the existing one is disproportionate to complaints, social and professional disorders, b) the disorder does not manifest itself only during panic attacks and c) the patient has to take medications, see a doctor, significantly change your lifestyle. Symptoms are combined into several groups. Gastrointestinal symptoms: vomiting (not like pregnancy), abdominal pain (not like menstruation), nausea (not like bowel disease), bloating (gas), diarrhea, intolerance (or poor well-being) of certain types of food. Pain symptoms: pain in the limbs, back, joints, during urination, other pain (except headache). Disorders of the heart and respiratory system: shallow breathing (without effort), palpitations, chest pain, dizziness.
Conversion or pseudoneurological symptoms: amnesia, difficulty swallowing, agony, deafness, double vision, blurred vision, blindness, fainting or loss of consciousness, seizures or convulsions, staggering when walking, paralysis or muscle weakness, urinary retention or difficulty urinating. Sexual symptoms (during a period of life with active sexuality): burning sensation in the genitals or rectum (not the same as during sexual intercourse), sexual indifference, pain during sexual intercourse, impotence. Female reproductive symptoms: painful periods, irregular menstrual periods, excessive menstrual bleeding, vomiting during pregnancy (if the patient considers these symptoms to be more frequent and severe than most women). The presence of somatization is indicated by the fact of seven obvious symptoms. This symptom complex, according to the authors, forms Briquet syndrome (1859). Some authors associate the latter with Munchausen syndrome (Campbell, 1981); others use it to designate a group of symptoms including a hoarse voice, increased breathing, and convulsive movements of the diaphragm (Peters, 1977). Note: for the domestic reader, the given definitions of symptoms may sound quite vague.
Somatization occurs much more often in women - 1–2%; in close relatives of patients it is detected in 10–20% of cases (in females); men in such families are prone to alcoholism, drug addiction and antisocial personality disorder. It is typical for patients to believe that they are ill for the majority of their lives. Anxiety, depression, and disturbances in interpersonal relationships are often detected; Suicides are rarely committed, usually in connection with drug addiction. Their descriptions of the disease are verbose, confusing, changeable, disorganized, and overly dramatized. They are seen as dependent and hysterical.
Only one doctor should treat such patients; this significantly limits the patient’s ability to manipulate the medical staff. Psychotherapy and, first of all, the patient’s satisfaction with medical care reduces his concern about his illness by half. Drug control, the prescription of antidepressants, tranquilizers, and mild neuroleptics may also be important. It is important to remember: patients treat drug therapy without due responsibility, and in addition, they often turn to charlatans for help, hoping for a miraculous cure.
2. Conversion disorder. The term “conversion” refers to the process by which a psychological complex of ideas, desires, feelings, etc. is replaced by a physical symptom, i.e., a somatic disorder (Rycroft, 1995). S. Freud believed (1893) that it is not the conceptual complex itself that turns into a physical phenomenon, but the affect attached to it, reflecting the fixation of libido on the Oedipus complex. Meanwhile, Rycroft points out, the transition from the mental to the physical is no less a mystery than the transition from the material to the fact of consciousness, the psyche.
One can have a different attitude towards the attempt to salvage the conversion hypothesis by suggesting that the somatic symptoms of hysteria are a symbolic manifestation of a certain meaning. There seems to be a psychological meaning to conversion if we consider that patients demonstrably present the corresponding symptoms without revealing a reaction of suffering to the disease; It seems that they really need such an illness; they are distinguished, like patients with a factitious disorder, by an abnormal need to be sick, and this need remains not fully conscious.
Symptoms of conversion are found in the sensory, motor and autonomic spheres, which is why they become similar to the manifestations of a somatic disease. They arise in a situation of psychosocial stress, presumably causing aggressive or sexual impulses that the individual cannot directly express if he is not able to recognize them. The anxiety that arises blocks or excites psychological structures in such a way as to express and, to some extent, realize a forbidden desire through body language without the participation of consciousness. In other words, conversion symptoms are not due to malingering, no matter how much they may appear to be; they cannot be eliminated by willpower. In addition, these symptoms are such that they express the patient's need for medical examination and treatment. They cannot arise except in the context of interpersonal relationships. The prevalence of conversion disorders has not been established. It is known that 0.01–0.02% of patients consult a psychiatrist annually for such disorders, and among them there are 2–5 times more women.
Sensory symptoms of conversion are represented by the phenomena of mental anesthesia in different types of sensitivity, and the distribution of disorders does not correspond to diseases of either the central or peripheral nervous system. Loss and weakening of skin sensitivity, taste, smell, paresthesia, deafness, blindness, “tunnel” vision on both one side and both are observed. Hemianesthesia, for example, begins exactly at the midline of the body. With blindness, patients can walk without any complications or self-injury, the pupils respond well to light, and cortical evoked potentials are normal.
Motor disorders are paresis, paralysis, astasia abasia, ataxia. When walking, irregular, jerking movements of the body and waving of the arms are observed; Patients rarely fall or hurt themselves. Rhythmic tremor, choreiform tics and twitching, aphonia, dysarthria, dyskinesia, and seizures with extremely expressive convulsions may occur. Sometimes the manifestations of a patient’s illness are similar to those of one of his relatives, acquaintances, patients in the ward or department, and he involuntarily identifies himself with them. If the patient has seen, for example, epileptic seizures, then his convulsions may be very similar to tonic-clonic seizures.
During hysterical attacks, patients do not completely disconnect from reality and, if doctors discuss the characteristics of the attack out loud, they can immediately, before their eyes, modify it, as if adjusting it to the required standard. An objective examination of patients with motor conversion disorders does not reveal any corresponding pathology: reflexes are preserved, there are no pathological reflexes, fasciculations and muscle atrophies are absent, the electromyogram is normal (with prolonged conversion paralysis there may be muscle atrophy and ankylosis). Conversion symptoms are often changeable, can disappear suddenly and reappear just as suddenly, be replaced by others, the disorder lasts up to 5–6 years or more. There is only one conversion symptom during one painful episode.
Under the influence of suggestion, hypnosis, and intravenous administration of barbamyl, conversion symptoms may disappear. As a rule, their appearance is accompanied by primary as well as secondary relief, since the internal conflict finds its expression and thereby weakens internal tension, and the disease, in turn, brings patients some advantages and privileges (support, help from others, sympathy, care from liability, etc.). The typical blind indifference of patients to the symptoms of conversion (and other hysterical disorders) is a “beautiful”, “beautiful” indifference, or La Belle indifferens. In ICD-10, conversion disorders are designated as dissociative and are mentioned along with dissociative amnesia, fugue, stupor, trance, states of mastery and obsession, Ganser syndrome, the phenomenon of multiple personality, and similar disorders in childhood and adolescence. G.I. Kaplan and B.J. Sadok, as shown earlier, some of the symptoms of conversion are considered in symptoms of somatization.
To diagnose a conversion disorder, it is necessary, among other things, to prove the connection between the appearance of its symptoms and the fact of psychosocial stress, as well as the nature of the disorder and the content of the traumatic experience. As for treatment, it is noted that long-term disorders do not respond well to it. In addition, patients often resist treatment for functional disorders (which is not the case for other disorders; organic, including cerebral, disorders are detected in 18–64% of patients). Treatment consists mainly of psychotherapy (suggestion in waking and hypnotic states, amytal-sodium intoxication; psychoanalysis, other methods). It is important to reduce resistance to treatment. You should not, for example, tell the patient that he only imagines himself to be sick, that it is beneficial for him to be sick, or that he is hiding in illness, etc. However, you should not follow his lead, thereby supporting the production of symptoms. It is necessary to find out the nature of the psychological conflict, show it to the patient, convince him to accept it and provide assistance in overcoming it. The most important thing is to create motivation for recovery, as well as to achieve a critical attitude of the patient towards the disease.
Illustration (Carson et al., 2004): “A 38-year-old woman, married, mother of five children, is admitted to the clinic. She complains of depression, meeting the criteria for major depressive disorder. Her marriage, concluded at the age of 17, turned out to be very unsuccessful: the husband is described as an alcoholic who has a permanent job; Quarrels often arise in the family due to financial problems, her indifference to sex and complaints of pain during sexual intercourse. From the anamnesis it follows that in the period from 19 to 29 years the patient herself abused alcohol, but since then has abstained from it. She says that she was nervous since childhood and was ill for a long time in her youth, and believes that she is sick with an unidentified somatic illness. Frequently visits doctors due to abdominal pain, which was diagnosed as a consequence of “colon spasm”. In addition to regular doctors, she consulted chiropractors and osteopaths for pain in her back, limbs and numbness in her fingertips. She was treated in a hospital due to complaints of chest and abdominal pain, as well as vomiting; During her hospitalization, she underwent a hysterectomy. After the operation, she suffered from anxiety attacks, fainting, vomiting, food intolerance, weakness and fatigue. During the examination, no somatic pathology was found. The patient explains her depression by hormonal imbalances, while continuing to seek a medical explanation for her other problems.”
3. Somatoform pain disorder. This refers to psychologically caused pain of various localizations. Patients have been in pain for at least six months. There is no real organic pathology associated with pain. The peak onset of the disease occurs between the ages of 40 and 50, as pain tolerance decreases with age. Women get sick twice as often as men. The disease is more common among workers.
In 60–100% of patients, dysthymia and depression are detected, often with daily fluctuations in well-being. In addition to pain, disorders such as anergy, anhedonia, decreased libido and weight, insomnia and irritability, and psychomotor retardation are expressed. Psychogenic pain is constant, usually insensitive to influences from the emotional sphere, cognitive sphere, attention, situations, as well as to the action of analgesics.
Pain during somatization is usually combined with many other somatic symptoms and abnormal skin sensations (itching, numbness, burning, etc.), begins before the age of 30 and is rarely observed in men. Conversion pain is usually short-lived, and pain that has a specific pathophysiological mechanism (for example, headache associated with muscle tension) is not considered a somatoform disorder. Nevertheless, pain caused by autonomic dysfunction (they, like other manifestations of vegetative dystonia, are considered in ICD-10 under section 45.3 - “Somatoform autonomic dysfunction”) are classified as somatoform pathology. Psychogenic pain that occurs during depression, schizophrenia, migraine, as well as organic pain with hysterical processing are not considered somatoform. Somatoform (psychogenic, idiopathic) pain is believed to be an unconscious defense that develops already in infancy or in young children: it is a way to achieve love, atone for guilt, avoid punishment, etc. The psychological interpretation of such pain, we note, is only a hypothesis.
It is indicated that somatoform pain usually begins acutely and in subsequent weeks and months increases in intensity. G. I. Kaplan and B. J. Sadok report that pain “may be post-traumatic, neuropathic, neurological, iatrogenic, or it may be pain in the striated muscles; Some patients may have other mental disorders, and some may not have them.” The prognosis of somatoform pain syndromes is unclear. “Psychogenic pain can sometimes resolve with treatment, after restriction of external reinforcers, or after successful treatment of co-occurring psychopathology. However, more often it lasts for years.” Patients can become litigious, seek financial compensation, and become dependent on psychoactive substances. The use of analgesics, sedatives and anxiolytics in the treatment of patients is ineffective; antidepressants (amitriptyline, melipramine, doxepin) are used more successfully. The successful use of multidisciplinary pain control programs has been reported, including psychotherapy (autotraining, cognitive psychotherapy, group psychotherapy, behavioral therapy, family therapy, etc.) as the main element.
4. Hypochondria. It manifests itself as constant presentation of somatic complaints or preoccupation with one’s somatic condition. There is no delirium of illness, but anxiety and depression are often expressed. The disorder usually appears before the age of 50 and occurs chronically or in waves. Patients are often observed by internists and are refused help from psychiatrists. Somatic disorders adequate to the complaints are not detected, patients do not believe doctors who are trying to convince them of the absence of somatic illness. G.I. Kaplan and B.J. Sadok argue that the nature of hypochondria is “psychodynamic,” since aggressive and hostile desires towards others “translate into physical complaints.”
The authors associate a predisposition to hypochondria with severe somatic illnesses (with subsequent hypochondriacal reactions) and somatic morbidity in childhood. Hypochondriacal reactions can also occur due to stress after the death or serious illness of someone significant to the patient. A tendency to hypochondria is observed in depression, generalized anxiety disorder, schizophrenia, other psychotic conditions, organic psychosyndrome, obsessions, and phobias. Hypochondriacs allegedly have a desire to “attract attention to themselves,” and they “loudly declare themselves abnormal.” “Primary” hypochondriasis reportedly responds better to group therapy because it “provides social support and social interaction.” Secondary hypochondriasis (depression, etc.) requires therapy appropriate to the underlying disorder. With hypochondriacal reactions, patients need to be helped to cope with stress without reinforcing their unhealthy behavior.
5. Body dysmorphic disorder. In ICD-10, non-delusional body dysmorphic disorder is presented as a variant of hypochondriacal disorder. Delusional hypochondria and delusional dysmorphophobia do not belong to either the somatoform or dissociative variants of the disorder. Note that the terms “somatoform”, “conversion”, “somatized”, “psychosomatic” are conventional names for a large number of disorders, the nature of which is unknown.
6. Somatoform autonomic dysfunction. This category of ICD-10 includes autonomic disorders with both objective signs (palpitations, sweating, redness and tremors) and “more idiosyncratic, subjective and nonspecific symptoms” such as “fleeting sensations of pain, burning, heaviness, tension, bloating or sprains,” related by patients “to a specific organ or system,” “which may also include autonomic symptoms.”
Data on a significant structural disorder of any organ or system are not identified, the disorder is chronic, causes anxiety to patients, they are so concerned about the possibility of a serious illness that they do not believe doctors who dissuade them from this. In addition, “additional subjective symptoms related to a specific organ or system” are observed. Symptoms of autonomic dysfunction are grouped depending on the organs and systems in which they predominate. The phenomena of vegetative dystonia occur in almost all diseases, including somatic and neurological ones. Local autonomic dysfunctions are more typical for segmental disorders of sympathetic innervation.
7. Other somatoform disorders. This refers to disorders in individual systems or parts of the body that are not directly related to autonomic dysfunction and local damage. Their appearance coincides in time with traumatic events. “Sensations of swelling, skin movement, and paresthesia (tingling and/or numbness) are common examples,” the ICD-10 reports. And here there is no clear distinction between somatic sensations and senestopathies, which in practice must be done very often. In addition, the following disorders are included: "hysterical coma" with dysphagia and "other forms of dysphagia", "psychogenic torticollis" and other disorders with spasmoid movements (excluding Tourette's syndrome), "psychogenic pruritus" (excluding alopecia, dermatitis, eczema or urticaria psychogenic type), “psychogenic dysmenorrhea” (excluding dyspaurenia and frigidity) and, finally, “teeth grinding”.
8. Somatoform disorder, unspecified and not elsewhere classified . Unspecified disorders include “unspecified psychophysiological” and “psychosomatic”. Not classified elsewhere include illness with symptoms of non-psychotic hypochondriasis lasting less than six months and illness with somatic and non-stress-related complaints lasting less than six months. For example, these are patients with an unreasonable fear of getting AIDS or patients who are afraid that they have AIDS. DSM-III-R also contains undifferentiated somatoform disorder, which includes complaints of general fatigue, anorexia, and one or more somatic complaints of disorders of the gastrointestinal or urinary systems. The duration of the disorder is at least six months. Organic pathology is not detected or it is insignificant and cannot be the cause of the existing social or professional decline. Cases of such a disorder are rare, and it “fully” meets the criteria for somatization.
The diagnosis of somatoform disorder can be established no earlier than after excluding somatic, endocrine, neurological pathologies, as well as endogenous, organic and other recognized mental diseases. It is also necessary to prove the connection of the alleged disorder with psychological conflict and traumatic events and situations for the patient. Only under these conditions can a somatoform (psychosomatic) disorder claim some independence and, even more so, the status of a separate painful form. There is no specific therapy for somatoform disorders, since data on the etiology and their pathogenesis are purely hypothetical.
Back to contents
Somatization and chronic somatoform pain disorder
Somatized dysfunction, in addition to organ manifestations, causes a decrease in the functioning of analyzers: vision, hearing, touch, smell. Coordination of movements is impaired: patients become clumsy and have an unsteady gait. Movement disorders manifest themselves in the form of paresis and paralysis.
They describe failures in the functioning of internal organs colorfully and with charm. For example, my head hurts, as if a hoop was put on it and was gradually being squeezed. Or your stomach is swollen like a balloon.
Unlike a hypochondriac, who expresses anxiety about his health, such a patient responds more rudely and persistently. He is convinced that he is sick. And if the doctor tries to hint at the psychogenic nature of the disorder, he screams and is indignant, rejecting what was said, and demands additional examination. This patient is constantly dissatisfied and complains.
The course of the disease is chronic, with wide variability of symptoms that persist for 2 years or more.
Often, a person, due to his anxiety and aggressiveness, experiences social maladjustment and family conflicts.
A pain disorder is distinguished by the presence of severe, debilitating pain that occurs for no reason. Usually it has a clear localization - the stomach, the heart. The pain characteristics do not change, there are no other symptoms.
During somatoform dysfunction, an undifferentiated disorder is also distinguished. With it, a person suffers all the typical symptoms of the disease, but it is not possible to classify them into any known group.
Diagnosis of somatoform disorder
The disease may remain undiagnosed for a long time due to the variety of symptoms, especially with somatization and undifferentiated somatoform disorders. The basis for the diagnosis of somatoform disorders is the collection of anamnesis and analysis of behavioral reactions. The presence of a disorder may be indicated by an improvement in condition after diagnostic examinations, ineffectiveness of treatment for a suspected somatic disease, uncertainty of complaints, or their dramatic change over time. The disorder may be accompanied by somatic illnesses, anxiety and depressive disorders.
It is important to pay attention to the presence of these clinical manifestations:
- Specific emotionally charged complaints about somatic malaise, autonomic dysfunctions, functional disorders (pain, cramps, muscle tremors, sleep disorders, appetite disorders, etc.) A person is fixated on any confirmation of his “diagnosis” and requires the appointment of examinations.
- The presence of manifestations of a mental disorder of the neurotic range (anxiety, fussiness, mood swings, irritability, short temper, apathy, fatigue, etc.)
- The presence of disorders of the somatosensory system. Sensopathy often manifests itself in the form of paresthesia (sensations of burning, burning, drilling, tingling, etc.). With paresthesia, the patient clearly points to the organ that is bothering him, describes the sensations clearly and emotionally. If discomfort is interpreted by the patient as pain, this is senestalgia. Senestalgia is distinguished by the location of pain and has its own name. With senestopathy, it is difficult for a person to describe what he feels; as a rule, the discomfort does not have a clear localization.
In the presence of pronounced somatic symptoms for two or more years, with social maladjustment and a persistent change in the emotional background, a diagnosis of somatization disorder is possible. If the disease lasts for at least six months and the clinical picture is atypical, an undifferentiated somatoform disorder is diagnosed. If a person experiences persistent anxiety about his health and fear of the “incurability of the disease,” a diagnosis of hypochondriacal disorder is made.
Differential diagnosis is carried out with the initial stages of somatic diseases, depression, hypochondriacal delirium and other mental disorders.
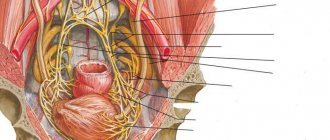
Somatoform dysfunction of the autonomic nervous system
The syndrome develops when there is a malfunction of the autonomic nervous system, which controls the functioning of internal organs, blood vessels, and is responsible for the course of physiological processes and the mobilization of the body as a whole.
The ANS consists of 2 sections: parasympathetic and sympathetic.
The sympathetic nervous system increases the heart rate, constricts blood vessels and increases blood pressure. Increases sweating and slows down intestinal motility. It relaxes the bladder, dilates the bronchi and pupil. Sympathy speeds up metabolism and activates the body as a whole.
The parasympathetic system has the opposite effect. But, despite the opposition of departments, normal well-being of a person is ensured by their coordinated work. Any malfunctions in the functioning of both systems cause various pathological sensations and syndromes, in particular, somatoform dysfunction.
There are 3 types of disorders:
- with a predominance of sympathy;
- with a predominance of parasympathetics;
- mixed.
According to the flow, stable and paroxysmal, with vascular and other types of crisis are distinguished.
Pathology can be primary, that is, it develops on its own, or secondary, after previous illnesses. Its symptoms manifest themselves under the influence of a psychotraumatic factor.
Such patients are characterized, first of all, by the appearance of vegetative signs: severe sweating, tremors of the limbs, paleness and redness of the skin.
Another group of signs expresses the dysfunction of internal organs under the control of the ANS:
- cough, shortness of breath, laryngeal spasm;
- tachycardia, arrhythmia, blood pressure changes. Heart pain does not have a clear localization and can be of various types. It happens that they are accompanied by a feeling of anxiety or fear. They are worse at rest, but go away during physical activity. Lasts from a few minutes to several days. Heart symptoms are so believable that they sometimes confuse even specialists;
- abdominal pain, bloating, difficulty swallowing; “bear disease” - diarrhea under the influence of stress;
- difficulty urinating, urinary incontinence;
- headaches, fatigue, poor sleep.
The complaints are numerous, but lack specifics. They signal a disruption in the functioning of several organs at once.
Patients are concerned about their condition, but still not to the same extent as hypochondriacs. They strive to find a way out of the situation and receive adequate treatment.
Diagnosis F 45.2 Hypochondriacal disorder
The most important feature is the patient's persistent concern about the possibility of having a severe, progressive disease or several diseases. The patient presents persistent somatic complaints or shows persistent anxiety about their occurrence. Normal, ordinary sensations and signs are often perceived by the patient as abnormal and disturbing; he usually focuses his attention on only one or two organs or systems of the body. Significant depression and anxiety are often present, which may explain additional diagnoses.
A disorder characterized by preoccupation with one's own health
Dysmorphophobia (non-delusional)
Hypochondriacal neurosis
Hypochondria
Nosophobia
Excluded:
- delusional dysmorphophobia (F22.8)
- delusions focused on the functioning or appearance of one's own body (F22.-)
SDVNS in children
Often, somatoform autonomic disorder appears in children at puberty, that is, during the period of maturation. This is due to a hormonal surge and intensive growth of the body.
The following factors can provoke the process:
- heredity;
- stress;
- mental, physical stress;
- infections;
- bad habits;
- surgical interventions;
- large body weight;
- sedentary lifestyle;
- staying at the computer for a long time.
The appearance of teenagers is typical. If sympathy predominates, then the skin of such children is moist and oily, with acne. She alternately turns red and pale. A bluish tint appears. Cold, with a marbled pattern called a vascular necklace. When pressed with a finger, the skin turns pale and red dermographism is observed.
When parasympathetics dominate, the skin is dry, with pink or white dermographism. These children have an increased appetite, but they do not gain weight.
The disorder is accompanied by a sudden rise in temperature under the influence of stress. A typical occurrence is fainting.
All characteristic changes in internal organs are present.
The psycho-emotional sphere is also undergoing changes. Such a child becomes distracted and nervous. He quickly gets tired, drowsiness and apathy appear, and his memory deteriorates.
In most cases, the course of the disease is stable. But periodically panic attacks and crises occur:
- sympatho-adrenal - accompanied by tachycardia, elevated blood pressure, headaches, thirst, chills and hyperthermia. Anxiety and feelings of fear develop;
- vagoinsular – migraine-like attacks, nausea, vomiting, pain in the abdominal area. Hyperhidrosis, decreased blood pressure and fainting, slow heart rate, increased urine output, breathing disorders;
- mixed.
The attack can last up to several hours.