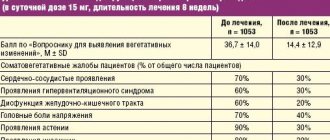
Anatomy and nodes of the sympathetic trunk
The sympathetic trunk (also called the borderline sympathetic trunk) is a paired organ, part of the body’s sympathetic system, located on the anterolateral part of the spine. Below you will find out what role the sympathetic trunk plays in the human body and what are the consequences of disruption of its functions.
Superior cervical sympathetic ganglion syndrome
Symptoms of the development of the syndrome are:
- disturbances in the functioning of the facial muscles;
- paroxysmal pain of a burning nature. In this case, the attack can pass in either a couple of hours or several days;
- radiating pain to the neck and shoulders. In this case, the pain is usually localized in the back of the head;
- drooping of the upper and raising of the lower eyelid, which reduces the size of the palpebral fissure;
- decreased tone of the orbital muscle;
- the color of the iris becomes lighter;
- reduction or cessation of sweating.
Stellate (cervicothoracic) node syndrome
This syndrome manifests itself with the following symptoms:
- pain in the area of the 5th-6th pair of ribs;
- pain in the arm on the affected side;
- impaired sweating in the affected area;
- reduction in pain sensation.
Posterior cervical syndrome
This syndrome occurs due to compression, the development of an infectious or inflammatory process, or a violation of the circulatory process. Most often, damage to the sympathetic plexus occurs due to the development of osteochondrosis.
Symptoms of the development of posterior cervical sympathetic syndrome are:
- severe headache that does not go away for a day or more. As a rule, pain is localized on the affected side and has an increasing or paroxysmal character;
- vomiting caused by a very severe headache;
- tinnitus, hearing loss;
- hot flashes, sudden redness of the face;
- numbness or shaking of the hands;
- pain in the face in the throat area;
- unnatural tilt of the head in the affected area;
- photophobia;
- pain in the area of the eyeball;
- blurred vision.
Jugular foramen syndrome
This disease occurs due to damage to the accessory, vagus or glossopharyngeal nerve. The syndrome is usually caused by trauma or tumors.
Treatment
Treatment is aimed simultaneously at:
- anesthesia. In this case, painkillers are prescribed, and in severe cases, tranquilizers. To speed up the effect, medications are administered intravenously;
- treatment of a viral or bacterial infection. For this, antiviral drugs or antibiotics are prescribed;
- To normalize the tone of sympathetic structures, cholinomimetic drugs are prescribed.
Physiotherapy procedures have a good effect: cold mud applications, UV irradiation, radon baths. It is advisable to take a massage course.
So, the sympathetic trunk is an element of the human sympathetic nervous system, which is responsible for the constancy of the internal environment of any person. Any problems with this organ are fraught with serious systemic disorders in the patient’s body and require immediate intervention.
You have no rights to post comments
Jan 06, 2021 5012
in Symptoms
All about the cellular spaces and fascia of the neck The cervical region of the human body is a complex complex of internal organs, muscle fibers, blood vessels and nerves...
Feb 01, 2021 33537
in Vessels
What causes a vein in the neck to pulsate and what to do? Swelling of the veins, accompanied by a noticeable pulsation from the outside, suddenly appearing in the submandibular area -...
Jan 05, 2021 7289
in Symptoms
Neck diseases The human neck performs a motor function and contains vital structures. Neck diseases have a very wide origin and…
Sympathetic trunk: structure, topography, nerves, plexuses and their formation.
Sympathetic trunk
Each of the two sympathetic trunks is divided into four sections: cervical, thoracic, lumbar (or abdominal) and sacral (or pelvic).
The cervical region extends from the base of the skull to the neck of the first rib; located behind the carotid arteries on the deep muscles of the neck. It consists of three cervical sympathetic nodes: superior, middle and inferior.
Ganglion cervicale superius is the largest node of the sympathetic trunk, having a length of about 20 mm and a width of 4-6 mm. It lies at the level of 11 and part of the Ill cervical vertebrae behind the internal carotid artery and medial to the n.vagus.
Ganglion cervicale medium is small in size, usually located at the intersection of the a.thyroidea inferior with the carotid artery, often absent or can split into two nodules.
Ganglion cervicale inferius is quite significant in size, located behind the initial part of the vertebral artery; often merges with the 1st and sometimes 11th thoracic node, forming a common cervicothoracic, or stellate, node, ganglion cervicothoracicum s.ganglion stellatum.
Nerves for the head, neck and chest arise from the cervical ganglia. They can be divided into an ascending group, going to the head, a descending group, going down to the heart, and a group for the organs of the neck.
The nerves to the head arise from the superior and inferior cervical ganglia and are divided into a group that penetrates the cranial cavity and a group that approaches the head from the outside.
The first group is represented by n.caroticus internus, extending from the upper cervical ganglion, and n.vertebralis, extending from the lower cervical ganglion. Both nerves, accompanying the arteries of the same name, form plexuses around them: plexus caroticus internus and plexus vertebralis; together with the arteries, they penetrate into the cranial cavity, where they anastomose with each other and give branches to the brain vessels, meninges, pituitary gland, trunks of the III, IV, V, VI pairs of cranial nerves and the tympanic nerve.
Plexus caroticus internus continues into the plexus cavernosus, which surrounds a.carotis interna in the area where it passes through the sinus cavernosus.
The branches of the plexuses extend, in addition to the innermost carotid artery, also along its branches. Of the branches of the plexus caroticus internus, it should be noted n.petrosus profundus, which joins n.petrosus major and together with it forms n.canalis pterygoidei, which approaches the ganglion pterygopalatinum through the canal of the same name.
The second group of sympathetic nerves of the head, the external one, is composed of two branches of the upper cervical ganglion, nn.carotici externi, which, having formed a plexus around the external carotid artery, accompany its branches on the head. From this plexus a stem extends to the ear node, gangl. oticum; from the plexus accompanying the facial artery, a branch departs to the submandibular node, gangl. submandibulare.
Through the branches entering the plexuses around the carotid artery and its branches, the superior cervical node supplies fibers to the vessels (vasoconstrictors) and glands of the head: sweat, lacrimal, mucous and salivary, as well as to the hair muscles of the skin and to the muscle that dilates the pupil, m .dilatator pupillae. The center of pupil dilation, centrum ciliospinale, is located in the spinal cord at the level from the VIII cervical to the II thoracic segment.
The organs of the neck receive nerves from all three cervical ganglia; in addition, some of the nerves arise from the internodal areas of the cervical sympathetic trunk, and some from the plexuses of the carotid arteries.
Branches from the plexuses follow the course of the branches of the external carotid artery, bear the same names and together with them approach the organs, due to which the number of individual sympathetic plexuses is equal to the number of arterial branches. Of the nerves extending from the cervical part of the sympathetic trunk, the laryngopharyngeal branches from the superior cervical ganglion are noted - rami laryngopharyngei, which often go from the n.laryngeus superior (branch n.vagi) to the larynx, often descending to the lateral wall of the pharynx; here they, together with the branches of the glossopharyngeal, vagus and superior laryngeal nerves, form the pharyngeal plexus, plexus pharyngeus.
The descending group of branches of the cervical part of the sympathetic trunk is represented by nn.cardiaci cervicales superior, medius et inferior, extending from the corresponding cervical nodes. The cervical cardiac nerves descend into the chest cavity, where, together with the sympathetic thoracic cardiac nerves and branches of the vagus nerve, they participate in the formation of the cardiac plexuses.
The thoracic section of the sympathetic trunk is located in front of the necks of the ribs and is covered in front by the pleura. It consists of 10-12 nodes of more or less triangular shape. The thoracic region is characterized by the presence of white connecting branches, rami communicantes albi, connecting the anterior roots of the spinal nerves with the nodes of the sympathetic trunk. Branches of the thoracic region:
1) nn.cardiaci thoracici depart from the upper thoracic nodes and participate in the formation of the plexus cardiacus (for a detailed description of the cardiac plexuses, see the description of the heart);
2) rami communicantes grisei, unmyelinated - to the intercostal nerves (somatic part of the sympathetic department);
3) rami pulmonales - to the lungs, forming plexus pulmonalis;
4) rami aortici form a plexus on the thoracic aorta, plexus aorticus thoracicus, and partly on the esophagus, plexus esophageus, as well as on the thoracic duct (the n.vagus also takes part in all of these plexuses);
5) nn.splanchnici major et minor, large and small splanchnic nerves; n.splanchnicus major begins with several roots extending from the V-IX thoracic nodes; the roots of n.splanchnicus major go in the medial direction and merge at the level of the IX thoracic vertebra into one common trunk, penetrating through the gap between the muscle bundles of the legs of the diaphragm into the abdominal cavity, where it is part of the plexus coeliacus; n.splanchnicus minor starts from the X - XI thoracic nodes and also enters the plexus coeliacus, penetrating the diaphragm with the greater splanchnic nerve. Vasoconstrictor fibers pass through these nerves, as can be seen from the fact that when these nerves are cut, the intestinal vessels are greatly filled with blood; nn.splanchnici contains fibers that inhibit the movement of the stomach and intestines, as well as fibers that serve as conductors of sensations from the viscera (afferent fibers of the sympathetic part).
The lumbar, or abdominal, section of the sympathetic trunk consists of four, sometimes three nodes. The sympathetic trunks in the lumbar region are located at a closer distance from one another than in the thoracic cavity, so that the nodes lie on the anterolateral surface of the lumbar vertebrae along the medial edge of m. psoas major. Rami communicantes albi are present with only two or three upper lumbar nerves.
A large number of branches extend from the abdominal section of the sympathetic trunk along its entire length, which, together with the nn.splanchnici major et minor and the abdominal sections of the vagus nerves, form the largest unpaired celiac plexus, plexus coeliacus. Numerous spinal nodes (C5 - L3) and the axons of their neurocytes also participate in the formation of the celiac plexus. It lies on the anterior semicircle of the abdominal aorta, behind the pancreas, and surrounds the initial parts of the celiac trunk (truncus coeliacus) and the superior mesenteric artery. The plexus occupies the area between the renal arteries, the adrenal glands and the aortic opening of the diaphragm and includes the paired celiac ganglion, ganglion coeliacum, and sometimes the unpaired superior mesenteric ganglion, ganglion mesentericum superius.
A number of smaller paired plexuses extend from the celiac plexus to the diaphragm, adrenal glands, kidneys, as well as the plexus testicularis (ovaricus), following the course of the arteries of the same name. There are also a number of unpaired plexuses to individual organs along the walls of the arteries, the name of which they bear.
Of the latter, the superior mesenteric plexus, plexus mesentericus superior, innervates the pancreas, small and large intestines up to half the length of the transverse colon.
The second ophthalmic source of innervation of the organs of the abdominal cavity is the plexus on the aorta, plexus aorticus abdominalis, composed of two trunks extending from the celiac plexus and branches from the lumbar nodes of the sympathetic trunk. The inferior mesenteric plexus, plexus mesentericus inferior, departs from the aortic plexus for the transverse and descending part of the colon, sigmoid and upper parts of the rectum (
plexus rectalis superior). At the origin of the plexus mesentericus inferior there is a node of the same name, gangl. mesentericum inferius. Its postganglionic fibers run in the pelvis as part of the nn.hypogastrici.
The aortic plexus initially continues into the unpaired superior hypogastric plexus, plexus hypogastricus superior, which bifurcates at the promontory and passes into the pelvic plexus, or inferior hypogastric plexus (plexus hypogastricus inferior s.plexus pelvinus).
Fibers originating from the upper lumbar segments are vasomotor (vasoconstrictor) for the penis, motor for the uterus and bladder sphincter.
The sacral, or pelvic, section usually has four nodes; located on the anterior surface of the sacrum along the medial edge of the anterior sacral foramina, both trunks gradually approach each other downwards, and then end in one common unpaired node - ganglion impar, located on the anterior surface of the coccyx. The nodes of the pelvic region, as well as the lumbar, are interconnected not only by longitudinal, but also by transverse trunks.
From the nodes of the sacral section of the sympathetic trunk a number of branches arise, which connect with branches that separate from the inferior mesenteric plexus and form a plate extending from the sacrum to the bladder; this is the so-called inferior hypogastric, or pelvic, plexus, plexus hypogastricus inferior s.plexus pelvinus. The plexus has its own nodes - ganglia pelvina. The plexus has several sections:
1) anterior lower section, in which there is an upper part that innervates the bladder - plexus vesicalis, and a lower part that supplies the prostate gland (plexus prostaticus), seminal vesicles and vas deferens (plexus deferentialis) and cavernous bodies (nn.cavernosi penis) in men;
2) the posterior section of the plexus supplies the rectum (plexus rectales medii et inferiores).
In women, there is also a middle section, the lower part of which gives branches to the uterus and vagina (plexus uterovaginalis), cavernous bodies of the clitoris (
nn.cavernosi clitoridis), and the upper one - to the uterus and ovaries.
Connecting branches, rami communicantes, depart from the nodes of the sacral section of the sympathetic trunk, joining the spinal nerves innervating the lower limb. These connecting branches constitute the somatic part of the sympathetic division of the autonomic nervous system, innervating the lower limb. The rami communicantes and spinal nerves of the lower limb contain postganglionic fibers that distribute in the vessels, glands and hair muscles of the skin, as well as in the skeletal muscles, providing its trophism and tone.
4.49 Morpho-functional concepts about analyzers: definition, components, example.
Sense organs, or analyzers, are devices through which the nervous system receives stimuli from the external environment, as well as from the organs of the body itself, and perceives these stimuli in the form of sensations.
Indications from the senses are sources of ideas about the world around us.
The process of sensory cognition occurs in humans through six channels: touch, hearing, vision, taste, smell, and gravity. The six senses provide a person with diverse information about the surrounding objective world, which is reflected in consciousness in the form of subjective images - sensations, perceptions and memory representations.
Living protoplasm has irritability and the ability to respond to irritation. In the process of phylogenesis, this ability especially develops in specialized cells of the integumentary epithelium under the influence of external irritations and intestinal epithelial cells under the influence of irritation with food. Specialized epithelial cells already in coelenterates are associated with the nervous system. In some areas of the body, for example on the tentacles and in the mouth area, specialized cells with increased excitability form clusters from which the simplest sensory organs arise. Subsequently, depending on the position of these cells, they specialize in relation to stimuli. Thus, cells in the oral region specialize in the perception of chemical stimuli (smell, taste), cells on protruding parts of the body specialize in the perception of mechanical stimuli (touch), etc.
The development of sense organs is determined by their importance for adaptation to living conditions. For example, a dog is sensitive to the smell of insignificant concentrations of organic acids secreted by the body of animals (the smell of traces), and is poorly versed in the smell of plants that have no biological significance for it.
The increasing sophistication of the analysis of the external world is due not only to the complication of the structure and function of the sense organs, but primarily to the complication of the nervous system. Nervous excitations arising due to certain irritations are perceived by us in the form of various sensations. For example, light energy, acting on the retina of the eye, causes nerve impulses, which, transmitted through the nervous system, cause visual sensations in our consciousness.
For sensations to arise, the following are needed: devices that perceive irritation, nerves through which this irritation is transmitted, and the brain, where it turns into a fact of consciousness. I.P. Pavlov called this entire apparatus necessary for the emergence of sensation an analyzer. “An analyzer is a device that has as its task to decompose the complexity of the external world into individual elements” (Pavlov I.P. Lectures on physiology).
Each analyzer consists of three parts:
1) receptor - transformer of irritation energy into the nervous process;
2) conductor-conductor of nervous excitation;
3) the cortical end of the analyzer, where excitation is perceived as a sensation.
There are two groups of sensations:
1. Sensations that reflect the properties of objects and phenomena of the surrounding material world: touch, i.e. sensation of touch and pressure, temperature sensation (heat, cold) and pain; then the sensations are auditory, visual, gustatory, olfactory and gravity.
2. Sensations that reflect the movements of individual parts of the body and the state of internal organs (motor sensations, a sense of body balance, sensations of organs). Accordingly, all sense organs are divided into two groups:
1. External sense organs that receive nerve impulses from the exteroceptive field are exteroceptors. There are six of them: the organs of the skin sense, the sense of gravity (gravity), hearing, vision, taste and smell.
2. Organs of internal sensations:
a) receiving impulses from the proprioceptive field (muscular-joint sense, closely related to the feeling of gravity) - proprioceptors;
b) organs that perceive nerve impulses from the interoceptive field (viscera and blood vessels) - interoceptors.
Sensations coming from the internal organs are usually vague and, in the normal state of these organs, do not reach consciousness, affecting only “general well-being.” In general, all internal processes regulated by the autonomic nervous system occur without our knowledge and only in painful disorders usually make themselves felt with more or less severe pain.
The interoceptive analyzer was described in detail in a special chapter. Of the excitations coming from the proprioceptive field, it is necessary to mention only the muscular-articular sense, thanks to which the sensation of the position of body parts is perceived and coordination of movements occurs. On the one hand, this feeling is combined with skin sensitivity (sense of stereognosis), on the other hand, it is in connection with the organ of gravity, which gives orientation in relation to the gravitational field, which can also be considered as a statokinetic apparatus that ensures balance of the body. Nerve endings (in muscles, bones, tendons and joints) and conductors of the muscular-articular sense were described in the presentation of the motor analyzer. In this section, only organs that perceive sensations received from the external world will be considered - exteroceptors.
The general plan of the perceiving devices in all classes of animals is more or less the same, despite subsequent significant complications in detail. The main element, with the exception of the cutaneous sense organs, in terrestrial animals are special sensitive cells, which in the process of development always originate from the epithelium of the outer layer (ectoderm), which, by its position, is in contact with the outside world. Each such cell at one end, facing the outer surface, carries a pin or receptive hairs, and on the other side gives off (in the organ of smell and vision) a process that connects with the processes of nerve cells of conducting neurons.
In other organs (taste and hearing), the sensitive cell, without giving rise to a central process, is entwined with the terminal branches of the afferent nerve approaching it. The first type of sensitive cells, compared with the second type, should be considered primary. In aquatic animals, this form of receptive elements is also found in the skin, where these elements are moistened by the surrounding liquid. In the skin of terrestrial animals there are no sensitive cells, and the receptor nerve fibers end either freely between the cells of the epithelial cover, or have a special kind of terminal bodies at their ends. The mesoderm also takes part in the formation of sensory organs, but only in a secondary manner, forming protective, supporting and auxiliary devices for them. These adaptations, growing and complementing sensitive cells, i.e. receptors form together with them the peripheral parts of the sense organs: skin, ear, eye, tongue, nose. For example, the visual receptor is the sensory cells of the retina (rods and cones), and the peripheral part is the entire eye.
In addition to dividing the sense organs into 2 groups, all analyzers can be classified from the point of view of I.P. Pavlov’s teaching about two signal systems as follows:
I. Analyzers of the first signal system (specifically, visual thinking):
A. Analyzers of the external world - exteroceptors (organs of skin sense, hearing, vision, taste, smell and gravity).
B. Analyzers of the internal world of the body:
1. Proprioceptors that carry irritation from the organs of animal life (muscular-articular sense).
2. Interoceptors that carry irritation from the organs of plant life (viscera, blood vessels).
II. Analyzers of the second signal system (abstract-logical thinking):
1. Spoken speech analyzers.
2. Written speech analyzers.
Analyzers of the first and second signal systems have sharp anatomical differences. Analyzers of the first signal system each have all three components (receptor, conductor and cortical end). Analyzers of the second signal system are deprived of their receptors and conductors, but have only cortical ends (cortical ends of speech analyzers); they perceive their signals (second signals) on the basis of the first signals that make up the first signaling system, without which they do not function. This emphasizes both the separation and unification of the cortical ends of all analyzers that make up the single cerebral cortex.
4.50 Organs of hearing and balance: general plan of structure. The external ear, its parts, structure, blood supply and innervation.
The vestibulocochlear organ, organum vestibulocochleare, consists of two analyzers: 1) a gravity analyzer (i.e., the sense of gravity) and balance and 2) a hearing analyzer. Each of them has its own receptor, conductor and cortical end. However, their joint description as a single organ has its own reasons, which lie in the nature of their development. At first, both analyzers formed as a single organ in one bone - the temporal bone, where they are localized in humans, and then they differentiated into two different analyzers. Both of these analyzers are closely interconnected, forming, as it were, a single organ. An essential part of it in vertebrates and humans is the labyrinth, in which two types of receptors lie: one of them (spiral organ) serves to perceive sound stimulation, the others (the so-called maculae et cristae ampullares) represent the perceiving devices of the statokinetic apparatus necessary for the perception of the forces of the earth. gravity, to maintain balance and orientation of the body in space.
At the lower stages of phylogenesis, these two functions are not yet differentiated from each other, but the static function is primary. The prototype of a labyrinth in this sense can be a static bubble (oto- or statocyst), which is very common in invertebrate animals living in water, such as mollusks.
In vertebrates, this initially simple form of the vesicle becomes significantly more complex in accordance with the complication of the labyrinth. Genetically, the vesicle originates from the ectoderm by invagination followed by laceration, then special tube-like appendages of the static apparatus begin to separate - the semicircular ducts. Hagfish have one semicircular duct connected to a single vesicle, as a result of which they can only move in one direction. Cyclostomes develop two semicircular ducts, thanks to which they are able to easily move their body in two directions. Finally, starting with fish, all other vertebrates develop three semicircular ducts, corresponding to the three dimensions of space existing in nature, allowing them to move in all directions. As a result, the vestibule of the labyrinth and semicircular ducts are formed, which have their own special nerve - the pars vestibularis of the vestibulocochlear nerve. With access to land, with the advent of locomotion using limbs in terrestrial animals, and bipedalism in humans, the importance of balance increases.
The entire evolution of man is determined by the adaptation of his body to the gravitational field of the Earth. To perceive the forces of gravity, a special analyzer (statokinetic) has been developed with a special receptor that perceives these forces and is therefore called the gravity receptor. The structure of the brain centers responsible for the automatic regulation of body position becomes more complex. In humans, the postural control centers reach their highest development.
While the organ of gravity in connection with the free movement of the body in space is already formed in aquatic animals, the acoustic apparatus, which is in its infancy in fish, develops only with the exit from the water to land, when direct perception of air vibrations becomes possible. It gradually separates itself from the rest of the labyrinth, spiraling into a snail. With the transition from the aqueous to the air environment, a sound-conducting apparatus is attached to the inner ear.
So, starting with amphibians, the middle ear-tympanic cavity with the eardrum and auditory ossicles appears. The acoustic apparatus reaches its highest development in mammals, which have a spiral cochlea with a very complex sound-sensitive device. They have a separate nerve - pars cochlearis of the vestibulocochlear nerve and a number of auditory centers in the brain - subcortical (in the diencephalon and midbrain) and cortical. They also develop an outer ear with a deepened auditory canal and auricle. The auricle is a later acquisition that plays the role of a sound collector and also serves to protect the external auditory canal. In terrestrial mammals, the pinna is equipped with special muscles and easily moves in the direction of sound (“prick up your ears”). It is absent in mammals leading an aquatic and underground lifestyle; in humans and higher primates, the auricle undergoes reduction and becomes immobile. At the same time, the emergence of oral speech in humans is associated with the maximum development of auditory centers, especially in the cerebral cortex, which form part of the second signaling system - this highest addition to the thinking of animals. Thus, despite the reduction of individual ear frequencies, the auditory analyzer turns out to be the most developed in humans.
The outer ear, auris extrena, consists of the auricle and the external auditory canal.
The auricle, auricula, usually called simply the ear, is formed by elastic cartilage covered with skin. This cartilage determines the external shape of the auricle and its protrusions; the free curved edge - the helix, and parallel to it - the antihelix, anthelix, as well as the anterior protrusion - the tragus, tragus, and the antitragus lying behind it, antitragus. At the bottom, the auricle ends with an earlobe that does not contain cartilage, which is a progressive feature characteristic of humans. In the depths of the shell behind the tragus, the opening of the external auditory canal opens.
The external auditory canal, meatus acusticus externus, is composed of two parts - cartilaginous and bone. The cartilaginous auditory canal is a continuation of the cartilage of the auricle in the form of a groove, open upward and posteriorly. Its inner end is connected through connective tissue to the edge of the tympanic part of the temporal bone. The cartilaginous auditory canal generally accounts for one-third of the length of the entire external auditory canal. The bony auditory canal, constituting two-thirds of the length of the entire auditory canal, opens outward through the porus acusticus externus; a circular bone groove runs along the edge of this hole,
sulcus tympanicus.
The direction of the entire auditory canal is generally frontal, but it does not go straight, but forms an S-shaped bend in both the horizontal and vertical planes. Due to the bends of the ear canal, in order to see the deep eardrum, it is necessary to straighten it, pulling the auricle back, up and out.
The skin covering the pinna continues into the external auditory canal. In the cartilaginous part of the passage, the skin is very rich in both sebaceous and a special kind of glands, glandulae ceruminosae, which secrete a yellowish secretion, the so-called earwax (cerumen).
The eardrum, membrana tympani, is located on the border between the outer and middle ear, being inserted with its edge into the sulcus tympanicus at the end of the external auditory canal, like in a frame. In the sulcus tympanicus, the eardrum is strengthened by a fibrous ring, anulus fibrocartilagineus. Due to the oblique position of the inner end of the ear canal, the membrane is inclined, in newborns it is almost horizontal. The eardrum in an adult has the shape of an oval with a long diameter (11 mm) and a short diameter (9 mm); it represents a thin semi-translucent plate, which at its center, called the navel, umbo membranae tympani, is drawn inward like a flat funnel.
Its outer surface is covered with a thin continuation of the skin of the ear canal (stratum cutaneum), and the inner surface is covered with the mucous membrane of the tympanic cavity (stratum mucosum).
The thickness of the membrane itself between these two layers consists of fibrous connective tissue, the fibers of which in the peripheral part of the membrane run in a radial direction, and in the central part - circularly.
At the top, the eardrum does not contain fibrous fibers, it consists only of skin and mucous layers with a thin layer of loose fiber between them; this part of the eardrum is softer and loosely stretched and therefore is called pars flaccida, in contrast to the rest of the tightly stretched part, pars tensa.
Vessels and nerves of the external ear. The external ear receives arterial blood from branches of two arteries - a.temporalis superficialis and a.auricularis posterior (both from a.carotis externa); the terminal branches of a.auricularis profunda (from a.maxillaris) approach the anterior wall of the bony part of the external auditory canal and the tympanic membrane.
Venous blood flows into the v.auricularis posterior and into the v.retromandibularis, as well as through the veins accompanying the a.auricularis profunda into the plexus pterygoideus. Lymph from the entire outer ear is carried to the lymph nodes lying in front and behind the auricle.
The eardrum, the entire anterior wall of the external auditory canal, as well as the anterior part of the auricle are innervated by the sensory branches of the n.auriculotemporalis (from the third branch of the n.trigemini). The rest of the auricle, together with the lobe, is supplied from the n.auricularis magnus (from the cervical plexus). The posterior and lower walls of the external auditory canal receive sensory branches from the ramus auricularis n.vagi.
Sympathetic nervous system
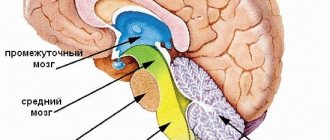
Brain stem: structure, functions, general information
Among people who are unfamiliar with the work of the nervous system, there is an opinion that it is one and indivisible. However, in reality everything is different. Thus, the sympathetic department, which in turn belongs to the peripheral, and the peripheral belongs to the autonomic part of the nervous system, supplies the body with the necessary nutrients. Thanks to its work, oxidative processes proceed quite quickly, if necessary, the work of the heart accelerates, the body receives the proper level of oxygen, and breathing improves.
Click to enlarge
Interestingly, the sympathetic division is also divided into peripheral and central. If the central part is an integral part of the work of the spinal cord, then the peripheral part of the sympathetic has many branches and nerve nodes that connect. The spinal center is located in the lateral horns of the lumbar and thoracic segment. The fibers, in turn, extend from the spinal cord (1st and 2nd thoracic vertebrae) and 2,3,4 lumbar vertebrae. This is a very brief description of where the sympathetic system is located. Most often, the SNS is activated when a person finds himself in a stressful situation.
Thoracic region
The thoracic sympathetic trunk includes ganglia thoracica (thoracic nodes) - triangular-shaped nerve formations that lie on the costal necks on the sides of the thoracic vertebrae, under the intrathoracic fascia and parietal pleura.
From the thoracic ganglia there are 6 main groups of branches:
- White connecting branches that branch from the intercostal nerves (their anterior roots) and penetrate the nodes.
- The gray connecting branches emerge from the ganglia and are directed to the intercostal nerves.
- Branches of the mediastinum. They originate from the 5 sympathetic superior ganglia and pass into the posterior mediastinum, together with other fibers forming the bronchial and esophageal plexuses.
- Cardiac thoracic nerves. They originate from 4-5 sympathetic superior ganglia, participating in the formation of the aortic and deep cardiac plexuses.
- The nerve is large splanchnic. Collected from branches 5-9 of the sympathetic thoracic ganglia and covered with intrathoracic fascia. Through the openings between the intermediate and medial crura of the diaphragm, this nerve passes into the abdominal cavity and ends in the ganglia of the celiac plexus. This nerve includes a large number of preganglionic fibers (which switch in the ganglia of the celiac plexus to postganglionic fibers), as well as postganglionic fibers, which have already switched at the level of the thoracic ganglia of the sympathetic trunk.
- The small intrasternal nerve. It is formed by branches of 10-12 nodes. Through the diaphragm it descends slightly lateral to n. splanchnicus major and is also part of the celiac plexus. Some of the preganglionic fibers of this nerve in the sympathetic ganglia switch to postganglionic, and some follow to the organs.
Histological significance
Spinal cord: structure and functions, basic physiology
The cervical section of the sympathetic trunk, like other parts of the peripheral nervous system, is subject to diagnosis if neurological and oncological pathologies are suspected. They provide certain information, and their condition depends on a number of factors:
- past diseases that also affect the condition of the nodes;
- age can significantly change the structure of the ganglia - due to this, a colossal number of atypical cells accumulate in the ganglia, which are valuable for diagnostic purposes;
- when protein levels change, a deterioration in the functionality of elements can be suspected, which is often associated with the development of diseases.
Materials sent for histology are subjected to detailed study. After this, doctors can detect certain damaged cells, linking them with pathologies of the central nervous system and lymphatic system.
Lumbar
The lumbar ganglia of the sympathetic trunk are nothing more than a continuation of the chain of ganglia of the thoracic region. The lumbar region includes 4 nodes, which are located on both sides of the spine on the inner edge of the psoas major muscle. On the right side, the nodes are visualized outward from the vena cava inferior, and on the left - outward from the aorta.
The branches of the lumbar sympathetic trunk are:
- White connecting branches arising from the 1st and 2nd lumbar spinal nerves and approaching the 1st and 2nd ganglia.
- Gray connecting branches. They unite the lumbar ganglia with all lumbar spinal nerves.
- Internal lumbar branches that arise from all ganglia and enter the superior hypogastric, celiac, aortic abdominal, renal and superior mesenteric plexuses.
Dentistry
- Surgical dentistry
- Oncological aspects in dentistry
- Functional diagnostics in dentistry
- Medical labor examination in dentistry
- Reconstructive surgeries of the maxillofacial area
- Actinomycosis of the maxillofacial region
- Copolymers in dentistry
- Cryosurgery in dentistry
- Organization of dental care for the population
- Organization of dental care in military units
- Diseases of the temporomandibular joint in children and adolescents.
- Diseases of the oral mucosa
- Dental and oral surgery
- Surgical dental diseases
- General surgical dentistry
- Surgical dentistry of a polyclinic doctor
- Purulent maxillofacial surgery
- Medical examination of children at the dentist
- Military oral and maxillofacial surgery
- Histology and embryology of the oral cavity and teeth
- Pathological anatomy of diseases of the dentofacial system and oral cavity
- Neurogenic diseases of the maxillofacial region
- Facial and brain injuries
- Temporomandibular joint diseases
- X-ray diagnosis of diseases of the facial skull
- X-ray diagnostics of diseases of teeth and jaws
- Emergency care in neuro-dentistry Lesions of the trigeminal nerve system. Neuralgia
- Neurodental diseases with damage to the autonomic system Rossolimo-Melkerson-Rosenthal syndrome
- Sjögren's syndrome
- Stomalgia (glossalgia, glossodynia)
- Lesions of the autonomic ganglia of the face
- Lesions of the cervical part of the borderline sympathetic trunk
- Differential diagnostic criteria for lesions of the autonomic ganglia
Sacral section
The lowest section (according to the topography of the sympathetic trunk) is the sacral region, which consists of one unpaired coccygeal ganglion and four paired sacral ganglia. The nodes are located just medial to the sacral anterior foramina.
There are several branches of the sacral portion of the sympathetic trunk:
- Connecting gray branches heading to the sacral and spinal nerves.
- The splanchnic nerves are part of the autonomic plexuses in the pelvis. Visceral fibers from these nerves form the hypogastric inferior plexus, which lies on branches from the internal iliac artery, through which the sympathetic nerves penetrate the pelvic organs.
Anatomy of the sympathetic trunk
In the human body, the trunks consist of 20-25 ganglia. They are located on the anterolateral region of the spine, running from the base of the skull to the coccyx, where they form the azygos ganglion. Connective fibers extend from them, which ensure the transmission of nerve impulses. Also from each ganglion branches go to the spinal nerves.
The cervical trunk is the first of 4 parts of the organ, which includes 3 paravertebral nerve ganglia and their branches. They are located between the deep neck muscles and occupy the area under the prevertebral plate of the cervical fascia.
Upper nodular section
The largest element of the sympathetic trunk is the superior cervical ganglion. It has an irregular shape and reaches 2 cm in size with a thickness of 0.5 cm. It is located in front of the 2-3 cervical vertebrae, next to their transverse processes. In front of it is the largest artery - the carotid. The large vagus nerve is located at the side and is supported by a long muscle at the back. Several branches with nerve fibers depart from it:
- gray tracts are small connecting branches that connect the ganglion with the first spinal roots located above;
- internal carotid nerve, going to the artery from the upper pole of the node;
- external carotid endings - pass in 2-3 layers to the back of the artery of the same name;
- The cervical cardiac nerve, located superiorly and coming from the cervical fascia, passes through the brachial region and goes deep into the cardiac plexus and aorta, the left part is located at the left side of the carotid artery.
The internal carotid nerve is of primary importance in the structure of the cervical ganglion, as it is connected to the carotid canal of the skull and passes through it. Enters the mucous membrane of the middle ear. It also affects the opening of the fibrocartilage and goes to the pterygoid zone of the sphenoid bone, where it intertwines with the petrosal nerve. At this point it acquires another name - the wedge-shaped canal node. And from here it goes into the pterygopalatine fossa, connecting with the node of the same name.
Middle node
The cervical ganglion, located in the middle of the section, is located anterior to the process of the 6th vertebra and is considered unstable. It may be partially displaced. Behind it is the thyroid artery. The size is significantly smaller than that of the superior ganglion - only 5 mm in diameter. Structure branches:
- gray connective - extend mainly to the 5th, less often to the 6th vertebra, in some people they can connect to the 7th element of the ridge;
- middle cardiac cervical nerve - located on the lateral side and runs parallel to the upper one;
- 1-2 thin nerves, forming the carotid plexus and the ganglion of the thyroid artery, extend to the 6th vertebral process.
The branches of the middle cervical ganglion form the subclavian loop.
Stellate or cervicothoracic node
It is located at the very bottom of the cervical region, in contact with the neck of the first rib. Behind it is the subclavian artery. The stellate ganglion is a combination of the inferior cervical and first thoracic ganglion. Its size is about 8 mm. There are as many as 5 branches coming off:
- the cervical cardiac nerve, located at the very bottom and running behind the brachiocephalic trunk, on the left passes under the aorta, goes deep into the cardiac plexus;
- gray connecting branches go to 6-8 vertebral endings;
- several fibers are located from the subclavian loop and go to the vessels of the hands;
- several elements connect to the branches of the vagus and phrenic nerve fibers;
- The vertebral nerve also originates from here, intertwining with the artery of the same name and forming the sympathetic plexus of the ridge.
All nodes together are responsible for forming a system that is responsible for important tasks.
Middle node
A formation measuring 2*2 mm, located at the level of the 4th cervical vertebra, at the place where the common carotid and inferior thyroid arteries intersect. This node gives rise to four types of branches:
- Connecting gray branches that go to the 5th, 6th spinal nerves.
- The middle cardiac nerve is located posterior to the common carotid artery. In the chest cavity, the nerve participates in the formation of the cardiac plexus (deep), which is located between the trachea and the aortic arch.
- Branches that participate in the organization of the nerve plexuses of the subclavian, common carotid and thyroid inferior arteries.
- The internodal branch that connects to the cervical superior sympathetic ganglion.
Top knot
Spindle-shaped formation measuring 20*5 mm. It is located on 2-3 cervical vertebrae (their transverse processes) under the prevertebral fascia.
Seven main branches depart from the node, which carry postganglionic fibers innervating the organs of the neck and head:
- Connecting gray rami to the 1st, 2nd, 3rd spinal cervical nerves.
- N. jugularis (jugular nerve) is divided into several branches, two of which are attached to the glossopharyngeal and vagus nerves, and one to the hypoglossal nerve.
- N. caroticus internus (internal carotid nerve) enters the outer shell of the internal carotid artery and forms a plexus of the same name there, from which, in the area where the artery enters the canal of the same name on the temporal bone, sympathetic fibers depart, which form a stony deep nerve passing along the pterygoid canal in the sphenoid bones. After leaving the canal, the fibers pass the pterygopalatine fossa and join the parasympathetic postganglionic nerves from the pterygopalatine ganglion, as well as the maxillary nerve, after which they are sent to the organs in the facial area. In the carotid canal, branches separate from the carotid internal plexus, which penetrate and form a plexus in the tympanic cavity. Inside the skull, the carotid (internal) plexus transforms into the cavernous, and its fibers spread through the vessels of the brain, forming the plexus of the ophthalmic, middle cerebral and anterior cerebral arteries. In addition, the cavernous plexus gives off branches that connect to the parasympathetic fibers of the parasympathetic ciliary ganglion and innervate the muscle that dilates the pupil.
- N. caroticus externus (carotid external nerve). It forms an external plexus near the artery of the same name and its branches that supply blood to the organs of the neck, face and dura mater of the brain.
- The pharyngeal-laryngeal branches accompany the vessels of the pharyngeal wall and form the pharyngeal plexus.
- The superior cardiac nerve passes near the cervical portion of the sympathetic trunk. In the chest cavity it forms the superficial cardiac plexus, which is located under the aortic arch.
- Branches that are part of the phrenic nerve. Their endings are located in the capsule and ligaments of the liver, pericardium, parietal diaphragmatic peritoneum, diaphragm and pleura.
Functions
In accordance with the sections of the sympathetic trunk and its constituent ganglia and nerves, several functions of this anatomical formation can be distinguished:
- Innervation of the neck and head, as well as control over the contraction of the vessels feeding them.
- Innervation of the organs of the thoracic cavity (branches from the nodes of the sympathetic trunk are part of the nerves in the pleura, diaphragm, pericardium and liver ligaments).
- Innervation of the vascular walls (as part of the nerve plexuses) of the common carotid, thyroid and subclavian arteries, as well as the aorta.
- They connect the nerve ganglia with the nerve plexuses.
- Participate in the formation of the celiac, aortic, superior mesenteric and renal plexuses.
- Innervation of the pelvic organs due to the entry of branches from the cruciate ganglia of the sympathetic trunk into the inferior hypogastric plexus.
Peripheral department
It is not so difficult to imagine the peripheral part. It consists of two identical trunks, which are located on both sides along the entire spine. They start from the base of the skull and end at the tailbone, where they converge into a single unit. Thanks to the internodal branches, the two trunks are connected. As a result, the peripheral section of the sympathetic system passes through the cervical, thoracic and lumbar regions, which we will consider in more detail.
- Cervical region. As you know, it starts from the base of the skull and ends at the transition to the thoracic (cervical 1st ribs). There are three sympathetic nodes here, which are divided into lower, middle and upper. All of them pass behind the human carotid artery. The upper node is located at the level of the second and third cervical vertebrae, has a length of 20 mm, a width of 4 - 6 millimeters. The middle one is much more difficult to find, as it is located at the intersections of the carotid artery and the thyroid gland. The lower node has the largest size, sometimes even merging with the second thoracic node.
- Thoracic department. It consists of up to 12 nodes and has many connecting branches. They reach out to the aorta, intercostal nerves, heart, lungs, thoracic duct, esophagus and other organs. Thanks to the thoracic region, a person can sometimes feel the organs.
- The lumbar region most often consists of three nodes, and in some cases has 4. It also has many connecting branches. The pelvic region connects the two trunks and other branches together.
Structure
In accordance with the structure of the sympathetic trunk (Truncus sympathicus), it is paired and consists of nodes that are connected to each other through sympathetic fibers. These formations are located on the sides of the spinal column along its entire length.
Any of the nodes of the sympathetic trunk is a collection of autonomic neurons that switch preganglionic fibers (most of them) that exit the spinal cord, forming connecting white branches.
The fibers described above are in contact with the cells of the corresponding node or go as part of the internodal branches to the underlying or superior node of the sympathetic trunk.
The connecting white branches are located in the upper lumbar and thoracic regions. There are no branches of this type in the sacral, lower lumbar and cervical nodes.
In addition to the white branches, there are also connecting gray branches, which consist mostly of sympathetic postganglionic fibers and connect the spinal nerves with the nodes of the trunk. Such branches go to each of the spinal nerves, departing from each of the nodes of the sympathetic trunk. As part of the nerves, they are directed to the innervated organs (glands, smooth and striated muscles).
The following sections are conventionally distinguished as part of the sympathetic trunk (anatomy):
- Sacral.
- Lumbar.
- Chest.
- Cervical.
Anatomy in humans
The sympathetic trunks consist of 20-25 autonomic ganglia of the 1st order and are located on the anterolateral surfaces of the ridge, from the base of the skull to the coccyx, where they connect to form one unpaired ganglion
.
At the level of C8-L2,
white communicating branches
the intermediolateral nuclei
of the lateral horns of the spinal cord .
gray connecting branches
depart from the ganglia , which are the axons of the neurons of these ganglia and transitively (without switching) passing axons of the intermediolateral nuclei of the lateral horns of the spinal cord, heading to the 2nd order ganglia (prevertebral), and being preganglionic. Each ganglion gives off gray communicating rami to specific spinal nerves (a postganglionic fiber from the sympathetic trunk approaches each spinal nerve).
Cervical region
It consists of three nodes, which are reached by preganglionic fibers from C8-Th7 by the ascending internodal branches of the sympathetic trunk.
Superior cervical ganglion (ganglion cervicale superius)
Located anterior to the transverse processes of C2-C3. It is the largest among the trunk ganglia (2.5 cm × 0.5 cm).
Gives off postganglionic fibers that form the following nerves:
- The internal carotid nerve (n. caroticus internus), which accompanies the internal carotid artery and branches off the deep petrosal nerve (n. petrosus profundus) to the pterygopalatine ganglion, the carotid-tympanic nerves, and the ophthalmic plexus, from which the sympathetic branch departs to the ciliary ganglion.
- External carotid nerves (nn. carotici externi), which form the external carotid plexus.
- General carotid plexus.
- Jugular nerve (n. jugularis).
- Laryngopharyngeal nerves.
- The superior cervical cardiac nerve (n. cardiacus cervicalis superior), of which the left one goes to the superficial cardiac plexus, and the right one to the deep one.
- Gray connecting branches to the I-IV spinal nerves.
Middle cervical ganglion (ganglion cervicale medius)
Located at the level of the transverse process of C6.
Gives away:
- The middle cervical cardiac nerve (n. cardiacus cervicalis medius), which goes to the deep cardiac plexus.
- Gray connecting branches to the V-VI spinal nerves.
Lower cervical ganglion (ganglion cervicale inferior)
Located at the level of the head of the first rib, behind the subclavian artery.
Gives away:
- Subclavian loop (two internodal branches to the middle cervical node, which clasp the subclavian artery on both sides).
- The lower cervical cardiac nerve (n. cardiacus cervicalis inferior), which goes to the deep cardiac plexus.
- The spinal nerve, which forms the spinal plexus around the spinal artery.
- Gray connecting branches to the VII-VIII spinal nerves.
Thoracic region
Lumbar, sacral spine and coccyx. On the anterolateral surface of the spine is the sympathetic trunk.
Consists of 10-12 spindle-shaped nodes located in front of the rib heads.
This is where they start:
- Thoracic cardiac nerves (nn. cardiaci thoracici) from the II-V thoracic nodes, which go to the deep cardiac plexus.
- Pulmonary and esophageal nerves from II-V thoracic nodes.
- Nerves to the thoracic aorta.
- Greater splanchnic nerve (n. splanchnicus major) from preganglionic fibers that transit through the V-IX thoracic nodes.
- Small splanchnic nerve (n. splanchnicus minor) from preganglionic fibers that transit through the X-XI thoracic nodes.
- The lowest splanchnic nerve (n. splanchnicus imus) from the XII thoracic node; not permanent.
Lumbar
Consists of 3-5 lumbar nodes. The nodes of the right and left trunks are connected to each other by transverse branches.
Each node gives off lumbar splanchnic nerves (nn. splanchnici lumbales), which pass in transit (are preganglionic).
Sacrococcygeal region
Both trunks form 4 paired and 1 unpaired node, located midway from the sacral foramina. The right and left nodes are connected to each other by transverse branches.
The sacral splanchnic nerves (nn. splanchnici sacrales) depart from the nodes, which pass in transit (they are preganglionic).
Bottom knot
The formation is located behind the vertebral and above the subclavian arteries. In rare cases, it is combined with the first sympathetic thoracic node and is then called the stellate (cervicothoracic) node. The bottom node gives rise to six branches:
- Connecting gray branches going to the 7th, 8th spinal cervical nerves.
- A branch going to the plexus vertebralis, spreading in the skull and forming the plexus of the cerebral posterior artery and the basilar plexus.
- The inferior cardiac nerve lies behind the aorta on the left, and behind the brachiocephalic artery on the right and is involved in the formation of the deep cardiac plexus.
- The branches that enter the phrenic nerve do not form plexuses, but end in the diaphragm, pleura and pericardium.
- Branches forming the plexus of the common carotid artery.
- Branches to the subclavian artery.
Diagnosis and symptoms
It is possible to make an accurate diagnosis only on the basis of clinical data, while diagnosis in some cases can be very difficult.
As for the symptoms of ganglionitis, they depend solely on its cause and type.
However, each species is characterized by such general characteristics as:
- burning pain, which can be paroxysmal;
- severe itching in the area affected by ganglionitis;
- in some cases, paresthesia may develop (tingling or numbness of the skin in the affected area);
- in most cases, the functions of thermoregulation and sweating are impaired;
- swelling of the subcutaneous tissue is observed;
- loss of muscle tone, decreased reflexes and reduced joint mobility.
Possible complications
In some cases, the disorder itself can be a complication.
For example, in women this disease is often caused by advanced inflammatory processes in the reproductive system.
Article on the topic: Flemoclav - instructions for use and indications, composition, dosage, release form and price
But ganglionitis can also have serious consequences.
The most common, dangerous and painful complication for the patient is postherpetic neuralgia.
In this case, the most unpleasant symptom is casual pain. Such painful sensations are pronounced, and they intensify many times when touched, but may temporarily recede when the affected limbs are immersed in water or wrapped in a wet rag.
Sometimes such pain persists for a long period, up to several years.
Very rarely, peripheral muscle paresis may be observed in the affected area when their motor functions deteriorate.
Complications after the disease also include zoster myelitis and encephalitis.
As a result of damage to a large number of nerves, Guillain-Barré syndrome occurs. Treatment of the disease is difficult, but possible.
Serous meningitis in children can become a serious problem if its symptoms are not identified in time and treatment is not started.
What diseases can affect the cervical ganglia?
There are no specific pathologies of the node. However, when nearby organs and tissues are affected, complex syndromes may occur:
- Superior cervical sympathetic ganglion. The disorder is accompanied by stiffness of the facial muscles, burning pain radiating to the neck and shoulders. The patient's upper eyelid droops or lower eyelid rises, which leads to changes in the palpebral fissure. In some cases, eye color changes and sweating may stop.
- Cervicothoracic node syndrome. Accompanied by pain in the first 5-6 pairs of ribs, in the arm, and changes in sweating.
- Posterior cervical syndrome. Characteristic of infection, compression or inflammatory processes. Pain occurs in the pharynx area, tremors, numbness of the hands, tinnitus and hearing impairment may appear. Some patients experience vomiting and an unbearable headache that lasts longer than 1-2 days. Vision also deteriorates, photophobia and discomfort in the eyeball appear.
To treat these syndromes, it is important to find out the cause of poor health. For infections and viruses, antibiotics are prescribed, and for pain relief - NSAIDs or analgesics
The cervical ganglia carry a huge layer of important diagnostic information. Their damage and atypical condition may indicate hidden pathological processes