Home — For the public
- Map of medical organizations
- Vaccination
- Clinical examination
- Fluorography
- Addresses and opening hours of clinics
- Emergency rooms
- Oncology
- Where to take an HIV test
- Healthy child's office
- Services
- Prevention of CVD
- Disease Prevention
- World Patient Safety Day
- Newspaper "Medical News"
- specialist
- School of Health
— Disease prevention
- HIV infection
- All about vaccination
- All about proper nutrition
- Hepatitis
- Flu
- Dementia
- Schoolchildren's health
- STD
- Tick-borne encephalitis
- Whooping cough
- Measles
- Legionellosis
- Meningococcal infection
- Oncology
- Acute intestinal infection
- Pediculosis
- First aid
- Pneumococcal infection
- Pneumonia
- Prevention of rabies
- Dependency Prevention
- Rotavirus infection
- Diabetes
- Cardiovascular diseases
- Injuries
- Tuberculosis
- Tularemia
- Physical activity
- Obstructive pulmonary disease
- Exotic infections
- Ecology
- Why is swimming in ponds dangerous?
— Cardiovascular diseases — Vascular diseases of the brain
Even at rest, the human brain consumes up to 25% of the oxygen entering the body; To ensure its operation, about 15% of the total volume of circulating blood is required. Vascular diseases, narrowing of their lumen leads to hypoxia and neuron death.
People without special education cannot always recognize the first symptoms of cerebrovascular accident and miss the time when therapeutic or preventive care is most effective.
Blood supply to the brain
Four large arteries are responsible for the transport of oxygen and nutrients to the brain tissues: two internal carotid and two vertebral. The vertebral arteries are responsible for supplying blood to the brain stem. At the base of the brain they merge into the basilar artery.
Each internal carotid artery is divided into anterior and posterior. These vessels supply the frontal, temporal, parietal, and occipital lobes.
At the base of the brain, the internal carotid branches, the basilar artery and the branches connecting them form a closed circle of Willis. It is named after the English doctor Thomas Willis. This anatomical formation ensures the redistribution of blood and the preservation of nutrition of parts of the brain during blockage of blood vessels. The outflow of blood from the cranial cavity occurs through the jugular veins.
Brain diseases occur when large and small vessels are damaged. Depending on the cause, symptoms occur acutely and require immediate medical attention or develop gradually, slowly leading to a deterioration in a person's quality of life.
The main causes of arterial damage include atherosclerosis and hypertension. In the first case, plaques form on the inner surface of the vascular wall, narrowing the lumen of the arteries. They have a thin cover and contain lipids inside. When such plaques rupture, blood platelets adhere to the damaged surface, leading to blockage of the lumen (thrombosis). The provoking factor is often vasospasm.
Arterial hypertension also damages the walls of blood vessels: they become denser, and areas of expansion (aneurysms) appear. These vulnerabilities can cause arteries to rupture or become blocked.
A condition in which small cerebral arteries are affected and the blood supply to the brain is affected is called discirculatory encephalopathy. Nerve cells do not receive enough oxygen and nutrients and die. A developed network of arteries cannot solve this problem. The process is not limited to any one area of the brain; lesions are found in various parts.
Signs and symptoms of acute cerebrovascular accidents depending on the area of brain damage
- The basin of the internal carotid artery – paresthesia, paresis, paralysis on the opposite side of the face and body. Pathology of speech and vision in one eye.
- Vertebrobasilar basin - systemic dizziness, pain in the back of the head, unsteady gait, loss of visual fields, double vision, inability to swallow and speak.
- Brain stem - eye paralysis, hearing loss, swallowing and speech disorders, paresthesia of the facial skin.
- Medulla oblongata – bilateral paralysis.
- Temporal lobe – loss of spatial and temporal orientation, memory impairment.
Risk factors for cerebrovascular diseases
Assessing the likelihood of vascular damage, neurologists and cardiologists say that some people are more predisposed to this group of diseases. Risk factors include such conditions, diseases and lifestyle features as:
- low physical activity;
- hypertonic disease;
- heart disease;
- diabetes mellitus of any type;
- hypercholesterolemia;
- smoking;
- regular stress, psycho-emotional stress;
- frequent drinking of alcohol.
In addition, the risk group includes people with a family history of hypertension, heart attack, stroke in close relatives.
Hemorrhagic stroke
Intracerebral hemorrhages are most common, subarachnoid hemorrhages are less common, and subdural hemorrhages are even less common.
In 60-70% of patients, the cause of hemorrhage was arterial hypertension, in 20% of cases - arterial aneurysm and arteriovenous malformation, in others - various diseases associated with atherosclerosis.
Among the reasons that determine the development of hemorrhagic stroke, the main place is occupied by hypertension and atherosclerosis.
Hemorrhagic stroke develops predominantly acutely, often without warning. It is characterized by a sudden loss of consciousness, sometimes after one or more vomitings. The patient's face becomes bluish-red, the pulse is tense and slow, breathing is loud and bubbling, the body temperature soon rises, the head and eyes are often turned to the side. Focal symptoms are primarily characterized by motor disturbances in the form of paresis and paralysis of the limbs on the side opposite to the hemorrhage, which arise as a result of compression of the internal capsule or vessels supplying it with blood by the hematoma.
Symptoms
The first signs of vascular damage to the brain may appear already at a young, working age. In this case, patients tend to ignore painful symptoms and not consult a doctor. And even when visiting a therapist or neurologist, the condition often remains unrecognized.
Among the early signs:
- absentmindedness;
- memory loss;
- fatigue;
- decreased performance;
- headache;
- noise in the head;
- episodes of dizziness;
- weather sensitivity.
Signs of circulatory problems may appear one by one. Young patients often associate them with overwork, as they believe that it is too early for them to be sick.
Over time, negative lifestyle factors lead to a deterioration of the condition - normal activities begin to suffer, severe weather sensitivity worries, and a person’s character “deteriorates.”
But sometimes the situation changes dramatically. In such cases, they speak of acute cerebrovascular accidents. How to recognize typical vascular diseases?
Encephalopathy
This diagnosis has already become “the talk of the town”: it is used to scare patients with hypertension, and it is “gifted” to old women who make scandals in pharmacies, clinics and on the street. And no wonder. The first symptoms of the disease are often noticeable behavioral, emotional and volitional disturbances. Thus, patients experience:
- irritability;
- emotional lability;
- sleep disorders;
- fatigue;
- depressive symptoms.
Relatives may notice that such a relative has become angry, sensitive to changes in weather, and his personality traits have become “sharpened.” Sentimental people become whiny, punctual people become pedantic, thrifty people become frankly stingy.
Over time, productivity begins to suffer: memory and attention deteriorate. The person becomes absent-minded, “constantly writes down so as not to forget,” but still forgets. Episodes of inappropriate, rude behavior are possible.
Discirculatory encephalopathy progresses, the course can be uniform or with sudden episodes of deterioration. It cannot be cured, you can only slow down the development of the disease. Severe encephalopathy is characterized by the development of dementia. Such a patient has completely lost self-care skills, in some cases cannot control physiological functions, and needs constant care and supervision.
Osteochondrosis often provokes or intensifies the manifestations of encephalopathy, as it impairs blood flow to the brain due to narrowing of the lumen of the vertebral arteries. Slow personality changes due to vascular damage also occur in systemic diseases accompanied by vasculitis.
Stroke
Stroke is one of the most common causes of death in people around the world. In fact, this is an acute circulatory disorder in the cerebral vessels, in which the entire brain lesion dies. According to the mechanism of development, there are 2 types of strokes: ischemic and hemorrhagic.
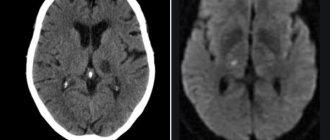
In ischemic stroke, the lumen of the vessel is blocked. Brain cells are very sensitive to hypoxia. At first, they try to provide for themselves through anaerobic glycolysis; within a few hours, the pathological processes are reversible. But decay products gradually accumulate, and the pH of the tissue changes to the acidic side. Neurons swell, their membranes cease to perform their functions and are destroyed. The final formation of the stroke focus occurs within 2-7 days; specialist assistance is most effective during the first 3-6 hours.
With a hemorrhagic stroke, the integrity of the vessel is compromised. Blood pours under the membranes, into the parenchyma (tissue) of the brain, and breaks into the ventricles. The cause of such a catastrophe is changes in the structure of the vascular wall and fluctuations in blood pressure. Congenital or acquired cerebral aneurysm can cause sudden death or severe disability. Until it reaches a large size, there is no pressure on the brain, and there are no clinical manifestations. The condition may worsen acutely, the patient is concerned about:
- headache;
- nausea;
- double vision;
- convulsions;
- disturbances of consciousness.
A special place is occupied by transient ischemic attacks, or as they say - micro-strokes. The name “microstroke” is unscientific; it reflects the reversibility of what occurs in the patient’s tissues. Some people who have had ischemic attacks are not aware of this. Thus, patients are greatly surprised to learn about them when describing a routine computed tomography or magnetic resonance imaging. (“I thought it was a simple hypertensive crisis!”)
Symptoms and prognosis for cerebrovascular accidents depend on the volume and location of the lesion. It is worth recalling obvious signs, the detection of which requires immediate medical attention:
- severe headaches, often with dizziness, tinnitus;
- asymmetry of the face, it is impossible to raise your hands, smile, show your teeth;
- weakness, numbness in the arms and legs, unsteadiness of gait;
- violation of pronunciation and perception of addressed speech;
- nausea and vomiting;
- disturbance, loss of consciousness.
Treatment
In case of acute cerebrovascular accident, treatment should be started immediately. The minutes count down.
For chronic pathology, the course of therapy is drawn up individually after diagnosis. The doctor takes into account age, concomitant diseases, and stage of the process.
Basic treatment includes, among other things, 3 mandatory recommendations.
- Nutrition correction. It should help normalize lipid metabolism and reduce blood cholesterol. Usually the consumption of meat, deli meats, and animal fats is limited. It is recommended to eat more vegetables, herbs, and dairy products.
- Increased physical activity. Helps normalize blood flow and increase vascular tone.
- Weight loss. Correcting your diet and increasing physical activity usually helps you lose extra pounds and be in good physical shape. If this is not enough, seek the help of an endocrinologist.
In case of cerebrovascular accident, with various symptoms, treatment is prescribed:
- physiotherapy;
- physical therapy;
- medicines;
- surgical treatment.
Diagnosis of vascular diseases of the brain
To “take care of your health and get examined,” you don’t need to wait until you reach pre-retirement or retirement age - many vascular disorders begin to develop in young people. What do we have to do? It is necessary to undergo regular preventive examinations, even if “nothing bothers you,” and do not be embarrassed to “bother” the doctor with complaints about a change in condition.
Diagnosis of cerebral vascular pathology includes:
- Analysis of patient complaints. You should tell your doctor even such “minor” symptoms as: fluctuations in blood pressure, headaches, dizziness, forgetfulness, and weather sensitivity.
- Anamnestic information: age, presence of risk factors, rate of development of symptoms, concomitant diseases (hypertension, diabetes, systemic and rheumatic lesions).
- Examination of the patient with analysis of neurological symptoms, examination of the fundus. Body mass index assessment.
- Laboratory data: blood sugar, blood lipid profile, coagulogram, platelet count assessment. CSF analysis to detect hemorrhagic stroke.
- Instrumental diagnostic methods: CT or MRI of the head, scanning of the vessels of the head and neck, ECG.
Prevention
To avoid the sudden appearance of cerebrovascular accidents, you need to lead an active lifestyle. Do as much physical activity as possible, morning exercises. Walk more, swim, take a contrast shower. Be sure to monitor blood pressure.
You should stop smoking and drinking alcoholic beverages.
It is recommended to consume more foods rich in vitamins C, D, E, and fiber. Minimize the intake of fried, fatty, spicy, salty foods. If you have chronic diseases, they must be treated. If you have hypertension, monitor your blood pressure.
Diagnostics
A neurologist deals with cerebral atherosclerosis. His task is to collect anamnesis, as well as conduct a series of tests. Doctor:
- will ask you to look up (a sick person will not be able to fulfill the request);
- will check the reflexes (they will be either excessively high or low, and asymmetrically);
- will ask you to stretch your arms forward and look to see if there is any tremors in the fingers, or if the patient is losing balance;
- will ask you to touch your nose with the tip of your finger with your eyes closed (the patient will not be able to cope with this task).
This is only a small component for assessing the patient’s health. Therefore, more detailed examinations are required next:
- consultation with an ENT doctor, ophthalmologist and other specialists depending on the identified disorders;
- biochemical blood test for triglycerides and cholesterol (lipid spectrum);
- According to indications, instrumental examinations are carried out.
To assess the condition of cerebral vessels, the following is carried out:
- Ultrasound of the brain and neck using two-dimensional and transcranial duplex scanning technology;
- angiography of cerebral vessels;
- Doppler ultrasound;
- MRI of the brain in vascular mode;
- REG (radioencephalogram);
- CT computed tomography of the brain and blood vessels;
- EEG – electroencephalogram.
The diagnostic capabilities of our multifunctional center of the FMBA of Russia allow us to carry out not only these, but also any other examinations necessary for the patient using the most modern and accurate equipment. You will be able to get advice from related specialists on any clinical case, including suspected cerebral atherosclerosis.
Arteriovenous malformations
An arteriovenous aneurysm (malformation) is a congenital malformation of cerebral vessels in which arterial blood is directly discharged into the venous bed, bypassing the capillary network. Such aneurysms consist of a dilated adductor arterial vessel, a tangle of vessels forming an arteriovenous shunt, and one or more sharply dilated efferent veins. The walls of the tangle of vessels of arteriovenous malformation are thinned, and it is almost impossible to determine their arterial or venous origin.
Since in arteriovenous malformation there is no capillary network, part of the blood entering the cerebral hemispheres does not take part in tissue metabolism, so-called hemorrhagic stealing of the brain occurs. This causes persistent cerebral ischemia and causes psychopathological disorders, as well as progressive brain atrophy.
The clinical picture of arteriovenous malformation is varied and depends on its location. Often, arteriovenous malformations are clinically manifested by epileptic seizures or spontaneous intracranial hemorrhages.
The prehemorrhagic period may be asymptomatic or manifest itself as epileptic seizures