Stroke can be ischemic or hemorrhagic.
The first is much more common than the second, but both are deadly.
Our expert is Candidate of Medical Sciences, Head of the Department of Neurosurgery of the Russian Scientific Center for Surgery of the Russian Academy of Medical Sciences. B.V. Petrovsky Sergey Vasiliev .
The symptoms of one and the other form of this dangerous disease may be very similar to each other, but their treatment methods are completely different. Therefore, it is so important for the doctor to find out as early as possible what kind of disease he had to deal with.
Types of stroke
All types of stroke occur with an acute decrease or cessation of blood supply to brain tissue. As a result, necrosis (death) of nerve cells is observed, which, as a result of hypoxia, lose the ability to perform their functions. A stroke leads to an acute cessation of innervation of the limbs and internal organs and a decrease in brain activity. The patient may partially or completely lose previously acquired skills, which are then slowly restored as new neural connections are created. Stroke is classified into ischemic and hemorrhagic; subarachnoid hemorrhage in the brain is also distinguished separately. These types differ in their causes, but present with a similar clinical picture.
Ischemic stroke
According to statistics, ischemic strokes take first place and account for up to 80% of all cases. However, they are considered less dangerous and more often occur with a favorable outcome and complete recovery. The cause of ischemic stroke is an acute decrease in blood circulation without compromising the integrity of blood vessels. Depending on the cause, it is customary to classify this pathology into 5 more varieties.
- Atherothrombic stroke is one of the complications of atherosclerosis. In this disease, the vascular walls become less strong and elastic due to deposits of cholesterol and other harmful substances. The formation of atherosclerotic plaques (thrombi) is dangerous due to complete or partial blockage of the vessel, which leads to cerebral ischemia. Symptoms of this type of stroke often begin at night and develop gradually over several hours or days.
- Cardioembolic stroke is a consequence of diseases and heart defects, which are characterized by the formation of wall thrombi. This type is considered life-threatening because it often includes a hemorrhagic component (bleeding in the brain) and occurs with significant damage to brain tissue.
- Hemodynamic stroke is a pathology that develops as a result of circulatory disorders. Its cause can be any disease of the arteries that carry blood to the brain, including atherosclerosis, stenosis (narrowing of the lumen), as well as congenital or acquired anomalies of their structure. Risk factors may include insufficient physical activity, decreased blood pressure, and ischemic myocardial disease.
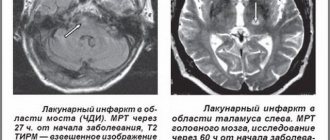
- Lacunar stroke - develops when blood circulation in small arteries is impaired. The area of the lesions does not exceed 1.5 cm, so the consequences of the attack are minimal. Such strokes are most often located in subcortical structures and do not affect the cerebral cortex.
- Strokes that develop according to the type of hemorheological microocclusion - during such attacks, significant circulatory disorders are not diagnosed. Its causes are various changes in the properties of blood, disorders of its coagulation and fibrin production processes. The neurological picture is weak, but there are additional signs associated with a violation of the composition and properties of the blood.
Ischemic stroke can have varying degrees of severity, depending on its cause and the size of the lesions. More often, the pathology manifests itself in old age, as well as against the background of diseases of the cardiovascular system. Doctors at the Clinical Brain Institute say that most cases of ischemic stroke progress at night, and its manifestations should be a reason to call an ambulance. During the rehabilitation process, repeated circulatory disorders and a relapse of the attack may occur.
Hemorrhagic stroke
Hemorrhagic stroke is diagnosed less frequently - no more than 25% of cases. The mechanism of its development is a violation of the integrity of the cerebral arteries and the development of hemorrhage into the membranes of the brain. As a result, hematomas of different sizes are formed, which put pressure on neurons and can cause their death. This leads to disruption of neural connections and loss of vital functions. If qualified assistance is not provided in a timely manner, there is a high probability of death.
It is often difficult to determine the cause of hemorrhagic stroke. The attack develops abruptly, without increasing symptoms, at any time of the day. In some patients, it is associated with various diseases of the cardiovascular system, if there is a history of them. Detailed diagnostics make it possible to determine the location of the damaged vessel and the size of the hematoma, but doctors will try to determine predisposing factors in order to avoid relapse.
Hemorrhagic strokes are distinguished by the location of the hemorrhage. Modern classification identifies several varieties:
- parenchymal - the place of its localization is brain tissue;
- intraventricular - hematomas are located in the lumen of the ventricles;
- subdural - the fluid is under the hard shell;
- epidural - blood enters the lumen above the hard shell;
- subarachnoid - hematomas between the arachnoid and soft membranes.
It is worth understanding that at least 15% of cases of hemorrhagic stroke occur for no apparent reason, and it cannot be determined even during instrumental diagnostics. Immediate medical attention and stopping bleeding is important - every minute of self-medication increases the likelihood of death. Despite the fact that hemorrhagic strokes occur less frequently, they pose a great danger to the patient’s life, and the presence of hematomas worsens the rehabilitation process after an attack.
Consequences of ischemic stroke of the right and left side
The consequences of an ischemic stroke will vary depending on the damaged hemisphere. If it is the left one (it is affected much more often), then the right side of the body may be lost. This hemisphere is responsible for logic and speech, hence the other consequences:
- speech is disrupted;
- I have to learn to read and write again;
- loss of speech memory occurs - the patient immediately forgets what he was talking about;
- if help is provided late or incorrectly, he will withdraw into himself and stop communicating.
Restoring memory and speech is difficult in such cases; the patient may not even understand speech. Physical activity is restored much faster.
If the right hemisphere is damaged, then the symptoms clearly appear later, so more time usually passes before seeking help, and the consequences are more serious:
- the patient seems to be completely paralyzed, although this is not the case;
- he forgets what he just did, while he can well remember long-ago events;
- The perception of reality and sense of space are disrupted, depression is observed, and the patient becomes very passive.
Recovery takes a very long time.
Causes and risk factors
The causes of a stroke can be congenital and acquired diseases that occur with various disturbances in the movement of blood through the vessels. In most cases, the attack occurs suddenly, so most disorders are diagnosed after the acute phase has subsided. According to statistics, stroke is more common in older people, but can occur at any age. It can be triggered by the following factors:
- vascular pathologies, including atherosclerosis;
- decreased or increased blood pressure;
- violations of blood composition and its main indicators;
- the patient’s lifestyle (smoking, drinking alcohol and drugs, obesity, lack of physical activity);
- metabolic pathologies;
- specific diseases, including carotid artery stenosis.
Atherosclerosis is one of the most common causes of both ischemic and hemorrhagic strokes. A provoking factor may be a disorder of lipid metabolism with the accumulation of excess cholesterol in the blood. This substance is deposited on the inner surface of the vascular walls and can form characteristic plaques. They clog arteries, preventing fluid from flowing through them, and can also cause a vessel to rupture under blood pressure.
Abnormal blood pressure readings can lead to dangerous consequences. Thus, hypotension is considered a common cause of ischemic stroke, and hypertension can cause hemorrhages in the brain. It should be understood that a chronic increase in pressure affects the condition of the vascular walls; they become less durable and lose elasticity. If you are prone to frequent pressure surges, you should have a tonometer with you and avoid serious physical activity and stressful situations.
Metabolic disorders can also become a predisposing factor to the development of stroke. One of these pathologies is diabetes mellitus. All changes in blood glucose levels are reflected in the condition of the artery walls, and their gradual wear and tear can cause a sudden attack. In some patients, several disorders can be diagnosed simultaneously, which together cause a stroke.
What are the types of strokes?
A stroke is an acute disorder of cerebral circulation, which instantly leads to damage and death of valuable nerve cells. The cause of its occurrence may be old age, chronic existing diseases, or heredity. Every year this disease claims the lives of 6 million people in the world, many patients remain disabled. Therefore, it is important to know what a stroke can be and how it manifests itself in order to take timely measures and save the person.
The following types are known:
- ischemic – a type of stroke, also known as cerebral infarction;
- hemorrhagic.
Stroke also includes a pathology such as transient ischemic attack, when blood circulation in the brain is disrupted for a short period of time, but the consequences can be noticeable. Doctors note that several such attacks can be equivalent to one stroke in terms of impact. In no case should attacks be ignored - in fact, the body provides a person with a chance to avoid more serious health problems.
Clinical picture
A stroke may appear suddenly or develop over several hours or days. Brain hemorrhages often present with a full range of symptoms, and the patient is rarely conscious until the ambulance arrives. He may experience numbness in part of the face or limbs, a severe headache, or discomfort behind the eyes. The pulse may increase or become too slow. In ischemic stroke, symptoms may be mild, but the degree of danger of an attack for a person does not depend on this factor.
A reminder for diagnosing a stroke
It is important to recognize a stroke immediately, even if it does not manifest itself with acute symptoms. A mild course is characteristic of an ischemic attack - the patient is often conscious and complains only of a short-term headache or a simple deterioration in health. In such a situation, you should ask the patient to perform several simple tasks:
- smile - with a stroke, the smile may be uneven, and one of the corners of the mouth is often downward;
- simultaneously raise two arms or two legs up - the patient rarely manages to perform the movement synchronously, one of the limbs will lag behind;
- articulation - difficulties arise with pronouncing even simple phrases, speech may become slow and incomprehensible.
If at least one of these signs corresponds, you must urgently call an ambulance. Doctors at the Clinical Institute of the Brain insist that if a stroke is suspected, timely hospitalization is important, and this factor may be decisive in determining the prognosis. In some cases, symptoms appear once and then become less obvious - this is characteristic of a transient cerebrovascular accident.
Characteristic symptoms of the acute stage of stroke
The clinical picture of the acute stage of stroke differs, depending on the cause of its development and the location of the main focus. As a rule, with ischemic stroke it is less pronounced, but there may be exceptions. A summary table may be useful to differentiate between different types of seizures.
| Sign | Ischemic | Hemorrhagic | Subarachnoid hemorrhage |
| Beginning of the attack | Slow | A few minutes or hours | A couple of minutes |
| Headache | Weakly expressed | Very strongly expressed | |
| Vomit | Rarely | Characteristic | |
| Increased blood pressure | Characteristic | In most cases | Not in all cases |
| Loss of consciousness | Not typical | Often, for a long time | For a short time |
| Increased tone of the occipital muscles | Rarely | Often | Always |
| Various speech disorders | Often | Not typical | |
| Retinal hemorrhage | Rarely | Sometimes | Often |
Diagnosing a stroke at home can be difficult if the clinical picture is not clear enough. However, any changes in behavior that indicate a cerebrovascular accident may be the first sign. It is important not to waste time and immediately contact doctors - this is the only way to provide timely assistance and avoid the dangerous consequences of a stroke.
Symptoms
Following the warning signs, the first symptoms appear. Feeling can deteriorate very quickly after this, so the speed of response is one of the main factors that can ensure survival.
The first symptoms may appear several hours before an ischemic stroke: weakness, headaches and dizziness, fainting. Limbs may be lost on one side or vision may be impaired - in some cases only affecting one eye.
Other signs that can help identify ischemic stroke:
- the patient perceives reality incorrectly;
- his speech becomes unclear;
- pulse quickens;
- the pressure rises and falls;
- auditory perception deteriorates;
- he has difficulty swallowing;
- there is noise in the head;
- movements are not coordinated;
- nausea;
- heat;
- the face is distorted;
- pain appears that a person has not experienced before, for example, the chest or half of the face begins to ache.
The following symptoms indicate a hemorrhagic stroke:
- the head begins to hurt very badly;
- arrhythmia or tachycardia occurs;
- pressure rises;
- breathing becomes loud and hoarse;
- the patient may faint;
- photosensitivity increases;
- the face becomes asymmetrical, turns red or pale;
- convulsions begin;
- the gaze loses its meaning;
- nausea or even vomiting begins;
- limbs or the whole body are paralyzed;
- bowel movements involuntarily.
Diagnosis and treatment of stroke
Until help arrives, the patient should remain in a supine position. It is better to tilt your head to the side, while simultaneously monitoring the patient’s breathing and consciousness. During this period, it is forbidden to take water and food, due to the possibility of damage to the muscles of the digestive tract. Further assistance is provided by doctors.
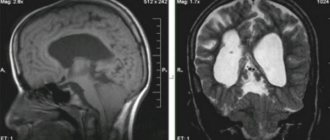
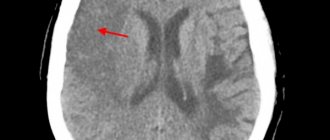
Diagnosis and differential diagnosis
The most important diagnostic value for strokes is magnetic resonance or computed tomography. These techniques make it possible to determine the location and size of the lesion, assess the degree of blood circulation and give a preliminary prognosis. An electroencephalogram is considered an additional method, but it is less informative than CT and MRI. Stroke must be differentiated from brain tumors, abscesses and subdural hemorrhages.
Methods of treatment and rehabilitation
The success of treatment measures for stroke depends on the timeliness of their initiation. After the acute phase has been relieved and the degree of circulatory impairment has been determined, recovery can begin. Treatment necessarily takes place in a hospital, and the Clinical Brain Institute offers comprehensive programs for patients of different ages and with any degree of stroke. Restoring brain activity is possible thanks to drugs (neuroreparants and neuroprotectors). Further rehabilitation is carried out in several directions:
- motor - carried out under the supervision of a physiotherapist;
- speech - regular classes with a speech therapist;
- restoration of lost skills and ability to self-care - with an occupational therapist and at home.
The effectiveness of the recovery period depends, among other things, on the patient’s age. The process is based on the formation of new neural connections. The human brain is plastic, meaning it is capable of learning certain skills at any stage of development. However, the degree of recovery depends on the stage of the stroke and the amount of damage to nerve tissue.
The Clinical Brain Institute offers individual treatment and rehabilitation programs for patients after a stroke. The clinic has all the conditions for full diagnosis and treatment of patients, including those with limited mobility. During the recovery process, you can stay on a day or daily basis in order to be able to undergo all procedures at the exact appointed time. Rehabilitation doctors, speech therapists, nurses and other specialists work with patients, and treatment is carried out with constant monitoring of all indicators.
Diagnostics
If warning signs appear, you should consult a doctor as soon as possible. He will conduct a simple test to make a preliminary diagnosis. The patient will need:
- Smile - if the lips on one side do not obey, the smile will turn out crooked.
- Extend your arms - they should be kept at the same level.
- Say something meaningful - for example, your full name.
- Stick out your tongue - it should not deviate to the side or sink.
By how these exercises are performed, it will be possible to determine whether the patient has suffered a stroke or whether the cause should be sought elsewhere. If signs indicate a stroke, the diagnosis is clarified using tomography and other procedures.
Hemorrhagic type of cerebral stroke
Such strokes occur due to the effusion of blood into a certain cavity of the skull; most often the disease is provoked by hypertension, although it happens that an aneurysm, vasculitis, and taking certain medications lead to a hemorrhagic stroke. Brain hemorrhage also occurs due to stress, poor blood clotting, smoking, and excess weight. A hemorrhagic stroke causes severe headache, numbness of the fingers, double vision, nausea and vomiting, convulsions; neurologically, memory loss, deterioration of speech, lethargy are manifested, and the part of the body opposite to the affected side of the brain does not move. Immobility after an attack often leads to thrombosis, bedsores, pneumonia; recovery requires enormous effort and time.
Doctors divide hemorrhagic stroke into the following types:
- intracerebral - a thin artery wall bursts, an aneurysm or a pressure surge can provoke an attack;
- subarachnoid - blood splashes into the cavity, which is located between the membranes of the brain and spinal cord; an attack is often provoked by smoking, alcohol, and hypertension.
Before prescribing treatment, the doctor diagnoses what type of attack it is and selects the necessary course of drugs.
Acute cerebrovascular accidents (ACI)
A stroke is an acute disorder of cerebral circulation, the symptoms of which persist for more than one day.
There are three types of stroke: ischemic stroke, hemorrhagic stroke and subarachnoid hemorrhage.
Ischemic stroke most often develops when the arteries, the vessels that carry blood to the brain, become narrowed or blocked. Brain cells die without receiving the oxygen and nutrients they need. This type of stroke is also called cerebral infarction, by analogy with myocardial infarction.
The reasons for blockage of a vessel can be different. The vessel can be closed by an embolus - a piece of intracardiac thrombus that occurs in certain heart diseases, or a piece of atherosclerotic plaque located on the wall of a large vessel. The cause of blockage of the vessel may be thrombosis - the formation of a blood clot (similar to the one that forms when the skin is cut with injury to the superficial vessels). A thrombus usually forms on the surface of an atherosclerotic plaque. Thrombosis is promoted by increased blood clotting and an increased ability for blood platelets (platelets) to stick together (aggregate).
With frequent increases in blood pressure, changes can develop in the walls of small vessels that supply deep structures of the brain. These changes lead to narrowing and often closure of these vessels. Sometimes, after another sharp rise in blood pressure (hypertensive crisis), a small infarction develops in the circulatory system of such a vessel (called a “lacunar” infarction in the scientific literature). Ischemic stroke occurs 4 times more often than the other type of stroke, hemorrhagic.
Hemorrhagic stroke most often develops when arteries rupture. The spilled blood soaks part of the brain, which is why this type of stroke is also called a cerebral hemorrhage. Most often, hemorrhagic stroke occurs in people suffering from arterial hypertension and develops against the background of increased blood pressure. At some point, the vascular wall cannot withstand the sharp rise in blood and ruptures. A more rare cause of hemorrhagic stroke is a ruptured aneurysm. An arterial aneurysm is usually a congenital saccular protrusion on the wall of a vessel. The wall of such a protrusion is thinner than the wall of the vessel itself, and a slight increase in blood pressure in stressful situations or during physical exertion is often enough to rupture it.
A rupture of a vessel on the surface of the brain allows blood to enter the space surrounding the brain (subarachnoid space). This type of stroke is called subarachnoid hemorrhage. The most common cause is a ruptured aneurysm.
The brain catastrophe itself occurs quite quickly: from several minutes to several hours (less often than several days). The time after a stroke is conventionally divided into acute (up to 3 weeks), recovery (up to 1 year) and residual (over a year) periods. During the acute period, both pathological processes occur (for example, an increase in cerebral edema) and processes that promote recovery (improved blood supply to the areas surrounding the lesion, a decrease in the size of the hemorrhage, a decrease in the compression of the surrounding brain matter by the hematoma).
Very rarely, a stroke is asymptomatic. When the first symptoms of a stroke appear, you should immediately consult a doctor. After all, a stroke is brain damage!
Risk factors for stroke
Risk factors for stroke can be divided into controllable (those that can be influenced by the doctor by issuing recommendations or by the patient himself by changing lifestyle) and uncontrollable (which cannot be influenced, but must be taken into account).
Controlled (adjustable) risk factors:
- high blood pressure (above 140/90 mmHg)
- smoking cigarettes
- alcohol abuse
- atrial fibrillation and other heart diseases
- lifestyle factors (excess weight, physical inactivity, poor diet and stress factors)
- increased blood cholesterol
- diabetes
- previous transient ischemic attack (TIA) and stroke
- use of oral contraceptives
Uncontrolled (unregulated) risk factors:
- age
- floor
- heredity
Stroke Prevention
1. Monitor your blood pressure. As statistics show, out of 100 patients with hypertension, only half know about their high blood pressure (although hypertension, as a rule, is visible a mile away - by the characteristic complexion, tense facial expressions, and often solid dimensions). And only 10-15 people out of 100 keep it, so to speak, in check with daily monitoring and medication. If you suffer from arterial hypertension, monitor your blood pressure regularly (twice a day!). A simple thing: you should have a blood pressure monitor at work and at home. According to the criteria of the World Health Organization, pressure above 140/90 mmHg is recognized as arterial hypertension. However, it is necessary to keep in mind that there are no hard numbers, and you cannot adhere to this guideline. If a person has had a blood pressure of 90/60 all his life (this is especially common in women), then its increase to 130/80 often results in a hypertensive crisis. On the other hand, it would be illiterate to “bring down” the pressure to 130/80 for those who have had it at 170/100 for a long time: after all, sharp fluctuations are extremely dangerous. However, in any case, the “pass” beyond 140/90 is a reason to see a doctor and take special medications.
2. Reduce the number of cigarettes you smoke per day if you smoke, and in the future completely give up this bad habit.
3. Drink alcohol in moderation (no more than 2 glasses of wine per day or 50 ml of spirits).
4. It is necessary to know about the presence or absence of any heart rhythm disturbances. To do this, it is enough to take an ECG once every six months. The main direction of preventing stroke in atrial fibrillation is to reduce the likelihood of blood clots forming in the cavities of the heart, which is achieved by taking medications.
5. Find out your blood cholesterol level. If it increases, consult a doctor. Follow all of his recommendations for controlling your cholesterol levels.
6. If you suffer from diabetes, follow your doctor's recommendations and do not let your blood sugar levels rise above normal.
7. Exercise. Lead an active lifestyle. Physical activity should be chosen according to your ability, age, health and on the advice of a specialist.
8. Eat a balanced diet, avoiding too much salty and spicy food, especially at night.
9. Maintain emotional balance, taking a position “above the fray” whenever possible. If you overreact to events, are very worried, or angry, do a very simple thing: try squeezing a tennis ball. You will not only throw out unnecessary emotions, but also... you will not be able to be angry anymore, since you have already switched psychologically.
If the first symptoms of a stroke occur, consult a doctor immediately!!!
The symptoms of the disease are quite obvious and allow even an ordinary person, not a specialist, to diagnose a stroke, in some cases even a type of stroke.
Signs and symptoms do not differ significantly by gender:
- weakness and impaired coordination of limb movements;
- short-term speech disorders, difficulties with understanding speech and speaking;
- numbness of one half of the body (face, tongue, hands, etc.);
- temporary or complete loss of vision;
- dizziness, double vision;
- walking disorders and problems;
- unsteadiness of gait
- severe headaches, nausea, vomiting, increased blood pressure, etc.;
- disturbance of consciousness.
It is extremely desirable for every person to know what the main signs of this disease are. Knowing how to recognize a stroke or symptoms of cerebrovascular disease and signs of acute cerebrovascular accidents (ACVA), you can help a sick person, and in especially serious cases, save his life.
If you suspect a stroke, ask the person to do three simple things (if possible):
- smile (a person will not be able to do this - there will be either asymmetry or a distortion of one side of the face);
- say a simple sentence (speech should be slurred and meaningless, or absent altogether);
- raise both arms (the person will be able to raise only one or will raise one arm lower than the other).
In some cases, if you ask a person to stick out their tongue, the tongue will be skewed to one side (although this does not always indicate a stroke, it may be one of the symptoms of a diagnosis of cerebrovascular disease, CVD).
A person who has had a stroke will not be able to fulfill these requests if the stage of development of the condition is deep. A severe stroke is accompanied by loss of consciousness and convulsions. The rate of stroke development is high, so it is quite easy to suspect it.
In any case, if a person feels unwell, whether or not you suspect a stroke, you need to call an ambulance.
The quality, quantity and degree of consequences and complications after a stroke depend not only on the severity of the injury, but also on the symptoms, on the interval between the incident and the diagnosis, on the time and volume of assistance provided and treatment provided, on the rehabilitation completed, its nature and intensity.
A small or quickly “caught” stroke occurs with minimal consequences, and sometimes they may even be absent, but these are extremely rare cases. Most often, violations are more serious and persistent.
The main and most significant disorders after a stroke:
decreased muscle strength on one side opposite the one where the brain is damaged (right-sided or left-sided hemiparesis after a stroke): difficulty moving (sometimes aids are needed), caring for oneself (dressing, eating, personal care, etc.) and etc.;
facial asymmetry and disorders of facial muscles;
speech impairment (can be not only a consequence, but also the first sign of a stroke): partial or complete loss of the ability and ability to speak and understand the speech of another person;
impaired coordination of movement if there has been damage to the brain stem (impairments vary in degree and may subside for some time after brain damage);
visual impairment: loss of half or a quarter of the visual image;
impairment of hearing, smell and habitual skills in normal life.
Stages of stroke (stroke and cerebral hemorrhages)
The stages of circulatory disorders depend on their type:
acute form (stroke itself), which occurs suddenly and symptoms can last up to one day;
chronic cerebrovascular accident.
Acute forms of stroke with all the characteristic signs usually develop within a few hours, but not more than one day. Acute forms are easily recognized, and the main thing here is not to miss the moment and quickly seek help from a doctor.
Stages of chronic cerebrovascular disease (cerebrovascular disease):
the first stage is similar to chronic fatigue syndrome: fatigue, insomnia, headaches and dizziness, frequent mood swings and absent-mindedness; transient numbness in the arms or legs;
the second stage is characterized by impaired movement, tinnitus, loss of concentration, decreased performance, constant dizziness and pain in the head;
The third stage is characterized by personality degradation, development of dementia, hand tremors, speech impairment, etc.
Treatment. Treatment Goals
Correction of disorders of vital functions and body systems.
Minimization of neurological defect.
Prevention and treatment of neurological and somatic complications.
Treatment goals
Normalization of respiratory function.
Normalization of blood circulation.
Regulation of homeostasis.
Reducing cerebral edema.
Symptomatic therapy.
In ischemic stroke, restoration of blood flow in areas of cerebral hypoperfusion (reperfusion).
In case of cerebral hemorrhage - reducing high blood pressure, stopping bleeding and removing the hematoma, in some cases eliminating the source of bleeding (aneurysm).
In SAH – stopping bleeding, eliminating the source of bleeding (aneurysm).
Neuroprotection and reparative therapy.
The best conditions for treatment and rehabilitation - Oberig Clinic
This is a multidisciplinary medical center for children and adults, operating in Kyiv since 2008, where they receive patients from all over Ukraine, as well as foreigners. The clinic operates a powerful stroke center, equipped with the latest equipment, where specialists in the field of neurology successfully treat and restore patients who have suffered a cerebral infarction or hemorrhagic stroke.
More than 80% of our patients return to their normal lifestyle, the results of the work of experienced doctors are comparable to the results in stroke centers in Europe, but the cost of our services is much lower. You can make an appointment on the website; if necessary, specialists will provide comprehensive advice on all issues.
3.Is it possible to prevent a stroke?
After your first stroke, there is a risk of it happening again. But making some lifestyle changes can help prevent strokes and improve your overall health. Doctors' recommendations are quite traditional, but nevertheless, it really works:
- It is worth controlling high blood pressure and high cholesterol. Timely diagnosis and examination and properly selected drug therapy will help with this.
- You should also maintain normal blood sugar levels.
- Doctors sometimes prescribe aspirin or blood thinners to prevent strokes.
- It is recommended to adhere to a healthy lifestyle - stop smoking, limit alcohol intake, watch your weight, exercise and diet.
About our clinic Chistye Prudy metro station Medintercom page!