Congenital complex vascular malformation. The formation is a tangle of vessels that directly connects the arterial and venous systems and, thus, shunts part of the blood bypassing the medulla. AVMs can manifest as intracerebral hemorrhages or epileptic seizures. To decide on treatment tactics, accurate data on the size, type of blood supply and the relationship of the formation to various brain structures is required.
General information Indications and choice of treatment method Principles of microsurgical removal of AVM Endovascular treatment of cerebral AVM Radiation treatment of cerebral AVM Conclusion
General information
| Schematic representation of an AVM |
Arteriovenous malformation (AVM) is a congenital malformation of blood vessels, which is a conglomerate of arteries and veins lacking an intermediate capillary link. AVMs can manifest as hemorrhages, manifested by corresponding symptoms and/or epileptic seizures. In most patients, the disease manifests itself at the age of 20–40 years, the peak of hemorrhages occurs at the age of 15–20 years. Hemorrhage from an AVM often leads to permanent disability (up to 50% of cases) and is often fatal (up to 10% of cases). The risk of hemorrhage from an unruptured AVM is 2-4% per year, the risk of re-hemorrhage: 6-18%.
Indications and choice of treatment method
To date, three methods of treating AVMs are used: direct microsurgical removal, endovascular embolization and radiation treatment. Indications for the use of each method have been sufficiently developed. In some cases, a combination of techniques is used. To determine the possibility of direct microsurgical excision of the malformation, the Spetzler-Martin classification is used, which takes into account the size of the AVM, its localization in relation to functionally important areas of the brain and the characteristics of blood drainage.
| Classification of Spetzler-Martin AVMs | |
| Feature being assessed | Points |
| Size Small (<3 cm) Medium (3-6 cm) Large (>3 cm) | 1 2 3 |
| Localization (by functional significance) Insignificant Significant | 0 1 |
| Type of venous drainage Only into superficial veins Also into deep veins | 0 1 |
The size of the AVM is determined by the maximum size of the tangle in centimeters. Functionally important areas include areas of the brain, damage to which is likely to lead to severe, persistent neurological deficits. Venous drainage is assessed as “superficial” if all drainage is into the cortical veins or sinuses. If at least one of the drainage veins flows into the network of deep veins, then the outflow is considered “deep”. The Research Institute of Neurosurgery has developed the following tactics for treating patients with AVM after hemorrhage. For patients with hemispheric AVMs SM 1-3, excision of the malformation is indicated. If necessary, the stroma is first embolized and available afferents are switched off. AVMs localized in functionally significant areas or deep structures are sent for irradiation. Patients with SM 4-5 AVMs are referred for radiation therapy or observation. In some cases, patients with SM 4 AVM can undergo removal of the malformation. AVM embolization can be considered as an independent method in a small group of patients with small compact AVMs that have one or more large afferents. For unruptured AVMs, management tactics are more conservative. If there are no or minimal clinical symptoms, observation is warranted. In the case of convexital AVMs SM 1-3 in young and middle-aged patients, “active” tactics are possible - embolization followed by removal or irradiation of the AVM. Radiation treatment can be recommended for patients with SM 1-3 AVMs localized in functionally significant areas. Patients with AVM SM 4-5 remain under dynamic observation. In elderly patients, observation is usually limited.
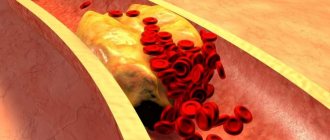
Complications of vascular malformation
Ignoring the symptoms of vascular malformation increases the likelihood of developing complications of the disease. Abnormal vessels can lead to insufficient blood supply to certain areas of the brain, causing hypoxia. Hypoxia, in turn, leads to degeneration and death of brain tissue. As a result, the clinical picture of ischemic stroke develops. Compression of surrounding tissues can lead to the development of hydrocephalus of the brain, persistent movement disorders, and severe neurological disorders.
A very serious consequence of malformations is cerebral hemorrhage. Depending on the volume of hemorrhage and its location, the result can vary from headache to death.
Principles of microsurgical removal of AVM
| AVM. View of operations |
Direct surgical interventions are preferably performed in the cold period after hemorrhage, since concomitant brain changes make it difficult to isolate the AVM, which leads to worsening brain injury and is more difficult for patients to tolerate. In the acute period of parenchymal hemorrhage, the tactic of removing large hematomas without attempting to excise the AVM is justified. An operation to simultaneously remove a hematoma and malformation can be performed for small lobar AVMs. It should be remembered that in the presence of a hematoma and cerebral edema, the contrast of the AVM may differ significantly from the true one due to compression of the vessels of the malformation. With deep AVMs, as well as with large AVMs, it is advisable to wait for the hematoma to resolve. In case of ventricular hemorrhage, installation of external ventricular drainage is indicated. Trephination should be performed in such a way that, in addition to the AVM node, it provides visualization of the afferent arteries and main drainage veins of the malformation throughout. When isolating the feeding vessels of the AVM, in order to reduce trauma to the medulla, it is important to use natural grooves and spaces (for example: wide preparation of the lateral fissure when isolating afferents coming from the middle cerebral artery; interhemispheric approaches to control afferents coming from the pericallosal or posterior cerebral arteries, etc.). P.). Switching off the afferent arteries must be done at a minimum distance from the AVM tangle. This is due to the fact that branches from the arteries feeding the AVM can extend to the brain parenchyma. This situation is especially relevant when excision of AVMs of deep and para-trunk localization, when branches supplying blood to functionally important structures may be damaged. To avoid injury to the AVM vessels, its isolation should be carried out as a single block along the perifocal zone. In patients after hemorrhage, one of the poles of the AVM tangle can be clearly demarcated from the brain by an intracerebral hematoma or post-hemorrhagic cyst, which simplifies surgical manipulations. It should be remembered that in some cases the hematoma can fragment the AVM, and therefore revision of the walls of the cavity of the removed AVM is mandatory. Transection of the main drainage veins should be performed after complete isolation of the AVM. The principle of gradual switching off of the arterial inflow as the tangle is released, and the venous inflow upon completion of AVM dissection, is well known. When venous drainage is reduced in conditions of continued arterial inflow, the AVM node becomes tense and bleeding. In certain cases, when there is an imbalance in blood flow, spontaneous ruptures of the thin vessels of the malformation occur, leading to intense bleeding that is extremely difficult to stop. The only way out in such a situation is the rapid isolation of the AVM with the afferents turned off. Since the walls of the malformation arteries, unlike normal vessels, have a thinned muscle layer, the vessels must be coagulated carefully and extensively. Significant intraoperative complications include air embolism. In the postoperative period, deterioration in neurological status was noted in 30% of patients, with a significant regression in the severity of symptoms in most cases. Postoperative mortality was 1.3%. Postoperative visual disorders are quite persistent and practically do not regress. With postoperative speech disorders, in the vast majority of cases, it is possible to achieve a significant regression of symptoms, and in many patients they will completely get rid of the speech defect.
Diagnostics
Diagnosis of vascular anomalies is carried out by a neurologist, who collects the patient’s complaints, examines the patient, assesses the neurological status and prescribes additional examination.
For diagnostics the following are used:
- Arteriography makes it possible to detect abnormal cerebral vessels. Catheterization of the femoral artery is performed, with the help of which a contrast agent is injected into the vessels of the brain. This will show the condition of the brain vessels and the presence of malformations.
- Computed tomography is also used with the introduction of contrast. Subsequently, the radiologist takes a series of images, which shows whether there are vascular malformations or not.
- MRI can be considered the gold standard in the diagnosis of vascular malformations of the brain. It shows the exact location of the malformation, its size and the presence of complications.
- Doppler ultrasound shows the position of the affected vessel and allows for differential diagnosis of this pathology with other vascular diseases.
Endovascular treatment of cerebral AVM
The main criterion for selecting patients for endovascular embolization is the presence of afferent vessels available for superselective catheterization. Until recently, AVM embolization was performed with histoacryl mixed with lipiodol. To date, AVM embolization in many patients has been performed with the Onyx composition. In fistula AVMs, occlusion of the afferent vessels is performed using microspirals. The volume of embolization and the number of stages depend on the angioarchitecture of the AVM. Total embolization can be achieved in 30% of patients. Subtotal AVM embolization was performed in 30% of patients. In 40% of patients, only partial embolization was achieved. Persistent neurological deficit after surgery was observed in 4% of cases, mortality was 1.3%.
| Turning off vein of Galen malformation |
AVM (aneurysm) of the vein of Galen is a special type of arteriovenous malformation, characteristic mainly of children. The pathology is congenital in nature and is characterized by the formation of an arteriovenous shunt in the area of one of the main venous collectors - the great vein of the brain. Aneurysms of the vein of Galen account for about 30% of malformations detected in childhood and are accompanied by high mortality (up to 90%). Treatment of the disease is carried out only by the endovascular method. The main goal is to stop or reduce the discharge of arterial blood into the venous system of the brain, which is achieved by occluding afferent vessels using transarterial access. To occlude the afferents of AVMs of the mural type, microspirals and balloon catheters are used; for the choroidal type, microspirals, adhesive compositions, or a combination thereof are used. Complete cessation of arterial inflow can be achieved with the mural type of malformation in 61% of cases, with choroidal type malformations - 7%. Both in the immediate and long-term periods after endovascular treatment, the overwhelming majority of observations obtained a positive result. The best results were observed in the group of patients under 1 year of age. Persistent neurological deficit developed in 5.6%, mortality was 2.8%. Spinal cord AVMs are rare and difficult to treat pathologies. AVMs and dural arteriovenous fistulas (DAVFs) of the spinal cord occur with a frequency of up to 3% in the population, accounting for about 20% of all vascular malformations of the central nervous system. The effectiveness of endovascular treatment of spinal AVMs is determined by the neurological status of patients after interventions: in our material, positive results (significant regression of neurological symptoms) were achieved in 91% of cases.
| AVM excision after embolization with Onyx composition |
Symptoms
Arteriovenous malformations can be asymptomatic for many years, or even a person’s entire life.
Often, they are discovered by chance, during the diagnosis of another disease of the body. If the malformation is small and does not progress, then the patient is unlikely to know about it. But if the abnormal vessel enlarges, it can compress the brain structures, which sooner or later will lead to neurological disorders. The symptoms of the disease are quite nonspecific, so the doctor must conduct a complete examination of the patient to make an accurate diagnosis.
Arteriovenous malformations can cause:
- intracranial hypertension with the development of pressing or throbbing headache;
- lethargy and apathy, which leads to a decrease in performance;
- movement coordination disorders, which leads to unsteady gait and sudden falls;
- speech disorders, in particular motor aphasia;
- disturbances of the innervation of certain parts of the body;
- decreased muscle tone and seizures;
- visual impairment, which may manifest itself as strabismus, loss of visual fields, partial or complete blindness;
- various epileptic seizures;
- paresis of the limbs
The severity and intensity of the clinical picture depend on the location of formation of vascular malformations.
Rupture of a vascular malformation entails the appearance of acute symptoms.
This complication is fraught with the development of internal bleeding in the brain or spinal cord and the development of ischemic disorders due to the sudden cessation of blood supply to certain brain structures.
Subarachnoid hemorrhage and the formation of intracranial hematoma manifests itself:
- a sharp and sudden attack of very severe headache;
- nausea and intense vomiting for no obvious reason, which does not bring relief;
- syncope;
- photophobia, ocular paresis and visual impairment;
- speech impairment;
- convulsive seizures;
- paralysis of the limbs.
Radiation treatment of brain AVM
| Leksell Gamma Knife |
Radiation therapy (gamma knife, proton beam irradiation) is most effective for small compact malformations with a diameter of no more than 3 cm. Thus, with malformations less than 1 cm in diameter, complete obliteration can be achieved in almost 90% of cases, and with malformations with a diameter of more than 3 cm only - up to 30%. The negative side of radiation therapy for AVM is that obliteration of the AVM vessels occurs 1–3 years after treatment. Recent studies have shown that pre-embolization of AVM reduces the effectiveness of radiosurgery. According to the Research Institute of Neurosurgery, after stereotactic irradiation, complete obliteration can be achieved in more than 70% of cases. In 10% of patients, a decrease in the size of the AVM and a reduction in blood flow is observed.