There are synonyms for a pathological autopsy - “necropsy”, “autopsy”, “section” and others. The autopsy is also divided into a pathological examination, necessary to confirm the conclusions previously made by doctors regarding the causes of death, and a forensic medical examination. The first is carried out in the general case and for a number of reasons it can be abandoned. For example, if the deceased was diagnosed with AIDS or one of the cancer diseases. Religious affiliation is considered as a reason if there is an outpatient card completed within the last six months.
An emergency medical examination is prescribed in emergency cases, when a body was found in a public place, there are suspicions of violence, or the death occurred under unclear circumstances. In the presence of such factors, it is impossible to refuse an autopsy.
Surgical treatment of wounds of soft tissues of the head
In the presence of wounds of the soft tissues of the head, the operation begins with the preparation of the surgical field. The hair around the wound is shaved. The wound is washed generously with a 3% hydrogen peroxide solution to remove small foreign bodies, hair, etc.
The edges of the wound are carefully treated with an antiseptic. The antiseptic solution should not get into the wound itself. The edges of the wound are then infiltrated with an antibiotic solution acceptable for endolumbar administration (penicillin sodium salt, kanamycin), based on 0.5% novocaine. This achieves both local anesthesia and prevention of wound infection.
The needle should be inserted near the edge of the wound through the skin, but not through the wound surface itself (Fig. 39).
Inserting a needle through the wound surface promotes infection deeper into undamaged tissue and provokes the development of suppuration in the postoperative period.
Rice. 39. Place of needle insertion during primary surgical treatment of soft tissue wounds of the head:
a – through intact tissue (correct); b – over the edge of the wound (incorrect)
Excision of the edges of the wound is carried out taking into account the location of the arterial trunks so that as little as possible gets into the incisions. Excision must be economical and performed in such a way that after suturing the wound, the underlying tissue (bone, dura mater) is necessarily covered with soft tissue. In cases where, due to extensive soft tissue defects or excessive excision during PSO, the bone remains uncovered, there is a danger of necrosis, infection and osteomyelitis of the bone. If it is still not possible to cover the exposed bone due to a lack of soft tissue, then proceed as follows. In the area of the bone that cannot be covered, the outer compact plate is removed to the diploic layer using a rotator equipped with a spear. It is desirable to form an almost continuous area from the removed outer plate. This creates conditions for the growth of granulation tissue and subsequent favorable engraftment of skin grafts. The rules for suturing wounds of soft tissues of the head are outlined at the end of the chapter.
Craniotomy technique
1. Make sure that the intervention side is chosen correctly.
2. Fix the head in the desired position for ease of access by placing a rubber or cotton-gauze ring under the head or by applying rigid fixation using a Mayfield-Kees bracket.
This creates reliability and minimizes the risk of endotracheal tube dislocation.
3. Correctly choose the physiological position of the patient on the operating table (most often this is the position on the back with a bolster under the shoulder and on the side). When lying on the side, to prevent positional compression of the axillary neurovascular formations, it is necessary to place a cushion under the chest, just below the armpit.
4. It is necessary to ensure that there is no possible contact between the patient’s body and metal parts of the table.
5. The head should be clean shaved and washed, preferably a few minutes before the operation.
6. Treat the surgical field with a large amount of antiseptic, according to the instructions for its use.
7. Select the correct type and location of the incision.
Active development
The period of particularly active development of neurosurgery occurred in the second half of the 18th century. Giovanni Morgagni appeared , which linked nosology and a specific pathological substrate. She completely changed the philosophy of all European medicine and justified the removal of tumors in the skull. The first neuro-oncosurgical operations were performed on tumors that destroyed the cranial vault. The explanation for this choice was simple: such neoplasms were diagnosed quite easily. But at the same time, mortality rates during such interventions were quite high. So, for example, in Paris, over the course of 6 years, all the patients who underwent trepanation died.
Craniotomy technique
Before covering the surgical field with linen, it is advisable to mark the incision line with a solution of brilliant green. The soft tissue incision is made horseshoe-shaped or linear vertical. In this case, the location and type of branching of the superficial temporal artery should be taken into account. Its intersection, especially with the main type of branching, can lead to necrosis of soft tissues in the intervention area. Therefore, before marking the proposed incision, the superficial temporal artery should be palpated. Stepping 2–3 cm away from it to the left or right, mark the cut line. With a horseshoe incision, the artery should be located in the center of the intended aponeurotic skin flap.
Does it make sense to infiltrate soft tissues with a physiological solution along the incision? Infiltration of soft tissues with saline solution for the purpose of “hydropreparation” or hemostasis gives practically nothing. If the surgeon traditionally prefers infiltration for the purpose of hemostasis, then the most effective is the use of 10 - 20 ml of 2% novocaine with the addition of adrenaline (in the absence of contraindications for its use). Adrenaline causes a spasm of the arteries in the incision area for about 2 hours.
The shape of the incision depends on the planned access and can be either linear or horseshoe-shaped (Fig. 40).
Preference should be given to horseshoe-shaped skin incisions with a wide base of the feeding pedicle. This ensures a large area for trephination and the absence of a retractor in the wound. To achieve the best cosmetic effect, it is possible to perform wavy incisions.
Rice. 40. Basic forms of incisions in the soft tissues of the head:
a – horseshoe-shaped; b – linear
For better hemostasis during the incision, the fingers of the surgeon and assistant, positioned perpendicular to the wound, should press the skin tightly to the bone. The length of the “step” when cutting should not exceed the width of 4 fingers across. When cutting the skin, the aponeurosis should also be cut immediately. This makes it possible to separate the edges of the wound with a napkin applied from the inside with finger compression of the edges. It is better to start applying hemostatic clamps from the “assistant” side.
The correct technique for applying hemostatic clamps to the edges of a skin wound is important. Clamps should be applied to the aponeurosis, without immersing the jaws to the full depth and capturing the subcutaneous fatty tissue (Fig. 41). A 3–5 mm grasp of the aponeurosis is sufficient. Applying a clamp to the entire thickness of the separated flap (including the skin) leads to flattening of the soft tissues and their necrosis in the postoperative period. It should not be a homemade effort to apply clamps in all places where bleeding arteries are visible, although it is advisable to apply them in this particular place. Clamps are applied approximately 1.5–2 cm apart, depending on the degree of blood supply to the incised area. On soft tissues, when the clamps are tilted to the sides, the aponeurosis is stretched and bent over the skin edge, which ensures good hemostasis along the entire incision line (Fig. 42). The resulting wound should be packed with a dry cloth.
Rice. 41. Technique for applying a clamp to the aponeurosis:
a – correct: 1 – aponeurosis; b – incorrect (according to Yu. V. Kushel, V. E. Semin, 1998)
After the formation of the aponeurotic skin flap, it should be turned towards the base, and be sure to place a roll of napkins under it. This achieves greater hemostasis and prevention of circulatory disorders in the flap due to a sharp bend in the area of the feeding pedicle.
If it is initially planned to perform resection craniotomy , the periosteum is dissected parallel to the edge of the skin incision (1 cm away from it) with a horseshoe-shaped incision and linearly along the center of the wound - with linear access. After this, it is peeled off with a rasp either to the base or to the sides. After selecting the location of the burr hole using a rotary tool equipped with a spear, drilling of the bone begins with measured force to avoid falling into the cranial cavity.
Rice. 42. The principle of operation of a hemostatic clamp on the soft tissues of the head (according to Yu. V. Kushel, V. E. Semin, 1998)
Drilling continues until the internal vitreous plate and its partial opening. Subsequently, the remnants of the lamina vitrea in the projection of the hole are removed using a Volkmann spoon. Changing the spear to the cutter should take place above the operating nurse's table to avoid its accidental fall to the floor. It is advisable to have two sterile rotators at the ready. Using a conical or ball cutter, the milling hole is drilled to the required size. In this case, it is allowed to perform angular rocking movements while drilling the bone to increase the size of the hole.
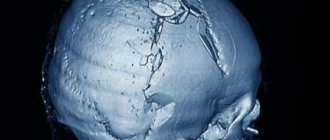
The formation of a trepanation window during the resection method is performed with bone cutters. It is important to remember that it is necessary to bite down the bone, and not to break it off with pliers from the mainland areas. Failure to comply with this rule can lead to unwanted breakouts of large bone fragments with concomitant fractures of the bones of the cranial vault, as well as damage to the underlying structures. The edges of the formed trepanation window should be as round as possible, without sharp protrusions and scalloped edges. These sharp protrusions, both during surgery and in the postoperative period, when the brain protrudes into the trepanation window, can injure the brain substance and cortical vessels. This leads to additional neuronal death and bleeding, which may require additional or repeat surgery.
The dimensions of the burr hole must be sufficient for a complete revision of intracranial formations or removal of the pathological focus. A common mistake is the desire of surgeons to perform a revision from a small burr hole (2x3 cm). An attempt to inspect not only the basal, but also the convexital sections from such a window leads to additional brain injury. A small burr hole with unsutured dura mater and bulging of the brain in the postoperative period leads to entrapment of the brain in the bone hole. This compresses the cortical vessels, primarily the venous ones, which leads to venous stagnation, hypoxia and even greater swelling of the prolapsed area of the brain. Further increase in infringement causes compression of the arterial vessels with the subsequent development of infarction of the brain area.
An excessively large trepanation window is also undesirable. An increase in the bone defect leads to an increase in the area of formation of postoperative scars and adhesions, the risk of developing “trepanned skull” disease, and post-traumatic epilepsy. Depending on the size and location of the pathological traumatic focus, the trepanation window should be no less than 6 x 7 x 8 cm.
It is very important to choose the correct location for the burr hole. When performing a computed tomography scan, the surgeon has the opportunity to assess the type and location of the traumatic focus and, in accordance with this, plan the location of the burr hole and the extent of the intervention. Doctors in non-specialized hospitals do not have this opportunity and must take into account that with TBI, the basal and inferior convexital parts of the brain (the poles of the frontal and temporal lobes) are most often affected. This dictates the requirement to place the burr hole as low as possible to the base of the skull. In this case, the “side” of the temporal bone at the lower edge of the trepanation window should be as small as possible. This allows for an inspection of the basal parts of the skull and brain and, if necessary, removal of the pathological focus with minimal trauma to the brain. Hemostasis from diploic vessels is achieved by using soft wax.
Osteoplastic trephination (OBT) of the skull is carried out in the traditional way by applying several burr holes and connecting them with a Gigli saw or from one hole using a craniotome. The surgeon should be especially careful when passing the saw guide under the bone to avoid damage to the dura mater and penetration of the instrument into the brain.
At the present stage, preference should be given to the free bone flap technique, in which the periosteum is less injured and the bone flap does not interfere with the work (since it is removed from the wound during the main stage of the operation). Leading foreign neurosurgeons (M. G. Yasargil, J. M. Tew, N. R. van Loveren and many others) consider the formation of a free bone flap with a craniotome from one burr hole to be the gold standard. The declared risk of developing osteomyelitis and poor fusion in the future does not have sufficient grounds. References to the feeding periosteal pedicle and the need to preserve it are not supported by morphological data, which indicate that about 80% of the blood supply to the bone occurs through the dura mater.
A comment
The fairly high incidence of hemorrhages due to rupture of intracranial aneurysms, accompanied by a very high level of adverse outcomes, determines the constant optimization and development of new approaches to treatment tactics in these patients. The review presented by the authors is devoted to a very narrow section of the surgical treatment of patients with intracranial hemorrhages due to rupture of aneurysms - the need for decompressive trepanation. Despite the obvious importance of solving the problem of intracranial hypertension, edema and dislocation of the brain, decompressive trepanation in this group of patients has not become as widespread as in patients with traumatic brain injury. Moreover, the number of works published on this topic over the past two decades is very small. A critical analysis of all available literature concerning this aspect of surgical treatment allowed the authors to determine the indications, timing and features of the operation, as well as evaluate the results of treatment and identify risk factors for adverse outcomes. It is obvious that the work performed by the authors can be the basis for conducting a prospective study aimed at clarifying the effectiveness of decompressive craniectomy in patients with intracranial hemorrhages due to ruptured aneurysms. This review will be extremely useful for neurosurgeons, resuscitators, and neurologists treating patients with intracranial aneurysms.
A.G. Gavrilov (Moscow)