If a person has increased intracranial pressure (ICP), attention is not always immediately paid to the syndrome, because it often occurs with mild symptoms. The pathology can develop both in childhood and in adulthood; it is more often diagnosed in women.
To protect yourself and start treatment on time, you need to know the symptoms of intracranial pressure to prevent the sad consequences of advanced forms of the disease. Next, we will talk about the essence of the diagnosis, the reasons that provoke indicators of intracranial pressure, symptoms, methods of diagnosis and treatment.
How does intracranial pressure increase?
An increase in pressure inside the skull can be caused by various reasons, of which there are many, but most often doctors diagnose a deterioration in the outflow of liquor fluid from the cavity of the cranium. If some people believe that there is nothing in the skull except the brain and the nerve cells that fill it, this opinion is wrong. In an adult, just like in a child, 1/10 of the brain is occupied by cerebrospinal fluid; it is located in its central part in special chambers (ventricles).
Another part of the cerebrospinal fluid constantly moves in microscopic spaces, reminiscent of arachnoid formations, present in the spaces between the membranes of the brain and spinal cord. Liquor performs many functions - it protects the skull and brain structures from blows and injuries, cleanses the body of harmful decay products and toxins, and stabilizes ICP. Complete renewal of cerebrospinal fluid occurs within 7 days, two-thirds of it is formed in the cerebral ventricles, and another part is formed from the blood supplying the brain tissue.
Normal intracranial pressure for an adult is 3–15 mmHg. Art., in children and adolescents the indicators are lower - 2–5 and 3–7 mm Hg. Art. respectively. High intracranial pressure, when the readings increase to 30 mmHg. Art., is considered dangerous to human health and life, since it threatens irreversible damage to brain neurons and death.
Treatment options
Treatment tactics are structured as follows: eliminating the root cause of the disease, accelerating the natural outflow of cerebrospinal fluid, relieving symptoms. If hypertension is a temporary complication of any other disease, manual therapy is prescribed to help restore normal blood circulation. At the same time, the drinking regime is regulated and a set of exercises is prescribed to relieve pressure inside the head.
More complex anomalies require a course of medications aimed at accelerating the absorption of fluid and its removal to the outside. The basis of drug therapy is diuretics. In some cases, long-term or permanent (lifelong) use of such drugs is required.
In critical cases, when the disease poses a direct threat to life, surgical treatment is performed. If there is a tumor blocking the outflow of cerebrospinal fluid, the possibility of its removal is considered. To urgently reduce pressure, shunts are inserted into the skull to drain excess fluid.
Causes of the disease
It should be clarified that signs of ICP do not arise just like that; pathology always accompanies any diseases and abnormalities in the functioning of the body. Symptoms of the disease begin to appear due to the following reasons:
- congenital abnormal structure of capillaries and brain structures;
- obesity due to hypertension;
- diseases of the endocrine system;
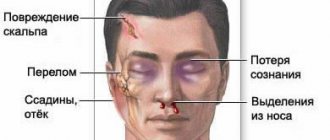
- traumatic brain and birth injuries;
- infectious diseases - meningitis, mastoiditis, malaria, complications of otitis media and pneumonia;
- neoplasms, cysts and abscesses in the cranial cavity;
- osteochondrosis of the cervical spine;
- use of certain groups of medications - corticosteroids, tetracycline and sulfonamide antibiotics, oral contraceptives in women).
We must not forget about hereditary predisposition to the disease. If several relatives in the direct line suffered from signs of intracranial pressure, they can definitely appear in the heirs.
In children, cranial pressure increases as a result of an unfavorable course of pregnancy in the mother (if there was brain hypoxia in the fetus, asphyxia, damage by toxic substances). You can also develop the disease during a cesarean section or when pulling the baby out of the birth canal with forceps. All these factors contribute to increased production of cerebrospinal fluid and the development of hypertensive-hydrocephalic syndrome.
Symptoms
The basis of the clinical picture of intracranial hypertension is headache, pressing on the eyes. In an acute course, its intensity quickly increases; in a chronic process, unpleasant symptoms are not so pronounced, pain occurs periodically.
Patients also complain of nausea, which with severe pain can turn into vomiting, and discomfort when moving the eyes. Acutely increasing intracranial hypertension can lead to loss of consciousness and even coma.
In a chronic course, the general condition of a person suffers. Sleep is disturbed and irritability appears. Patients note fatigue and weather dependence. They periodically experience liquor-hypertensive crises, characterized by intense headaches, nausea, vomiting and even loss of consciousness.
Idiopathic intracranial hypertension most often causes transient visual disturbances (double vision, blurring, decreased sharpness).
In children whose intracranial pressure increases, their behavior changes. They become restless, whiny, often burp and refuse to eat. One of the specific symptoms is bulging fontanel. The chronic course of the pathology can lead to mental retardation, even mental retardation.
Characteristic symptoms
How to understand that a person has increased cranial pressure, what signs may indicate a problem? There is no special device that will allow you to check the level of intracranial pressure, but you should pay attention even at the initial stage of the disease to the following symptoms:
Signs of a hypertensive crisis
- Headaches, especially disturbing at night and in the morning; this symptom sometimes helps to recognize increased pressure inside the skull. They vary in nature, from dull, aching and not expressed, to intense, accompanied by pain in the eyeballs and the inability to turn the eyes in the other direction.
- Deterioration of vision. At the initial stage of ICP, a person notices the flickering of “spots” before the eyes, double objects and blurred pictures; the symptoms either appear or go away on their own. As the disease worsens, the changes become permanent and pronounced.
- Dizziness, fainting. They are accompanied by severe headaches and occur in response to weather changes, after physical exertion or stress. In severe cases, fainting occurs with convulsions.
- Attacks of nausea. They appear not only after eating, but often in the morning, when a person has not even had time to have breakfast. It is noteworthy that nausea and vomiting occur during the next attack of headache, at its very peak.
- Irritability, nervousness, frequent mood swings, tendency to apathy and depression.
- Signs of vegetative-vascular dystonia are increased fatigue, weakness, sweating, chronic fatigue, sleep disturbances, rapid heartbeat.
In severe forms of the disease, the patient may experience generalized seizures with muscle paresis, respiratory depression and the risk of developing cerebral edema. That is why, if the listed signs of increased intracranial pressure appear, you should not delay your visit to the hospital, but immediately begin an examination.
In children, you can learn about the development of pathology by the following clinical symptoms:
- moodiness, lethargy, poor sleep with frequent awakenings;
- bulging of a large fontanel, covering the scalp with a pronounced network of blood vessels;
- protrusion of the eyes, due to which the pupils are visible between the eyelids during sleep;
- increase in head volume - in advanced forms of the disease, the skull can increase 2-3 times more than normal;
- frequent regurgitation, up to 3–4 times a day;
- deterioration in health when the child lies in a crib in a horizontal position - this causes the cerebrospinal fluid to flow from the cranial cavity even worse, and signs of high ICP develop.
Increased intracranial pressure is usually recorded simultaneously with neurological disorders in a child - nosebleeds, stuttering, a trembling chin while crying, blue discoloration of the nasolabial triangle. However, such signs may not indicate high blood pressure, but occur in isolation against the background of perinatal encephalopathy.
Monitoring the effectiveness of treatment
After surgical treatment, it is important for doctors to assess the state of the central nervous system and determine the likelihood of relapse. To monitor the quality of treatment, hardware diagnostics - MRI - are also used. It is absolutely safe to carry out such screening several times in a row, since during the examination the body is not exposed to x-ray radiation. The magnetic fields produced by the MR installation do not have a destructive effect on the body.
The scan can be performed in any medical institution that has the necessary technical facilities and trained functional radiologists. In Moscow, hundreds of diagnostic centers located in every district of the city receive services. To quickly find the nearest MRI medical facility, you can use a single city service.
When you click on the link, a search page will open where you can select a diagnostic service and the area where the clinic is located. In response to the request, a complete list of medical institutions will appear, distributed by rating and prices for procedures. Study the information, read reviews, mark the best offers. To make an appointment for a tomography, just call the phone number listed on each page of the site. All service guests who have booked a scanning time through the portal receive a guaranteed discount of 1,000 rubles on any type of diagnosis.
Diagnostics
What should you do if an adult or child shows signs of increased ICP, especially on a regular basis? Seek advice from a neurologist and undergo the necessary examination. In severe cases of the disease, rather dangerous and complex techniques are used, for example, puncture of the cerebral ventricles and insertion of catheters into the sites of cerebrospinal fluid circulation.
A puncture of liquor fluid from the spinal vertebral region is also performed. This measure is necessary if an acute or latent neuroinfection is suspected. Examination methods require appropriate equipment, completely sterile conditions and highly qualified specialists, so they are not used so often. What causes high intracranial pressure is now clear, but how else can a correct diagnosis be made?
There are simpler and safer research methods for this:
- Ultrasound of cerebral vessels;
- Magnetic resonance imaging;
- CT scan;
- neurosonography (NSG);
- examination of the fundus by an ophthalmologist.
During an ultrasound examination, the attending physician is able to determine approximate indicators of intracranial pressure and evaluate the structures of the brain for congenital abnormal structure. MRI and CT scans provide information about the presence of changes in the cavities of the brain containing cerebrospinal fluid - whether they were damaged or ruptured during traumatic brain injuries. A fundus examination is indicated for all patients with suspected high ICP - it shows changes in the size of the capillaries of the apples, small hemorrhages on the surface of the retina, and vascular spasms.
General information
Increased intracranial pressure is a condition in which intracranial pressure is increased to 20–25 mmHg. Art. and more in the sinus cavity of the structure of the dura mater of the brain, ventricles, epidural, subarachnoid space and, in general, the skull. Also called intracranial hypertension .
The pathology causes intracranial syndrome with a number of clinical manifestations - increasing headache, nausea, vomiting, clouding of consciousness , etc.
Possible complications
If measures are not taken in time and the blood pressure level is not normalized, as the disease progresses, the symptoms will only worsen, causing serious complications. These include:
- damage to the cerebellum with partial or complete loss of coordination in space;
- disorders of speech and mental functions;
- arrhythmia, tachycardia, surges in blood pressure due to compression of the brain stem;
- loss of vision;
- the appearance of epileptic convulsive seizures, during which the patient’s breathing is depressed, the risk of cerebral edema and transition to a coma increases;
- paralysis.
Now it has become clear why intracranial pressure that is not subject to adequate treatment is dangerous. The benign form of intracranial hypertension occurs much more easily and without dangerous consequences; it is more often observed in women aged 20–40 years, taking oral contraceptives and being obese. The disease manifests itself as unsteadiness of gait, dizziness, morning sickness and signs of migraine.
When hormonal medications are discontinued and lifestyle is adjusted, it happens that the symptoms of the pathology may go away on their own. But it’s better not to hope that in a particular case the problem is caused by a benign form of hypertension; it’s worth starting to fight it right away.
Lumbar puncture
If hardware diagnostics do not help identify the cause of the disease, the neurologist prescribes a lumbar puncture - a lumbar puncture. It is an invasive procedure performed to obtain a sample of cerebrospinal fluid. The procedure can be performed for diagnostic and therapeutic purposes. During diagnosis, a lumbar puncture helps to more accurately determine the degree of pressure increase. For therapeutic purposes, the procedure is performed for benign intracranial hypertension to improve the patient’s condition.
Treatment
In the case of a secondary process in adults, the culprit of the disease may be atherosclerotic changes in blood vessels, obesity, hypertension, and hormonal dysfunction. It is important not only to cure the primary disease, but also to eliminate the symptoms of ICP. For this purpose medications are used:
- diuretics – Furosemide, Veroshpiron, Torasemide;
- nootropic drugs - Pantocalcin, Piracetam, Pantogam, Tanakan, they improve the supply of oxygen to the brain and the transfer of nutrients to it;
- sedatives - valerian extract, peony and motherwort tinctures, Novo-passit, Persen forte;
- stimulators of nerve cells in the brain - Glycine, Nervohel, they also improve sleep, memory, concentration and attention;
- vitamin complexes, as well as a course of injections of B vitamins to restore normal functions of the nervous system.
Treatment of intracranial pressure begins with proper diagnosis and clarification of the cause of the pathology.
If there is a need for additional medications, the doctor makes a prescription, and the patient must strictly follow the instructions and complete the full course of treatment. In addition to medications, physical therapy and physiotherapy (SMT, electrophoresis, magnetic therapy) help to remove signs of ICP. General massage, ozokerite applications, acupuncture and hirudotherapy work well to combat symptoms.
The patient also needs to adjust their lifestyle:
- get proper rest and sleep at least 8 hours a day;
- follow a diet with limited salt to eliminate fluid retention in the body;
- drink no more than 1.5 liters of water per day;
- eat a balanced diet, focusing on meat, fish products, vegetables, fruits, and grains;
- spend more time in the fresh air;
- protect yourself from stressful and conflict situations.
Moderate physical activity is the path to recovery from ICP.
Such measures will help prevent the progression of the disease and prevent the dangerous complications described above. If symptoms of ICP appear regularly, courses of treatment should be taken at least once every 6 months.
Increased intracranial pressure is not a death sentence. If you detect the disease in time, follow the doctor’s recommendations and change your lifestyle, you can successfully get rid of the acute signs of the disease within 6–12 months. People with diabetes mellitus, autoimmune pathologies, traumatic brain injuries and signs of arterial hypertension need to pay special attention to their health.
How it manifests itself
The main symptoms of ICH in adult patients are headaches of moderate or severe intensity. Symptoms most often appear in the morning, since while in a horizontal position, the outflow of cerebrospinal fluid from the skull is even more difficult. The pain is dull, aching in nature, intensifies during coughing, physical activity, and is accompanied by a feeling of pressure on the eyeballs.
If cranial hypertension is moderate, there may simply be a feeling of heaviness in the head. Also, headaches are accompanied by attacks of nausea, which do not depend on the time of eating. The urge to vomit is observed during exacerbations of pain in the head, especially in the morning, after waking up, then they occur on an empty stomach. Sometimes the amount of vomit is quite copious, after which the person feels relief.
Further, in the absence of treatment, vision problems occur due to constant tension in the fundus of the eye and spasm of the vessels located there. At first, a person notices a distortion of the picture, a lack of clarity. Vision is blurred, objects in the eyes may appear double, but such phenomena pass on their own. As the disease progresses, such symptoms appear more and more often, and movements of the eyeballs in any direction bring pain.
Indirect signs of intracranial hypertension in adults are changes in well-being as a reaction to weather conditions, irritability, and a decline in the physical and emotional capabilities of the body. A person’s mood often changes, he becomes whiny, hypersensitive, sleeps poorly and feels unwell during rain and thunderstorms.
Moderate hypertension is also manifested by dysfunction of the autonomic parts of the nervous system - increased sweating, increased heart rate, and surges in blood pressure. The pronounced picture of the disease occurs against the background of constant intense pain in the head and nausea that accompany the listed symptoms.
How dangerous is intracranial hypertension if you do not pay attention to its symptoms and do not start timely therapy? The patient develops daily attacks of morning vomiting and severe headaches. If pain is accompanied by hiccups, this sign indicates the presence of a neoplasm in the posterior cranial fossa.
As the pathology progresses, signs of depression of mental functions increase - the patient becomes inhibited, his consciousness is impaired until he completely falls into a coma. There are regular surges in blood pressure with a decrease in breathing, while the heart rate drops to 50–60 times per minute. In advanced cases, generalized convulsive syndrome appears.
Symptoms in children
If the damage to the ventricles of the brain is mild, symptoms may be mild. But a neurologist must notice it at the first appointment at the clinic, at the age of 1 month. Later, parents themselves note some signs of ICH in their baby:
- enlargement of the head and protrusion of the eyeballs - with a severe degree of the disease, the skull grows in volume several times, and the eyelids cannot completely close during sleep, the pupils are visible between them;
- pulsation in the area of the large fontanel and a pronounced venous network on the surface of the scalp;
- regurgitation up to 3-4 times a day, occurring due to injury to the nerve receptors responsible for the functions of the gastrointestinal tract;
- poor sleep, frequent awakenings, deterioration of health when lying on your back - this is explained by a deterioration in the outflow of cerebrospinal fluid and the appearance of severe headaches;
- walking on tiptoes;
- lag in psychophysical development - in comparison with peers, the child later begins to stand on his feet, crawl, sit, roll over from back to stomach, and talk.
Children of kindergarten and school age often complain of headaches, and have attacks of nausea and vomiting even in the absence of food intake. Academic performance deteriorates, the child cannot concentrate on simple tasks, attention and concentration are reduced. Speech functions also remain not fully developed - children with intracranial hypertension syndrome often need the help of a speech therapist, they burr, mix up words, and “chew” endings.
In adolescents, the symptoms are more pronounced compared to schoolchildren - fainting occurs due to increased weather sensitivity and headaches. Regular changes in blood pressure appear. Teenagers become prone to depression, which is why there are frequent scandals with parents and peers. They need help from psychologists.
Reviews
Larisa, 36 years old: My son was diagnosed with increased intracranial pressure at the age of 14. Before this, he had not made any special complaints, except for headaches, but I thought that this was an age-related problem and would go away on its own. After the examination, the doctor prescribed a course of general massage, Furosemide, Cavinton and Pantogam tablets. After just two weeks, my son began to feel better; in a year he needs to take another course.
Svetlana, 46 years old: My intracranial pressure increased after severe stress when my husband got sick. I had a severe headache, blood vessels in my eyeballs burst, and one eye hurt unbearably. The neurologist prescribed me Actovegin injections, Veroshpiron tablets and physiotherapy - electrophoresis with magnesia. After a week I felt better and didn’t go to the doctor again. But now, in every situation when I worry, I feel the familiar pain in my head. Apparently, one course was not enough, I am going to see a neurologist again.
Anton, 24 years old: I have been boxing since I was a teenager, and in another fight I received a severe head injury. After an MRI, I was diagnosed with increased ICP. I take pills, go for massages and swimming, try to rest more and not be nervous, because I want to return to sports again. So far the doctor says that the injury was severe and another 2-3 courses of treatment are needed every three months. I hope that ICP is not a death sentence and I can make a full recovery.
Benign form of pathology
Benign intracranial hypertension is a separate form of the disease that occurs with the mildest manifestations, without symptoms of damage to the nervous system. It is also called idiopathic or false brain tumor. Women who are young and obese most often suffer from the pathology. The main symptoms are the urge to vomit, unsteadiness of gait, pain in the head and eyes. Why such a syndrome is formed is still not completely clear to doctors.
Initially, headaches are mild, which is why people do not seek medical help, especially since attacks are quickly eliminated after taking analgesic tablets. Then the problem becomes constant, accompanied by nausea and vomiting. Vision problems appear, in women the regularity of the menstrual cycle is disrupted, in men - weakening libido.
As a rule, there are no signs of damage to the nervous system, and in the initial stages the disease goes away on its own without treatment. Doctors have identified a connection between the development of symptoms in women and the use of oral contraceptives, after which the pathology disappears without a trace. If the clinical picture is pronounced, the same drugs are used in conservative treatment as in the treatment of the usual form of intracranial hypertension.
Pathogenesis
Normally, intracranial pressure readings should not exceed 7–15 mmHg. Art. in a lying position. They are provided:
- a rigid frame of the skull and dura maters, which gives constancy of the volume as a whole and the sum of the individual volumes of elements and structures;
- complex processes of physiological regulation - cerebral perfusion pressure, cerebral vascular tone, volumetric blood circulation in the brain, production and resorption of cerebrospinal fluid, permeability of the blood-brain barrier and colloid-osmotic stasis of brain fluid.
When one of the listed factors, the dislocation of the brain, changes or is disrupted, a compensatory reaction should be automatically activated, which is aimed at displacing venous arterial and blood from the sinuses and, accordingly, the arteries, reducing the volume of cerebrospinal fluid by displacing it from the ventricles and reducing the volume of the brain by reducing the amount intercellular fluid.
For example, due to an increase in arterial blood pressure , the blood vessels in the brain rapidly constrict, causing blood flow in the brain and intracranial pressure to undergo significant changes.
The mechanism of intracranial hypertension is most often based on an increase in the volume of intracranial contents (due to impaired outflow or hyperproduction), including cerebrospinal fluid ( CSF ), tissue fluid ( with cerebral edema ), blood (may be caused by venous stagnation ), as well as the appearance of foreign tissue , for example, during oncological processes of tumor . The latter have not only a direct effect of mass, but also a direct blocking of the flow of cerebrospinal fluid. In addition, pathological changes in the brain that increase blood pressure occur as a result of processes such as:
- extravasation caused by cytokines (vasogenic edema);
- cytotoxic damage leading to cell death and necrosis (increased interstitial pressure);
- restorative and inflammatory processes initiated by cells of the inflammatory infiltrate in the cerebrospinal fluid during meningitis, ventriculitis , etc.;
- obstruction associated with congenital defects, excessive growth of dural tissue, impaired venous outflow, formation of a parenchymal or intraventricular mass of a cyst or neoplasm;
- increase in intravascular volume;
- hypoxemia;
- changes in partial pressure of carbon dioxide ( hypercapnia or hypocapnia );
- the effects of metabolic intermediate metabolic toxins , including neuronal excitotoxins ;
- depletion of energy substrates, for example, with blockage of great vessels, contusion or diffuse axonal damage, anoxia caused by cardiac arrest , hypertensive encephalopathy , encephalitis infection , metabolic poisoning.
Consequences and complications
- The emergence of areas of distension and the development of dislocation syndromes (disruption of higher nervous activity, respiratory centers, blood circulation, mental processes, consciousness, oculomotor functions, the occurrence of convulsions, anabolic disorders, etc.).
- Transtentorial wedging of the hook into the temporal lobes, entrapment of the oculomotor nerve and loss of the papillary reflex.
- Brain stem damage.
- Heart attack.
- Additional secondary edema.
- Brain death.
Facts and myths about increased intracranial pressure
There are several misconceptions about intracranial hypertension:
- It does not need to be treated; the condition will go away on its own with age. In fact, both children and adults need treatment to avoid serious complications.
- The condition cannot be treated. False: Treatment results depend on the cause and severity of hypertension. Even if it cannot be completely cured, therapy greatly improves the condition and reduces the risk of health consequences.
- High intracranial pressure always causes developmental delays in children. This is a myth: with timely treatment, such consequences can be avoided.
It is important to know that:
- High intracranial pressure in children most often occurs due to hydrocephalus and birth injuries.
- Homeopathic or herbal preparations do not affect blood pressure in any way and do not help normalize it.
- If a person already has intracranial hypertension, he needs to be examined by a neurologist at least once every two years.
What are the risks of increased intracranial pressure? Complications and consequences
The brain is the highest energy system in the human body. It needs approximately five times more oxygen than the heart. Therefore, the quality of blood supply to the brain is a vital indicator that depends on two parameters - blood pressure and intracranial pressure. At constant blood pressure, the lower the intracranial pressure, the better the blood supply to the brain. If for some reason intracranial pressure increases, this proportionally worsens the blood supply to the brain, and ischemia develops. Therefore, high intracranial pressure is a dangerous condition that can cause the following complications:
- reduction and complete loss of vision;
- convulsions;
- acute cerebrovascular accident;
- depression and/or disorder of consciousness;
- depression of respiratory and circulatory function.
Important! With a rapid increase in intracranial pressure, there is a threat of death. If the symptoms are severe or appear sharply, suddenly and rapidly increase, you need to call an ambulance.
Prognosis and prevention
When driving at high speed, wearing a helmet is mandatory.
Photo: Paha_L / Depositphotos Increased intracranial pressure is most often associated with head injuries. To prevent them, you need to take precautions: wear a seat belt in a car, use a helmet when riding a bicycle, and reduce the risk of falls.
If there are signs of hypertension, you should see a doctor as soon as possible. The earlier treatment is started, the lower the risk of serious health consequences.
In children
Intracranial pressure can be measured in cmH2O (centimeters of water). Normal indicators for childhood and infancy are approximately 6 cm H2O (do not exceed 5 mm Hg, for adolescents over 25-52 cm H2O (corresponds to 18-40 mm Hg), this is considered abnormal and provokes symptoms, with possible preservation of normal cognitive functioning with adequate perfusion pressure. In this case, it is not the absolute indicator of intracranial pressure that is indicative, but relative data in relation to mean arterial pressure. The clinical picture can be ominous and is usually caused by abnormal perfusion pressure at 52-78 cmH2O (up to 60 mmHg) to lower mean arterial pressure. It is caused by reduced perfusion and the development of swollen damaged tissue, an increase in the volume of parenchymal brain tissue, as a result of which the condition is aggravated by increased pressure due to increased volume, as well as the Cushing reflex (in hypertension against the background of bradycardia and bradypnea ).
Treatment of children with encephalopathies usually takes place in intensive care. craniotomy may be necessary . Treatment tactics are selected based on the size and location of the damage, deformation of brain tissue, and the likelihood of stopping perfusion.
Increased intracranial pressure in a child
It is very important to promptly pay attention and help when the child shows the first signs of intracranial increased pressure. Children experience more severe cerebral edema with a variety of head injuries, which is caused by a combination of cytotoxic and vasogenic edema. Children with the blue type of heart defect may develop an abscess; with sickle cell disease, a stroke , which also leads to increased pressure in the intracranial box.
Problems in teenage girls can be identified with increased body weight and cerebral circulation disorders, for example, hypertension can be caused by venous sinus thrombosis . Presumably, the mechanism of development may be based on a decrease in the level of corticosteroids in the bloodstream and an increase in the concentration of estrogen .
Changes in intracranial pressure in children most often develop as a result of hemorrhagic diathesis or complicated otitis media , mastoiditis , taking overdoses of vitamin A , tetracyclines closed head injury, as well as in case of refusal of steroid therapy.
Increased intracranial pressure in infants
In children, disturbances in intracranial pressure can occur with ischemic brain damage caused by difficulties during childbirth, as well as with drowning or thrombosis of blood vessels in the brain.
In infants and newborns, the following are considered suspicious signs:
- increase in head circumference;
- hypertension;
- protrusion and elevated location of the fontanelle;
- lack of retraction and ability to raise the eyes, probably caused by pressure in the midbrain;
- hyperreflexia due to hydrocephalus.
First aid
How to lower intracranial pressure?
Very often it is not possible to establish the cause of intracranial hypertension; its manifestations - headaches, vomiting - bother patients mostly in the mornings and nights, causing insomnia and dizziness , and reduce the ability for mental and physical activity. Therefore, many people try to lower their blood pressure on their own, at home, but, unfortunately, they can make mistakes, which only worsen the condition.
Typically, the problem of intracranial pressure worries people after 45 years of age who have problems with weight and hormonal systems. Eliminating the causes is quite difficult, so treatment in adults can become exclusively syndromic.
Primary treatment before the arrival of an ambulance in a serious condition (unstoppable vomiting, clouding of consciousness, convulsions) can begin with the application of a compress of camphor and ethyl alcohol in a 1:1 ratio. It is enough to apply the mixture on your head, wrap it in plastic, for example, put on a shower cap and lie down for a couple of hours.
The situation is more complicated with young children, whose crying can also quite often be caused by intracranial hypertension. Parents need to be alert and not try to lower intracranial pressure at home, but consult a doctor. The easiest way to alleviate the condition is a light 10-15-minute relaxing massage of the head, back and neck, and calmly bending forward.
The first thing to remember is that you cannot tolerate a headache; high blood pressure is one of its possible causes; to complete the picture, you should regularly visit a qualified neurologist and consult a family doctor.