Cysts of the choroid plexus of the brain in the fetus are detected in less than 1% of cases. The possibility of their detection usually occurs between the 16th and 20th week of intrauterine development. As a rule, most of these tumors regress on their own in the third trimester of pregnancy (closer to 28 weeks).
A choroid plexus cyst can be identified during fetal development and usually disappears by the time of birth.
Characteristics
The formation is an isolated cavity filled with clear liquid.
Structure Features:
- They are small in size and tend to dissolve on their own.
- More often they are localized closer to the caudal part of the choroidal glomus.
- It has clear, even contours.
- Does not show any upward trend.
- The presence of signs of malignancy is not typical. Due to the location, it should be differentiated from choroid carcinoma and choroid papilloma.
- There are no clinically significant symptoms. The exception is the development of occlusive hydrocephalus (disruption of the normal outflow of cerebrospinal fluid and its accumulation in the head). It is extremely rare.
- It is regarded as a stigma of dysembryogenesis (developmental defect). These newborns are at high risk of having chromosomal abnormalities (trisomy 18 - Edwards syndrome).
- The main diagnostic method is ultrasound. Discovered as an incidental finding during screening.
- The pathology does not have serious consequences and does not affect the life and health of the child, therefore it does not require treatment.
- The prognosis is favorable.
How often should you have an ultrasound during pregnancy?
The standard number of procedures is 2-3, but in some cases the patient has to visit the diagnostic room several times a month. These are women who are at risk due to the high likelihood of developing abnormalities in the fetus. People in this category include:
- over 35 years old;
- having children with congenital pathologies;
- with a family history;
- exposed to radiation, in contact with toxic substances;
- having a history of premature birth, cases of stillbirth or fetal death in the womb, miscarriages.
Do not be alarmed if the doctor prescribes an additional ultrasound - careful monitoring of the condition of the fetus allows you to avoid congenital pathologies and notice deviations from the norm in the early stages.
Origin
The choroid plexuses are derivatives of the pia mater, which are localized in the ventricles of the brain. During embryogenesis at week 4, 3 brain vesicles are formed from the neural tube:
- front;
- average;
- diamond-shaped with internal cavities.
The walls of their cavities are lined with a layer of ependymal cells, and the blisters themselves are filled with cerebrospinal fluid (the contents of the future cyst). Blood vessels grow through the cells of the ependyma (the future pia mater) and ensure its protrusion into the cavity of the brain vesicles, where folds of cells form. The choroid plexuses are formed in the following order:
- 4-5 weeks – network in the fourth ventricle;
- 6-7 weeks – network in the third ventricle;
- Weeks 7-9 – lateral ventricles.
Thus, based on the characteristics of the formation of choroid plexus cysts, we can conclude that they do not belong to typical cystic formations (they are regarded as a congenital malformation).
Why are ovarian cysts dangerous?
There are cases when a follicular cyst or corpus luteum cyst bursts and its contents spill into the abdominal cavity. In this case, bleeding may begin, and, as a result, the need for hospitalization in a hospital. In addition, torsion of an ovarian cyst is possible, which is accompanied by severe abdominal pain and also requires treatment in a hospital.
During pregnancy, large ovarian cysts pose a potential danger, since cyst rupture or torsion may occur, in which case surgical intervention is not necessary.
In rare cases, the formation of multiple ovarian cysts causes infertility.
Causes
The exact reason for the development of a cyst in the prenatal state has not been established, but this is not required, given its harmlessness and ability to disappear after a short period of time.
Conditional factors include:
- Genetic mutations (trisomy 18, trisomy 21). In this case, the cyst is only one of the symptoms of the underlying disease. It is important to understand that it is not the cyst that causes the mutation, but the mutation that causes the formation of pathologies (for example, due to divergence or underdevelopment of the skull bones). These pathologies are identified using karyotyping.
- Intrauterine infections . Of particular importance are the herpes virus and cytomegalovirus. In this case, there is a risk that an ultrasound examination will reveal a cystic formation formed directly in the brain tissue (a choroid plexus cyst is formed only at the stage of formation of the brain vesicles, long before the appearance of clearly differentiated organ tissue, but it is not possible to distinguish between these two types in utero). In this case, the cysts will often be multiple and will be located in the frontal and temporal lobes. The pathogenesis is based on necrosis of nervous tissue. To clarify the nature of the neoplasms, PCR of the baby’s blood after birth (DNA/RNA of the virus) is required.
- Traumatic injuries . They can occur either during fetal development or during childbirth. It is necessary to understand that during screening ultrasounds it is not always possible to view all tissues and structures of the fetus (due to its small diameter, the choroid plexus cyst is not always visible). If a cystic cavity is detected in a child during the neonatal period (usually they do not persist until this time, but there are exceptions), it is necessary to carry out a differential diagnosis with hematomas and other formations.
- As a consequence of ischemic stroke . It occurs extremely rarely and usually against the background of severe oxygen starvation (partial placental abruption, concomitant maternal diseases).
- As a consequence of hemorrhagic stroke (ruptured aneurysm). It is extremely rare.
Only general factors that can presumably cause cystic neoplasms are given.
By what signs can you identify a cyst in a child?
Vascular compactions are diagnosed during special diagnostic methods, so ultrasound and neurosonography can provide a complete description of the cyst. According to accepted WHO recommendations, these studies must be carried out on all children under one year of age to exclude possible neurological disorders.
In infants, cystic formation is practically asymptomatic
Mandatory indications for neurosonography are:
- trauma during childbirth;
- high risk of intrauterine infection;
- oxygen starvation of the fetus;
- severe pregnancy;
- the presence of chronic diseases in the mother;
- intense physical activity during pregnancy;
- deviations in the physical development of the newborn (underweight, insufficient growth);
- severe deformation of the anatomical parts of the skull.
According to statistical data, cystic formations are recorded both in children without deviations in physiological development and in those with developmental delays.
Consequences
Choroid plexus cysts do not have any health consequences. Below are the expected complications of any cystic formation (suppuration, rupture):
- prolonged hypertension in newborns;
- focal symptoms due to compression of brain structures (visual impairment, hearing impairment, sensory or motor disorders);
- partial epileptic seizures.
One of the most dangerous, but extremely rare complications is hydrocephalus. It occurs due to blockage of the cerebral aqueduct by a cystic formation. In this case, shunt surgery and a course of medications to normalize brain function in the postoperative period are indicated. Signs of pathology:
- divergence of the skull bones due to increased intracranial pressure;
- bulging and pulsating fontanelles;
- retardation in mental and physical development due to prolonged ischemia of the cerebral cortex.
Choroid plexus cysts are far from the first and extremely atypical form of formation that leads to the formation of hydrocephalus (there is no clear evidence base).
Clinical manifestations
Frequent crying and a child’s bad mood is a reason to consult a neurosurgeon
As a rule, if cysts do not disappear on their own, they do not interfere with life and for a long time do not in any way remind of their existence. Brain tissue can be affected in the presence of infectious pathogenesis, trauma, or late appearance of a neoplasm.
The growth of neoplasia provokes the appearance of a certain clinic due to compression of neighboring structures. In addition, increased formation of cerebrospinal fluid is recorded, which causes the appearance of negative manifestations characteristic of hydrocephalus
A typical clinical picture in the presence of large or growing cysts in a newborn:
- attacks of nausea;
- constant regurgitation, vomiting is possible;
- decrease or increase in muscle tone of the arms and legs;
- convulsions;
- coordination disorders;
- strabismus.
The baby becomes lethargic, capricious, sleeps poorly, shows no interest and often cries, which is associated with constant headaches.
Diagnostics
The following methods are used for diagnosis:
- Routine ultrasound in the second trimester. It should be noted right away that if a cyst is detected, the uzologist may not tell the expectant mother anything. The diagnosis is considered legitimate only if a cyst is present after 30 weeks. In this case, the diagnosis is included in the chart and after birth the child is indicated for neurosonography (repeated at 3 months, 6 months and a year). If the cyst enlarges or changes in its shape, more complex diagnostic measures are required (differential diagnosis with similar diseases and, if necessary, correction of the diagnosis).
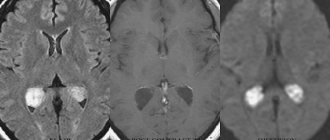
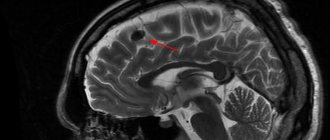
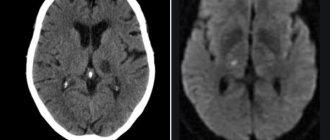
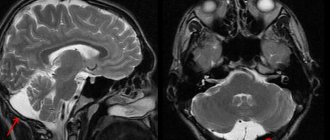
- MRI/CT. Used in cases of questionable diagnosis (signs appear that are atypical for simple choroid plexus cysts).
- Laboratory tests are not carried out (with the exception of PCR), since they are not informative.
Diagnosis of pregnant women is based on critical or sensitive periods of fetal development (the greatest sensitivity to external influences and the greatest risk of developing pathologies, including cystic formations):
| Embryogenesis period | Time | Peculiarities |
| Preimplantation or tubal period | First week of pregnancy | Development of ectopic pregnancy, disruption of division processes and the occurrence of mutations (abnormal mitosis processes) |
| Second period | From 3 to 8 weeks | The initial period of organogenesis, when tissue formation occurs (the formation of the placenta takes 3 months, but begins in this period). It is during this period that the rudiments of the cerebral cortex (bone marrow hematopoiesis) are formed. Beginning of cystic cavity formation |
| Third stage | From 20-24 weeks | This period is associated with the formation of all systems and structures of the body from tissue rudiments (cell differentiation). Approximate time to detect a cystic cavity by ultrasound |
The periods are allocated conditionally, since it is problematic to identify the exact time of formation.
Screening ultrasound in the second trimester of pregnancy can detect a choroid plexus cyst in the fetus
Possible complications
Echo signs of a vascular neoplasm should make a specialist wary. Cysts themselves are not dangerous, but their presence may increase the risk of developing chromosomal pathologies in the future.
Increases in the frequency of cysts are largely influenced by Edwards syndrome
With normal laboratory test results, a vascular cyst does not indicate a pathological process in the body. To exclude genetic abnormalities, the doctor prescribes amniocentesis (sampling of a small amount of amniotic fluid).
In cases where genetic abnormalities are detected in the fetus, their consequences are the following developmental anomalies:
- Down syndrome.
- Edwards syndrome.
Pseudocysts have no absolute influence on the development of genetic defects, since they also occur in healthy children.
Treatment
Not required in 95-98% of cases. Only monitoring of the child's condition is indicated.
If clinical manifestations occur, medications may be prescribed:
- Antiviral agents – for laboratory-confirmed herpes virus (Acyclovir).
- Drugs that reduce intracranial pressure (diuretics) – if signs of hydrocephalus occur (Spironolactone).
- Anticonvulsants - they are prescribed not only when an epileptic focus has formed in the brain, but also when there is pronounced activity of the neural network (pre-epileptic state).
- Weak sedatives – for increased excitability (Glycine).
- Antioxidant complexes and nootropics - to restore metabolic processes in the brain and normalize blood circulation.
All these groups of drugs are used only to eliminate symptoms.
Types of cystic formations
There are several types of vascular cysts. They differ in the process of formation and localization.
Left
It is determined in the left lobe of the brain even before the birth of the child. This is a unilateral formation that does not cause disease of the nervous system. In 95% of cases, it indicates an active accumulation of cerebrospinal fluid. In infants, pseudocysts of the left choroid plexus appear against the background of severe trauma or hypoxia.
On right
Right-sided pathology differs from left-sided only in location. Numerous observations suggest that normalization of the choroid plexus occurs up to 22-24 weeks of pregnancy. A cyst in the right choroid plexus, which is of normal size, does not have a negative effect on the nervous tissue.
Bilateral pseudocysts
Requires more careful monitoring.
Such formations already have a more complex development mechanism and manifest themselves with clear signs. They require more careful monitoring of the development of the fetus and newborn.
There are three types of pseudocysts that are caused by injury to the fetus or infections of the pregnant woman - choroidal, subependymal and arachnoid. With their intensive growth, there may be a threat of diseases of the nervous system.
- Focal changes in the brain of vascular origin