Home>Articles>Alcoholic encephalopathies: signs, forms, treatment
quick menu (hide)
- Symptoms of alcoholic encephalopathy
- Development of the disease
- Acute types of disease
- Chronic form of alcoholic encephalopathy
- Diagnosis and treatment
Chronic alcohol abuse leads to the development of various mental and physical problems over time. All organs in the body are affected by excessive use of a toxic substance, including brain function. Alcoholic encephalopathy manifests itself during the transition from stages II to III of alcoholism, but in some cases much earlier. The disease, whether acute or chronic, interferes with a person's ability to think rationally and retain memories. If left untreated, it can lead to permanent brain damage.
Content:
- What you need to know about the disease
- Where does the disease come from?
- Types of disease
- Acute forms 4.1. Gaye-Wernicke syndrome 4.2. Mitigated acute encephalopathy 4.3. Illness with fulminant course
- Chronic encephalopathies in alcohol addiction
- Patient examination
- How is the treatment carried out?
- Quitting alcohol is a prerequisite for recovery
Alcoholic encephalopathy is a dangerous disease that leads to damage to brain cells.
People who abuse alcohol and are in the second or third stage of alcoholism face it. The pathology occurs in acute or chronic form. It is characterized by pronounced somatic, mental and neurological disturbances. If you delay treatment, your body weight will begin to decrease, orientation in space will be disrupted, lethargy and fatigue will become constant companions of life.
To rid a person of the signs of the disease, doctors carry out medication correction. If necessary, drugs are combined with psychotherapy sessions.
There is no point in fighting the disease on your own - it will not be possible to win such an unequal battle. Only by enlisting the help of a narcologist can a patient count on the disappearance of painful symptoms.
Why is hospitalization required?
The most important thing is to save a person’s life and minimize the toxic effects of alcohol. Without complete, active specific therapy, patients die much more often. In any case, it is impossible to provide the entire necessary range of activities at home. Even if it costs a lot. In such situations, a person must be observed simultaneously by several doctors of different specializations. And at home, 24-hour monitoring, at least 3 specialists, and this is a very big luxury. As a rule, after an acute attack of illness at the time of another binge, a person sharply degrades. This usually manifests itself in unfunny, offensive, obscene jokes, statements, and anecdotes told. Nystagmus and optic nerve palsy begin to form, which persists and develops as a consequence of the disease. Treatment of alcoholic encephalopathy provides some relief of symptoms, but does not go away completely.
As usual, treatment of alcoholic encephalopathy is effective and does not bring complete relief to about 50% of patients. Impaired motor function does not disappear completely, the gait continues to be slow, clumsy, and they spread their legs wide apart when walking.
Treatment methods for alcoholic encephalopathy developed at the Transfiguration clinic for the most part bring more than 30% of patients almost complete restoration of motor and mental functions. Concomitant diseases are also compensated. Only in the most severe cases, and this is less than 20%, treatment of alcoholic encephalopathy does not bring complete relief. The remaining 50% of cases have a completely positive effect, with complete restoration of all functions.
After hospitalization
Alcoholic encephalopathy disrupts gait and forms horizontal nystagmus, which is the main symptomatology. This is accompanied by alcoholic dementia and complex somatic pathology. Recovery of the vestibular apparatus is usually slow, as is the regression of ataxia. It takes several weeks or months, depending on the severity of the condition. However, in very severe cases it is not always complete.
Apathy, lethargy and confusion begin to decrease gradually, while long-term memory takes much longer to fully recover. Long-term memory and learning ability (Korsakoff's syndrome) may remain as a long-term effect.
It should be emphasized that patients with alcohol dependence, exhaustion and Korsakoff psychosis are not divided into separate diseases. This is one disease, the sources of which can be various reasons.
Oculomotor disorders, ataxia, global disorientation and amnestic syndrome are successive phases of regression in the context of a single pathological process. Korsakoff psychosis is one of the components of alcoholic encephalopathy.
What you need to know about the disease
This disorder is characterized by the rapid destruction of brain cells. The first symptoms of the disorder are preceded by a long period of drunkenness - from seven to twenty years. But an earlier onset of the disease cannot be ruled out.
Alcoholic encephalopathy is a diagnosis that should not be joked with. The sooner treatment is started, the higher the chances of brain recovery. And, conversely, in advanced cases, it is not always possible to achieve a return to high-quality brain activity.
Often, in parallel with the disease, a psychoorganic syndrome develops - a symptom complex indicating organic damage to brain structures. Then the drinker becomes emotionally unstable, he experiences memory loss, and his intellectual abilities are greatly reduced.
Conditional classification
There is no generally accepted division of these ailments of similar origin.
The development of the encephalopathic process occurs:
- acute, “super-acute”;
- subacute;
- chronic.
The onset of the disease is preceded by a period of prodromal (preliminary) complaints. Its duration can be from 2-3 weeks to a year.
Prodrome is characterized by:
- Asthenic syndrome with adynamia and physical exhaustion.
- Dyspeptic disorders - heartburn, belching, aversion to certain types of food. Patients experience abdominal pain, alternating diarrhea and constipation.
- Psychoorganic manifestations - sleep disturbances, nightmares, fears, complaints of body pain and limb cramps, a sharp decrease in visual function.
Describing the clinical picture of these diseases at a popular level is very difficult. Without special medical education, it will be difficult to discern the difference between the specific changes characteristic of each type of encephalopathy. Therefore, in the description we will only touch on some of the main points, or even just limit ourselves to the names of the ailments.
Where does the disease come from?
Almost always, the diagnosis described is a consequence of many years of drunkenness. The first signs of pathology appear after a prolonged binge. Those at risk for this problem are people who, in order to save money, use industrial alcohol and toxic alcohol substitutes.
Doctors know cases where the disorder developed in people who do not suffer from alcoholism. The individual characteristics of the human body are to blame here. Then, sometimes taking small doses of alcohol, he is faced with abnormal destruction of brain tissue.
At the physiological level, metabolic abnormalities contribute to the occurrence of a malfunction. A deficiency of B vitamins is especially dangerous. As is known, ethanol does not allow them to be absorbed and absorbed. Then the activity of the entire nervous system is disrupted.
Prevention
{banner_banstat9}
The set of measures includes:
- monitoring blood glucose levels;
- monitoring blood pressure and taking appropriate medications;
- eradication of alcoholism;
- refusal of alcohol;
- good nutrition;
- healthy sleep;
- playing sports.
All patients are very different from each other, so the treatment algorithm is drawn up taking into account the individual characteristics of the patient.
But the main condition for successfully combating the consequences of the disease is detection of the disorder in the early stages
and timely treatment.
Types of disease
Narcologists classify brain disease in alcohol addicts taking into account the following criteria:
- dominant symptoms;
- speed of development;
- flow features;
- frequency of exacerbations;
- degree of mental health.
The disease can occur in two forms:
- Spicy. This group includes Gaye-Wernicke syndrome, a pathology of the mitigated type and with a fulminant course.
- Chronic. Korsakov's psychosis and alcoholic pseudoparalysis have a long development.
Causes of pathology
The occurrence of this type of encephalopathy occurs due to a failure of the body’s metabolic processes characteristic of chronic alcoholism:
- lack of vitamins B1 and B6;
- lack of microelements;
- damage to nerve cells and the formation of substances that have a neurotoxic effect;
- disturbances in the functioning of the hypothalamus.
Algerica - a medicine or a drug, a help or aggravation of the patient’s condition, a panacea or a poison? Look for the answer in our article.
How first aid should be provided for epilepsy - video instructions and tips in our material.
At-risk groups
The development of encephalopathies due to alcohol abuse covers different groups of people, but still has some features.
Gaye-Wernicke encephalopathy
suffer more often:
- male representatives 35-45 years old;
- There are cases of the disease developing even at 20 years of age.
Korsakoff psychosis:
predominantly women.
Alcoholic pseudoparalysis
often develops:
- in men from 35 years to 65 years;
- less often - women from 30 to 65 years old.
There is also a general tendency to all types of encephalopathies due to a predisposition to drinking alcohol:
- inability to adapt to changing environmental conditions;
- subject to the influence of the majority;
- nervous disorders due to constant emotional discomfort;
- lack of education;
- life circumstances;
- heredity;
- dysfunctional family environment;
- family traditions.
Acute forms
Before the disease develops, so-called warning symptoms occur.
The patient becomes lethargic, complains of loss of strength and weakness. His appetite is worsening. He does not want to eat foods rich in fats and proteins. He prefers high-carbohydrate dishes, which further aggravates his condition. Encephalopathy may be preceded by anorexia. Then malfunctions in the functioning of the stomach and intestines appear. The beneficial microelements supplied with food are poorly absorbed. Exhaustion is getting worse.
Gaye-Wernicke syndrome
Appears in alcoholics with acute thiamine deficiency. In the absence of vitamin B1, some important metabolic reactions become impossible. The utilization of glucose by nerve cells is suppressed (they suffer from a lack of energy). Extracellular accumulation of glutamate occurs, which causes hyperactivation of the channels through which calcium ions enter neurons. Excess intracellular calcium destroys the cell and creates conditions for its self-destruction.
With Gaye-Wernicke syndrome, the most severely damaged cerebral tissues are in the area of the III and IV ventricles and the Sylvian aqueduct. Stable activity of the brain stem, diencephalon, and cerebellar vermis becomes impossible. This leads to serious memory disorders.
Gaye-Wernicke syndrome can be recognized by the triad of manifestations:
- confusion;
- movement coordination disorder;
- oculomotor failure.
Mitigated acute encephalopathy
The development of pathology begins with:
- depressed mood;
- asthenia;
- lack of appetite;
- insomnia at night and drowsiness during the day.
The drinker is nervous and worried a lot. He has a tendency towards hypochondria, a mental disorder in which there is a feeling of approaching death. A person is constantly trying to find symptoms of a dangerous disease. Because of this, his quality of life is deteriorating.
Abnormal activity is indicated by recurring neuritis. The prodromal period in an addict often lasts longer than a month, and then turns into delirium.
Illness with fulminant course
Often leads to death. The warning signs last for about three weeks. Afterwards, severe psychosis occurs. The patient begins to feel unwell. He experiences somatic pain, fainting, and hallucinations. Body temperature can rise to 41°C.
Before death, addicts with the fulminant form fall into a coma. Even if a person manages to survive with this diagnosis, he will no longer be mentally normal.
First aid
First aid if alcoholic encephalopathy of the brain is suspected has the following specifics:
- you need to wrap the person well in a blanket to keep warm;
- make sure that if there is vomiting, the patient does not choke on the vomit;
- wait for the ambulance to arrive.
One should not discount the condition as a result of which a person falls into a coma.
In this case, you should trust your doctors.
It should be borne in mind that even if you get out of this state with the help of medications and the help of doctors, this will not go away without consequences for the body, because it receives extreme stress.
Chronic encephalopathies in alcohol addiction
Chronic forms of the disease are distinguished by a long and indolent course. In the case of Korsakov's psychosis, memory lapses plague the patient. A person talks about something that didn’t really happen. He is unable to remember new information and is poorly oriented in the surrounding space.
The patient's vocabulary becomes quite modest. He makes few body movements. Often encounters symptoms of neuritis.
As for the second form of chronic encephalopathy - alcoholic pseudoparalysis - men are more prone to it. A person loses many skills and forgets what he knew before. He becomes rude, aggressive and cynical. Can't take care of himself properly. Those around him have to endure sudden mood swings when communicating with him.
Neurological distress in pseudoparalysis is manifested by speech disorders, tremor of the limbs and face, and polyneuritis.
Clinical picture
Alcoholic encephalopathy has 2 forms:
- acute alcoholic;
- chronic form - alcoholic pseudoparalysis, Korsakov psychosis.
Less common are other forms of the disease, the cause of which is the consumption of different types of wine.
Features of the period of development of the disease:
- asthenia;
- adynamia;
- lack of appetite;
- painful thinness;
- nausea and vomiting - in the morning;
- diarrhea;
- stomach ache;
- belching;
- heartburn;
- constipation;
- sleep disturbance;
- profuse sweating;
- heart pain;
- dyspnea;
- lack of air;
- numbness, pain and aches in the limbs;
- disturbance of consciousness;
- anxiety;
- speech disorders;
- coma - in severe cases;
- twitching of the tongue, lips, face;
- problems with eye function;
- puffiness;
- temperature is above normal;
- skin is dry, flaky or greasy;
- bedsores;
- dizziness;
- nervous disorders;
- memory loss;
- disorientation;
- polyneuritis;
- epilepsy attacks.
The diagnosis is determined against the background of studying information about the occurrence and development of the disorder and clinical picture data.
How is the treatment carried out?
The fight against alcoholic encephalopathy includes:
- Normalization of nutrition. The patient needs to eat more foods containing fats and proteins.
- Vitamin therapy. It is important to take increased doses of thiamine.
- Taking nootropics. These are medications aimed at improving brain activity and protecting brain cells from destruction.
- The use of medications that increase blood circulation and metabolism in the brain.
At the same time, the addict is prescribed treatment for the somatic disorders that have arisen.
Complications and consequences
The consequences of the disease coincide with its symptoms and are special for each type of encephalopathy.
Alcoholic encephalopathy has the following consequences:
- high blood pressure;
- heart disorders;
- heartburn;
- disturbances of eye functions;
- muscle disorders;
- trophic disorders;
- imbalance;
- neuralgia;
- stiffness of movements.
Complications:
- fetal alcohol syndrome;
- dementia;
- speech disorder;
- partial memory loss;
- schizophrenia;
- brain tumor;
- inability of the brain to work;
- urinary and fecal incontinence;
- neuritis;
- paralysis of limbs;
- epileptic seizures.
Quitting alcohol is a prerequisite for recovery
It is impossible to cure an illness caused by drunkenness without giving up alcohol. Therefore, the fight against encephalopathy should begin with coding. The patient should make an appointment with a narcologist and choose the best option for prohibitive therapy. This could be hypnosis, Dovzhenko stress therapy, medication or hardware correction.
Sobriety will create the conditions necessary to restore full brain activity. But you must observe the “law of sobriety” for the rest of your life. As soon as the patient violates this requirement, he will again become a binge alcoholic with severe mental disorders.
Forecast
Cure predictions are directly related to the clinical picture of the deviation.
The forecast depends on:
- duration of the disease;
- frequency of use;
- type of alcohol;
- drinking low-quality alcohol;
- heredity and environment;
- the nature of the consequences of alcohol exposure.
The prognosis is not positive for the onset of alcoholism in adulthood. In advanced cases, mental and physical disability increases, despite abstinence from alcohol, due to metabolic failure, nutrition, and disturbances in the functioning of internal organs.
Literature:
- Fadeeva O. V. Alcoholic encephalopathy at a young age: clinical, therapeutic and socio-demographic features. Abstract, dissertation of a candidate of medical sciences, 14.00.13. Place of defense: Scientific Center of Neurology of the Russian Academy of Medical Sciences. - Moscow, 2008. - 25 p.
- Mendelevich S.V. Motor, cognitive and emotional-personal disorders in patients with alcoholic encephalopathy. Abstract, dissertation. candidate of medical sciences, 14.00.13. Place of protection: Moscow Medical Academy named after. THEM. Sechenov. - Moscow, 2009. - 24 p.
- Shulyak Yu. A. Features of the clinic and therapy of alcoholic encephalopathies with various variants of their course. Dissertation of a candidate of medical sciences, 14.00.18. Place of defense: Moscow State Medical and Dental University. - Moscow, 2008. - 158 p.
Alcoholic encephalopathy - symptoms and treatment
Factors in the pathogenesis of alcoholic encephalopathy
The following factors play a role in the pathogenesis of alcoholic encephalopathy:
1. Genetic factor, namely the activity of enzymes that utilize alcohol:
- alcohol dehydrogenase (ADH) - converts ethanol into acetaldehyde;
- acetaldehyde dehydrogenase (ALDH) - oxidizes acetaldehyde to acetic acid.
The hereditary combination of high ADH activity and low ALDH activity is an unfavorable prognostic factor, since when drinking alcohol, acetaldehyde accumulates in the tissues, which has a direct toxic effect on target organs.
2. Immunological disorders. A significant link in the pathogenesis of addiction diseases, including alcoholism, is a violation of the mechanisms of interaction between the immune and nervous systems. This disorder is manifested, among other things, by the increased production of antibodies to neurotransmitters (biologically active substances that transmit information between nerve cells): serotonin, glutamate, dopamine, norepinephrine [7][17][20].
This is explained by the fact that alcohol stimulates the production of these neurotransmitters, which is why a person feels joy and euphoria. In response to the release of mediators, the body produces more antibodies. At the same time, people with alcohol dependence with long-term abstinence from alcohol have the highest level of antibodies to neurotransmitters. This pattern characterizes the biochemical features of alcohol dependence [20].
3. A decrease in the content of gamma-aminobutyric acid (GABA) in brain tissue promotes hyperactivation of nerve cells, since GABA is a neurotransmitter that provides inhibition of cells of the central nervous system.
4. Excitotoxic effects of glutamate. First, it is worth explaining that excitotoxicity is a pathological process as a result of which nerve cells die from exposure to neurotransmitters. The fact is that the effect of alcohol on a specific glutamate receptor - N-methyl-D-aspartate (NMDA) - makes it hypersensitive to the neurotransmitter glutamate.
Receptors are a kind of door that closes the entrance to the cell. Neurotransmitters are the “keys” that open these “doors.” The “key” for the NMDA receptor is glutamic and aspartic acids. When these acids act on the receptor, the “door” opens and calcium and sodium ions enter the cell.
Ethanol blocks the functioning of NMDA receptors. However, with chronic use, the receptors adapt to the suppressive effect of ethanol and become more sensitive. At the same time, the release of glutamate increases to maintain a constant internal environment of the body.
When a person gives up alcohol, ethanol stops suppressing receptors; due to the sensitivity of NMDA receptors and high levels of glutamate, the glutamatergic system is hyperactivated. What does this mean: glutamate has an excessive effect on the receptors, the receptor channel remains open for a long time and through it too many calcium ions enter the cell, which triggers the process of cell death. Thus, the excitotoxic effects of glutamate can be described by three processes:
- first, with prolonged alcohol consumption, increased sensitivity of NMDA receptors is formed;
- when you give up alcohol, ethanol stops blocking receptors;
- due to hyperactivation of NMDA receptors and excessive intake of calcium ions into the cell, nerve tissue is damaged.
5. Violation of water-electrolyte balance and acid-base balance. Dehydration occurs with a lack of potassium and magnesium ions, a decrease in blood pH - a shift in the blood reaction to the acidic side.
6. Increased permeability of the blood-brain barrier (between the circulatory and central nervous systems). It occurs due to the fact that alcohol and its breakdown products damage the endothelium (inner layer) of blood vessels, resulting in the formation of “systemic capillary toxicosis” (vascular damage).
7. Liver damage and decreased function. The toxic effect of alcohol and its metabolic products ultimately leads to liver cirrhosis (replacement of working liver cells with connective tissue). As a result, the liver functions to synthesize proteins and neutralize toxic substances, including repeated doses of alcohol, are disrupted. Liver damage disrupts metabolism and leads to toxin poisoning, which negatively affects all internal organs, including the brain with the formation of hepatic encephalopathy.
8. Excessive synthesis of aromatic amino acids. As a result of liver damage, the amount of aromatic acids in the blood increases: phenylalanine, tyrosine, tryptophan and histidine. These substances are precursors of aminergic neurotransmitters (serotonin). Thus, an imbalance of mediators occurs: an increase in the amount of serotonin and phenylethylamines (thyronine, octapamine, phenylethanolamine) and a decrease in dopamine and norepinephrine. This disrupts metabolism and the balance of excitation and inhibition of the nervous system.
10. Impaired absorption of nutrients in the gastrointestinal tract as a result of the irritating effect of strong alcohol or its surrogates.
11. Deficiency of thiamine (vitamin B1) and other vitamins, microelements, alpha-lipoic acid as a result of an unbalanced diet in alcoholism and malabsorption in the gastrointestinal tract.
Organic changes in the brain
All these factors lead to organic changes in the brain:
1. Cerebrovascular accident. It manifests itself as sclerosis (narrowing) of cerebral vessels and pathological (painful) plethora, which is often detected during post-mortem examination of deceased patients who suffered from alcoholism. When large doses of alcohol are consumed, the permeability of the vascular wall increases, which promotes edema, glomerular filtration in the kidneys increases, and the amount of fluid in the vascular bed decreases (dehydration), followed by thickening of the blood (hemoconcentration). All this disrupts cerebral circulation and contributes to the formation of atherosclerotic plaques.
2. At the cellular and tissue level, a change in the structure of nerve and glial cells is observed - vacuolar (hydropic) dystrophy develops.
Against the background of tissue energy deficiency and hypoxia progressing during alcoholism, the function of K+ / Na+-ATPase is impaired. It is a membrane enzyme that is responsible for the transport of ions across the membrane and regulates cellular volume. When the function of this enzyme is disrupted, an excess amount of sodium ions enters the cell. Sodium ions attract excess water through the membrane. Excess fluid first enters the cisterns of the Golgi apparatus, which is responsible for completing the synthesis and excretion of organic substances produced in the cell. The cisterns increase in size, turning into cavities filled with liquid (vacuoles), their contents become light, and their function is impaired. Vacuoles, increasing in size, are able to merge and fill a significant part of the cell.
Further, according to a similar mechanism, mitochondria (intracellular structures responsible for energy processes - respiration) “swell”, this further aggravates the energy deficiency. Lysosomes also change, which break down unnecessary obsolete cell components using hydrolytic enzymes. Ultimately, a change occurs in the nucleus of the nerve cell.
Due to excess fluid, the nerve cell swells, so-called cytotoxic edema is formed. The membranes of the “vacuoles” are eventually destroyed and their contents, including the contents of lysosomes, end up in the cytoplasm of the affected cell. The environment inside the cell against the background of energy deficiency becomes acidic (intracellular acidosis), lysosomal enzymes are activated, and the cell finally destroys itself.
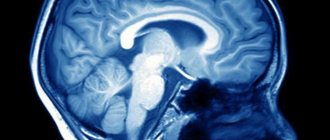
3. Pathological postmortem studies of patients with alcoholic encephalopathy and neuroimaging methods (MRI, CT) showed that the brain as a whole (brain morphology) changes. The ventricles of the brain filled with cerebrospinal fluid (CSF) are enlarged, the mass of the brain matter is reduced, primarily due to the cerebral hemispheres and cerebellum.
On sections of the brain, foci of demyelination (loss of nerve conductors of their sheath) and formed foci of proliferation of the connective tissue of the brain - glia (foci of gliosis) are noted. Alcoholic encephalopathy is characterized by damage to the subcortical ganglia:
- Cholinergic nuclei at the base of the brain. They are involved in the production of the neurotransmitter acetylcholine, which mediates neuromuscular transmission.
- The locus coeruleus is a formation located in the brain stem. It is involved in information processing and learning, and is also responsible for the body's reactions to anxiety and stress.
- The raphe nuclei are clusters of neurons located along the midline of the medulla oblongata. Participate in serotonin metabolism. Impairment in this area appears to provoke depression in patients with alcoholism.
The hippocampus, the brain structure responsible for remembering, is damaged to varying degrees. In classical Wernicke-Korsakoff encephalopathy, hemorrhages and foci of necrosis (death) of nervous tissue are found in the hippocampus.
According to animal studies, both long-term and short-term alcohol use can cause brain damage.
When abstaining from alcohol for 1-5 months, restoration of brain volume is observed, but it may be incomplete, since dead nerve cells are not restored. It should also be noted that giving up alcohol will not necessarily lead to the restoration of all brain functions, since this occurs due to an increase in the size and connections of surviving neurons and the proliferation of glial cells [1][2][3][4][5][7 ][10][15].