The most common complaint that doctors hear from their patients is headache. Both adults and children complain about it. It is impossible to ignore this. Especially if there are other symptoms. Parents should pay special attention to the child’s headaches and the baby’s behavior, because he cannot say that he is in pain. Perhaps these are the consequences of a difficult birth or congenital anomalies, which can be determined at an early age. Maybe these are liquorodynamic disturbances. What is it, what are the characteristic signs of this disease in children and adults and how to treat it, we will consider further.
What does liquorodynamic disturbances mean?
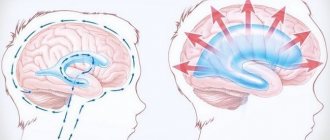
Liquor is cerebrospinal fluid that constantly circulates in the ventricles, cerebrospinal fluid ducts and in the subarachnoid space of the brain and spinal cord. Liquor plays an important role in metabolic processes in the central nervous system, in maintaining homeostasis in brain tissue, and also creates a certain mechanical protection for the brain.
Liquorodynamic disorders are conditions in which the circulation of cerebrospinal fluid, its secretion and reabsorption are impaired. These processes are regulated by glands located in the choroid plexuses of the brain ventricles that produce fluid.
In the normal state of the body, the composition of the cerebrospinal fluid and its pressure are stable.
Diagnosis of pathologies
Currently, there are several methods for diagnosing liquorodynamic disorders. The basis in this case is complaints and the clinical picture. In order for the doctor to make a more accurate diagnosis, it is necessary to initially talk with the patient, ask him about the complaints, the time of their appearance, duration, as well as the conditions against which they appear.
The accuracy of the diagnosis and the reduction of possible examinations are reduced after examining the patient; it is preferable to do this not during a period of calm and absence of a clinic, but at the moment of manifestation of the disease.
An examination is carried out, great attention is paid to checking nystagmus and palpation of muscles, especially the occipital muscles. After this, instrumental and laboratory diagnostic methods begin.
Laboratory
The most common and economically less expensive is a general blood test. It indirectly determines the presence of an inflammatory process. This is necessary to confirm or, conversely, exclude a possible cause of the disease.
Cerebrospinal fluid examination. The method is less common and requires highly trained specialists for this manipulation. With its help, the nature of the contents contained in the cavity of the brain and spinal cord is clarified. In case of liquorodynamic disorders, an increase in protein content may be detected. A mandatory point is the complete absence of an inflammatory component.
There are many more instrumental diagnostic methods compared to laboratory ones, and in addition, they have greater diagnostic value. Among them are the following:
- Ultrasonography. It allows you to evaluate not only the structures of soft tissues, but also possible mechanical causes that create a violation of the outflow of fluid.
- Angiography is a method for determining the condition of the vascular component of the body. In cases of liquorodynamic disorders, examination of the vessels of the head and neck is of great importance. With its help, you can identify even small disorders that give a clinical picture of the disease.
- Echoencephalography. This is a non-invasive way to detect pathological changes in the transmission of nerve impulses at the level of the brain substance.
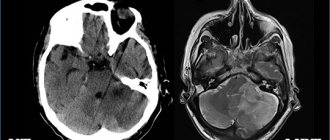
- Computer or magnetic resonance imaging . These are ways to assess the state of brain structures, the volume of cavities and the sizes of component parts. Recently, the technique has become very popular due to the high accuracy of the resulting image compared to the previously common method of x-ray examination. Its significant disadvantage is high economic costs, as well as in some regions inaccessibility.
It is after a correctly developed diagnostic plan and the data obtained that the issue of selecting treatment is decided. It is useless to treat only symptoms, as this can lead to more rapid development of complications.
What is the mechanism of violations
Let's consider how liquorodynamic disorders of the brain can develop:
- The rate of production and release of cerebrospinal fluid by the choroid plexuses increases.
- The rate of absorption of cerebrospinal fluid from the subarachnoid space slows down due to the blocking of the narrowing of the cerebrospinal fluid vessels due to previous subarachnoid hemorrhages or inflammatory diseases of the meninges.
- The rate of CSF production decreases during the normal absorption process.
The rate of absorption, production and release of cerebrospinal fluid is influenced by:
- On the state of cerebral hemodynamics.
- State of the blood-brain barrier.
The inflammatory process in the brain increases its volume and increases intracranial pressure. The result is poor circulation and blockage of the vessels through which the cerebrospinal fluid moves. Due to the accumulation of fluid in the cavities, partial death of intracranial tissue may begin, and this will lead to the development of hydrocephalus.
Prevention of violations
This is one of the most important stages aimed at preventing not only liquorodynamic disorders, but also complications associated with them.
First of all, this is to prevent the development of the congenital form of this disease. If family members have hereditary pathologies, especially those related to circulatory disorders or developmental defects of various organs, it is necessary to consult a geneticist for advice. This is necessary to exclude the possible transmission of disorders associated with genetic mutations transmitted by inheritance.
As well as careful pre-conception preparation of a woman to prevent the development of inflammatory diseases at the stage of bearing a child.
Among the measures to prevent acquired conditions, the following should be highlighted:
- Prevention of infectious inflammatory diseases associated with damage to the nervous system.
- Monitor the state of the blood coagulation system, avoid hypercoagulation and stressful situations, as well as surges in blood pressure.
- Monitor your posture and prevent the development of osteochondrosis, especially in the cervical spine. To do this, you regularly need to carry out physical exercises aimed at strengthening your muscles. When working in a forced position of the body, take regular breaks to relax muscle fibers, as well as prevent stagnation.
Classification of violations
Liquorodynamic disorders are classified in the following areas:
- How does the pathological process proceed:
- Chronic course.
- Acute phase.
2. Stages of development:
- Progressive. Intracranial pressure increases and pathological processes progress.
- Compensated. Intracranial pressure is stable, but the ventricles of the brain remain dilated.
- Subcompensated. Great danger of crises. Unstable condition. Blood pressure can rise sharply at any moment.
3. In which cavity of the brain is the cerebrospinal fluid located:
- Intraventricular. Fluid accumulates in the ventricular system of the brain due to obstruction of the cerebrospinal fluid system.
- Subarachnoid. Liquorodynamic disturbances of the external type can lead to destructive lesions of brain tissue.
- Mixed.
4. Depending on the pressure of the cerebrospinal fluid:
- Hypertension. Characterized by high intracranial pressure. The outflow of cerebrospinal fluid is impaired.
- Normotensive stage. Intracranial pressure is normal, but the ventricular cavity is enlarged. This condition is most common in childhood.
- Hypotension. After surgery, excessive outflow of cerebrospinal fluid from the ventricular cavities.
Treatment of diseases
It will largely depend on the cause that caused the clinical manifestations. Therefore, this therapy is also called etiopathogenetic. If the cause is congenital, associated with structural anomalies, then surgical intervention may be required to create artificial drainage systems or restore the outflow disorder. Such methods currently help cope well with hydrocephalus in the early stages of its course. Some congenital anomalies in the development of the brain or spinal cord, as well as bone structures, cannot be eliminated.
In case of thrombotic disorders that cause outflow disturbance, the use of anticoagulants, as well as agents that promote the resorption of blood clots, is required.
Tumor processes need to be treated using a comprehensive method. It will include surgery and, at the discretion of the specialist, chemotherapy or radiation therapy.
If the root cause is an infectious agent, anti-inflammatory treatment is prescribed taking into account the sensitivity of the pathogen.
Since currently most liquorodynamic disorders can occur due to outflow disturbances due to changes in posture, much attention is paid to this method of treatment. In adults, it is quite difficult to completely correct the situation, and this may require complexes of surgical and physical methods; in childhood, you need to consult a specialist in order to select the most effective exercises aimed at improving the muscular corset of the spine.
Causes congenital
There are congenital anomalies that can contribute to the development of liquorodynamic disorders:
- Genetic disorders in intrauterine development of the fetus.
- Agenesis of the corpus callosum.
- Dandy-Walker syndrome.
- Arnold-Chiari syndrome.
- Encephalocele.
- Stenosis of the cerebral aqueduct, primary or secondary.
- Porencephalic cysts.
Acquired reasons
Liquorodynamic disorders can begin to develop for acquired reasons:
- Spinal cord and brain injuries.
- Various infectious diseases and parasitic infections that affect the nervous system.
- Neoplasms inside the skull that block the cerebrospinal fluid pathways.
- Thrombosis.
- Intrauterine hypoxia in the first two days after birth.
- Papillomas of the choroid plexus.
Possible results
MRI of the brain can reveal the following pathological conditions:
- Oncological pathologies in the brain.
- Various pathologies of infectious origin that affect the patient’s central nervous system.
- Cystic formations affecting the cerebrospinal fluid ducts.
- Hypoxia, which caused hemorrhage in the skull and impeded the movement of cerebrospinal fluid.
- Brain injuries leading to dysfunction of the cerebrospinal fluid.
Treatment after MRI of the brain will be selected individually for each patient, depending on the results of the study and the advanced stage of the disease.
Symptoms of disorders in infants
Liquorodynamic disorders in children under one year of age have the following symptoms:
- Frequent and profuse regurgitation.
- Unexpected crying for no apparent reason.
- Slow overgrowth of the fontanel.
- Monotonous crying.
- The child is lethargic and sleepy.
- Sleep is disturbed.
- Seams coming apart.
Over time, the disease progresses more and more, and signs of liquorodynamic disorders become more pronounced:
- Tremor of the chin.
- Twitching of limbs.
- Involuntary shudders.
- Life support functions are disrupted.
- Disturbances in the functioning of internal organs for no apparent reason.
- Possible squint.
Visually, you can notice the vascular network in the area of the nose, neck, and chest. When crying or tense muscles, it becomes more pronounced.
The neurologist may also note the following signs:
- Hemiplegia.
- Extensor hypertonicity.
- Meningeal signs.
- Paralysis and paresis.
- Paraplegia.
- Graefe's symptom.
- Nystagmus is horizontal.
- Delay in psychomotor development.
You should visit your pediatrician regularly. At the appointment, the doctor measures the volume of the head, and if pathology develops, changes will be noticeable. So, there may be such deviations in the development of the skull:
- The head grows quickly.
- It has an unnaturally elongated shape.
- The large and small fontanelles swell and pulsate.
- Sutures are coming apart due to high intracranial pressure.
All these are signs that a syndrome of liquorodynamic disorders is developing in an infant. Hydrocephalus progresses.
I would like to note that it is difficult to determine liquorodynamic crises in infants.
Health - medical portal of Azerbaijan
One of the causes of headaches is liquorodynamic disorders. When a liquorodynamic crisis occurs in children, they cannot accurately convey their sensations, which significantly complicates the doctor’s task.
Things are bad for children under one year old. Children can only scream to notify others that something is bothering them. But what exactly? Understanding this is a difficult task for doctors and parents.
* The syndrome of liquorodynamic disorders is a pathological condition of the body in which the secretion, circulation and resorption of cerebrospinal fluid (CSF) washing the brain is impaired. The disease develops in a hypertensive or hypotensive type and is characterized by severe headaches and frequent crises.
Causes
Liquorodynamic disorders can be congenital or acquired. Congenital anomalies that provoke the development of changes in the circulation of cerebrospinal fluid include the following brain anomalies: - Arnold-Chiari malformation; - Dandy-Walker malformation; - primary or secondary stenosis of the cerebral aqueduct; - agenesis of the corpus callosum; - genetic disorders in the X chromosome; - encephalocele; - porencephalic cysts; - trisomy on chromosomes 13, 18, 9. The list of causes of acquired triggers includes the following anomalies: - Intrauterine hypoxia, leading to intracranial hemorrhage in the first 48 hours after birth. — Injuries to the brain and spinal cord. - Tumors and cysts of the brain that block the cerebrospinal fluid pathways. — Infectious and parasitic diseases affecting the nervous system. — Thrombosis of veins and sinuses. - Papilomas of the choroid plexus.
* During pregnancy, a screening ultrasound of the fetus is performed at 18-20 weeks. During this period, it is already possible to examine the brain and liquor system of the unborn child. This makes it possible to draw a conclusion about the presence or absence of brain pathology in the fetus.
Features of clinical symptoms in children of the first year of life
In children under one year of age with cerebrospinal fluid circulation disorders, parents note frequent and profuse regurgitation, very slow overgrowth of fontanelles, suture dehiscence, spontaneous crying for no reason, after which the children become lethargic and drowsy. As the disease develops, the symptoms also increase, including twitching of the limbs, tremor of the chin, and involuntary shuddering of the baby. It is very important for children under one year old to regularly visit the pediatrician. During the examination, the doctor, during the examination, measures the circumference of the child's head. Normally, the volume of the head increases by 6-7 cm in the first 3 months, and by 0.5-1 cm per month from the fourth month to one year. In the presence of pathological changes, the head grows very quickly and takes on an unnaturally elongated shape, usually in anteroposterior dimensions. The large and small fontanelles in such infants do not close, but rather swell and pulsate. Due to increased intracranial pressure and the plasticity of the connective tissue, the sutures separate. Thanks to this, children remain in the compensation stage for a long time. Increasing hydrocephalus is a clear sign of impaired cerebrospinal fluid dynamics. When examined by a neurologist, focal neurological symptoms are noted: paralysis and paresis, para- and hemiplegia, extensor hypertonicity, nystagmus, Graefe's symptom, meningeal signs. Young patients are characterized by monotonous crying and their sleep is often disturbed. In the area of the bridge of the nose, neck, and upper chest in sick children, a vascular network is pronounced, which becomes visible when the child tenses (crying, trying to raise his head, sit down). In young patients, it is difficult to identify liquorodynamic crises. Children under one year of age may experience disorders of internal organs without objective reasons. Vital functions are impaired. Over time, such children begin to lag significantly behind in psychomotor development. Sometimes a mother’s attention is attracted by the child’s growing squint. An experienced ophthalmologist may already suspect a syndrome of liquorodynamic disorders based on changes in the fundus of the eye.
Clinic for children after one year
After the child’s skull has fully formed and the fontanelles have closed, the sutures have ossified, and symptoms of increased intracranial pressure begin to predominate. Children complain of headaches, apathy, followed by anxiety, impaired coordination of movements, gait, and speech. Liquorodynamic headache occurs in attacks, often in the morning, and may be accompanied by nausea and vomiting. There is no relief after vomiting. Such children have poor vision, horizontal nystagmus is noted, and due to muscle paralysis they cannot look up. In severe cases, the “bobble doll head” symptom is observed. Increased symptoms are called “liquid dynamic crises.” If the disease occurs at an early age, children speak poorly or do not speak at all. Changes in mental development from minimal to extreme idiocy. Such children use standard memorized phrases in their speech, often without understanding their meaning. They are always in a good mood. Children also have disorders of the endocrine system, most often they manifest themselves in the form of obesity and delayed sexual development. Over time, convulsive syndrome increases in young patients.
Diagnostics
In children under one year of age, the diagnosis of liquorodynamic disorders consists of collecting a pregnancy history, parental complaints, examining the child by specialists (neurologist, ophthalmologist), fundus examinations, and instrumental studies, including ultrasound, magnetic resonance imaging, neurosonography, computed tomography.
In children over one year of age, complaints are also collected for diagnosis, examined by specialists, and MRI and CT are used from instrumental studies.
Treatment
The treatment method is chosen based on etiological factors, the patient’s age, and the presence of concomitant pathology. There are medicinal and surgical types of therapy. Drug therapy is used to reduce the volume of circulating cerebrospinal fluid, its formation, and reduce intracranial volume. For this purpose, Diacarb and Furosemide are prescribed. These drugs are often used in neonatal practice, despite the risk of complications. To achieve maximum effect, drugs are combined in different dosages. Steroids are also used. Their action in this situation is aimed at reducing cerebral edema. The decision to perform surgical treatment is made if it is necessary to reduce intracranial action and reduce neurological symptoms. Indications for surgical treatment:
— occlusive form of hydrocephalus, confirmed by MRI data; - lack of effect from drug treatment; — liquorodynamic crisis. In each case, the decision about surgical intervention is made individually.
www.bakumedinfo.com
Signs of liquorodynamic disorders in children after one year
After one year, a child’s skull is already formed. The fontanelles have completely closed and the sutures have ossified. If there are liquorodynamic disturbances in a child, signs of increased intracranial pressure appear.
There may be such complaints:
- Headache.
- Apathy.
- Worry for no reason.
- Nausea.
- Vomiting, after which there is no relief.
The following signs are also characteristic:
- Gait and speech are impaired.
- There are disturbances in the coordination of movements.
- Vision decreases.
- Horizontal nystagmus.
- In advanced cases, “bobble doll head”.
And also, if liquorodynamic disorders of the brain progress, the following deviations will be noticeable:
- The child speaks poorly.
- They use standard, memorized phrases without understanding their meaning.
- Always in a good mood.
- Delayed sexual development.
- Convulsive syndrome develops.
- Obesity.
- Disturbances in the functioning of the endocrine system.
- Lag in the educational process.
ABOUT INTRACRANIAL PRESSURE IN A CHILD. TREATMENT.
We often hear the phrase “My child has ICP .” And this is a true statement - all living creatures on the planet that have a skull also have intracranial pressure. But what then worries parents of children?
The correct way to talk about the problem is increased intracranial pressure. Let’s make a reservation right away - this is not a diagnosis, but a description of one of the links in the development of many different diseases (that is, a symptom ). Intracranial pressure (ICP) increases with hydrocephalus, brain tumors, neuroinfections (encephalitis, meningitis), traumatic brain injury, intracranial hemorrhage, some rare hereditary diseases, etc.
Attention! If a child really has increased intracranial pressure, then he really needs medical help, since the question is about developmental disorders of the child in the future, and in some cases - even a threat to life!
Indirect signs of increased ICP are:
- — sleep and behavior disorders;
- - hyperactivity, attention deficit;
- — disorders of mental, speech and motor development, low learning ability;
- - “marble” skin pattern (including on the head);
- - nosebleeds;
- - “finger impressions” on a skull x-ray;
- - tremor (shaking) of the chin;
- - walking on tiptoes
The cause of the condition lies in the excessive accumulation of cerebrospinal fluid in the ventricles of the brain, where this fluid is produced, and the difficulty of its movement or absorption in the subarachnoid space.
Sometimes doctors give such children syndromic diagnoses: “hydrocephalic syndrome” , “increased intracranial pressure” , “dilatation of the ventricles of the brain” (symmetric or asymmetric), “Graefe’s symptom”, “setting sun syndrome”, “hypertensive-hydrocephalic syndrome”.
Associated symptoms are:
- non-overgrowth of fontanelles;
- drowsiness;
- noticeable squint;
- white stripe of the eyeball between the pupil and the upper eyelid;
- frequent and profuse regurgitation;
- the occurrence of seizures;
- involuntary shuddering of the whole body;
- the baby’s innate reflexes are too weak;
- decreased muscle tone;
- excessive enlargement of the skull ;
- nausea; vomit;
- dizziness;
- poor sleep;
- excessive tearfulness;
- developmental delay.
Reliable diagnostic methods for increased ICP are: ultrasound ( neurosonography ), CT and MRI of the brain.
TREATMENT OF HIGH ICP.
The choice of treatment methods depends on the severity of the disease.
Very severe forms ( hydrocephalus ) require surgical treatment with shunting to create an outflow of excess fluid. These are quite complex cases and osteopathic treatment can only be indicated after bypass surgery.
In less complex cases: traditionally, doctors prescribe diuretics, which remove fluid from everywhere, including the cerebrospinal fluid spaces. This is a nonspecific effect that is not aimed at the cause.
We set ourselves the task of normalizing the mechanisms of cerebrospinal fluid dynamics - the production and resorption of cerebrospinal fluid. This is work with the mobility of the bones of the base of the skull, which helps improve venous outflow, balance the tension of the dura mater, normalize the position and mobility of the cervical vertebrae, etc.
That is, we identify the root cause and act on it, restoring the normal physiology of the body.
Naturally, in the case of gross structural disorders, pharmacotherapy and, if necessary, surgical treatment are indicated. But if it is possible to restore normal mechanisms, this must be done.
It is important to understand that the solution to the problem does not need to be delayed or postponed, because the development of the syndrome can be prevented or reduced. It is necessary to consult a doctor - an osteopath already in the initial stages of the disease and almost always avoid serious consequences.
Diagnosis of the disease in adults
If you experience headaches and the symptoms described above, you should consult a neurologist. To clarify the diagnosis and prescribe treatment, the following studies may be prescribed:
- Computed tomography.
- Angiography.
- Pneumoencephalography.
- ECHO of the brain.
- NMRI.
If there is a suspicion of a syndrome of cerebrospinal fluid dynamics disorders, a lumbar puncture may be prescribed with a change in cerebrospinal fluid pressure.
When diagnosing adults, much attention is paid to the underlying disease.
Consequences of liquorodynamic disorders
If you do not treat this disease in time, then after a short time after the onset of symptoms, adverse consequences may appear:
- Among them, the most common are cognitive impairment and memory impairment. A person may forget about events that happened to him recently. The ability to perceive information and remember gradually decreases.
- Children who have liquorodynamic disorders begin to develop worse than their peers, both mentally and physically.
- Constantly disturbing headaches prevent a person from performing his work duties normally. In many ways, the changes described above occur due to impaired nutrition of the brain substance. All brain cells, and in particular the cortex, are very sensitive to a lack of oxygen, and with prolonged or constant deficiency, their atrophy begins to occur. That is why adult children with severe manifestations of liquorodynamic disorders are forced to receive a disability group.
Treatment of liquorodynamic disorders
The earlier the disease is detected, the greater the chance of restoring lost brain functions. The type of treatment is selected based on the presence of pathological changes in the course of the disease, as well as the age of the patient.
In the presence of increased intracranial pressure, diuretics are usually prescribed: Furosemide, Diacarb. Antibacterial agents are used in the treatment of infectious processes. Normalization of intracranial pressure and its treatment is the main task.
To relieve swelling and inflammation, glucocorticoid drugs are used: Prednisolone, Dexamethasone.
Steroid medications are also used to reduce cerebral edema. It is necessary to eliminate the cause of the disease.
As soon as liquorodynamic disturbances are detected, treatment should be prescribed immediately. After undergoing complex therapy, positive results are noticeable. This is especially important during the period of child development. Speech improves, progress in psychomotor development is noticeable.
Surgical treatment is also possible. It may be prescribed in the following cases:
- Drug treatment is ineffective.
- Liquorodynamic crisis.
- Occlusive hydrocephalus.
Surgical treatment is considered for each case of the disease separately, taking into account age, characteristics of the body and the course of the disease. In most cases, surgery on the brain is avoided so as not to damage healthy brain tissue, and complex drug treatment is used.
It is known that if the syndrome of liquorodynamic disorders in a child is not treated, the mortality rate is 50% up to 3 years, 20-30% of children survive to adulthood. After surgery, mortality is 5-15% of sick children.
Mortality increases due to late diagnosis.
Diagnosis of perinatal cerebral disorders in young children includes a comprehensive study of indicators of venous blood flow, ultrasound of brain structures in determining the characteristics of hemodynamic disorders in comparison with hemodynamic manifestations. In children, especially those born before the 34th week of gestation, it is necessary to regularly evaluate morphometric and functional parameters of the heart for early detection of abnormalities that may aggravate cerebral pathology.
The problem is not only prematurity
In full-term and premature newborns who have suffered severe asphyxia or have severe respiratory distress syndrome, a direct connection was noted between cerebral blood flow and changes in blood pressure, which was a phenomenon of impaired autoregulation. Due to the lack of regulation, cerebral blood flow passively follows changes in blood pressure, increasing the risk of developing ischemic lesions during hypotension and hemorrhage during episodes of increased blood pressure. For a more reliable assessment of the child’s condition, not absolute values of arterial blood flow velocities were used (due to their significant variability and dependence on a large number of external factors), but resistance indices, taking into account adjustment for gestational age.
Very premature babies experience neurological disorders. In addition, their further development, biological and social adaptation is influenced by a number of specific factors, including somatic chronic diseases, functional disorders, behavioral characteristics and impaired socialization in the family and society. Problems are associated not only with prematurity itself, but also with intensive care.
The quality of life of very premature infants may deteriorate due to surgical and somatic problems specific to them, chronic diseases, and rehospitalizations, which leads to daily activity, disruption of social and behavioral status. Deterioration in quality of life occurs in inverse proportion to birth weight. Upper respiratory tract infections, bronchial asthma, and ENT pathology aggravate the condition, aggravated by neurological deficit.
The level of physical development of a child is the main indicator of health. Premature children in the first year of life experience delays in weight and height indicators, as well as growth heterochrony.
Diagnosis of microcephaly (a decrease in head circumference by more than 2 standard deviations in accordance with age and gender) has demonstrated that the pathology is associated with a low rate of psychomotor development, a high incidence of cerebral palsy (CP), and delayed motor and mental development. Children with slow growth rates of head circumference had a significantly lower mental development index than healthy children.
The study of bioelectric activity (BEA) of the brain is carried out using electroencephalography (EEG). The BEA of the brain is formed in utero and by birth has the character of slow-wave activity with fragments of fast oscillations.
It is important to consider: when recording a certain pathological pattern using a traditional EEG, the ECG often overlaps, and interference from the operation of electrical devices can mask a gross suppression of activity in the inter-burst intervals.
Background characteristics of BEA (degree of intermittency, presence of cyclic variability of BEA, amplitude, correspondence of the degree of maturity of the general pattern of BEA to the child’s age from conception) have a high diagnostic value in assessing the severity of perinatal CNS lesions in newborns of different gestational ages.
The persistence of a pathological burst-suppression pattern is a marker of the severity of brain damage in full-term infants, the pathophysiological basis of which includes functional and/or structural disconnection of neuronal connections between the cortex and deep brain structures, such as the thalamus. In the works of neurophysiologist Karl Aso, one can see that a decrease in the amplitude of EEG activity is directly proportional to the prevalence of encephalomalacia, mainly in the cerebral cortex, corpus callosum, thalamus, midbrain and pons in postmortem examination of newborns. A pathological study showed a direct relationship between the number of damaged neurons and background aEEG activity in both full-term and premature infants.
Benefits of aEEG
Multichannel neonatal EEG involves recording BEA from scalp electrodes located above the main areas of the cerebral cortex. The technique makes it possible to assess the general and local characteristics of background BEA with a presumable topical diagnosis of one or more sources of pathological activity, to diagnose a delay or process of impaired maturation of the functional state of the central nervous system, and to objectively differentiate epileptic phenomena from paroxysmal conditions of non-convulsive origin.
When recording aEEG (amplitude-integrated electroencephalography), a very weak alternating current with a frequency of 400 Hz is applied to the scalp electrodes. This is necessary for monitoring the measurement of interelectrode impedance and monitoring the serviceability of signal transmission from the electrodes through the buffer amplifier to subsequent amplification stages. After amplification, the signal passes through a filter with a passband from 2 to 15 Hz, which minimizes artifacts from movements, sweating, myogram, ECG and possible interference from equipment in ICU conditions (artificial ventilation, infusion pumps, etc.).
The aEEG method accurately predicts outcome in 80% of children 3 hours after birth and in 90% of children after 6 hours of life. The combination of clinical assessment of neurological status with aEEG in the first 12 hours of life increases the accuracy of the forecast from 75% to 85%. When analyzing the relationship between the minimum aEEG amplitude, the Sarnat scale score and the presence of structural changes on MRI in full-term infants, the minimum amplitude showed the greatest predictive information. Its value of less than 4 μV in the first 72 hours after birth made it possible to predict the detection of subsequent structural abnormalities when performing MRI.
Ventriculomegaly diagnosed by the 40th week of postmenstrual age is a predictor of the development of cerebral palsy.
In very premature infants, early prediction of outcome using aEEG/EEG is much more difficult than in full-term infants who have suffered asphyxia. Perinatal outcome depends on the degree of prematurity and the spectrum of pathology of the perinatal period and is not always determined by the presence of primary cerebral damage.
It is necessary to clearly identify flashes on aEEG in the first 48 hours of life, which will be associated with predicting the outcome of peri- and intraventricular hemorrhage (PVH) up to grade 3–4 (about 130 flashes in 60 minutes increases the chances of survival, as well as favorable neurological forecast for 70–80%). Children with low densities of BEA outbreaks are statistically more likely to have fatal or severely disabling outcomes.
Seizure activity, which is recorded on aEEG in premature infants with extremely low body weight, very low body weight with grade 3-4 PVC, does not have a significant relationship with neurological outcomes.
An important aspect of assessing the functional state of the brain of newborns is the ontogenetic approach to the analysis of neonatal EEG. Dynamic changes in the BEA of the brain in newborns of different gestational ages fully reflect the morphological and functional development of the central nervous system in children in early ontogenesis.
Diagnostic features
To determine the predisposition of a newborn to the development of cerebral palsy, a comprehensive approach to assessing BEA is required.
In babies born before the 28th week of gestation, up to the 30–32nd week of postmenstrual age, BEA is represented by irregular, intermittent activity on the EEG. The final transition from intermittent to regular, continuous EEG activity ends at approximately 44–46 weeks of postmenstrual age.
In newborns with a short and extremely short gestation period (up to 30–32 weeks), it is almost impossible to distinguish the physiological stages of the sleep/wake cycle or their functional rudimentary nature exists. The sequential formation of physiological and electrographic patterns of the stages of the sleep/wake cycle begins around the 30th week, final differentiation is possible after the 36–37th week of postmenstrual age.
In the process of functional maturation of the central nervous system, there is an increase in the degree of interhemispheric synchronization of BEA rhythms, which reaches almost 100% by the 40–42nd week of postmental age.
The first outbreaks of oscillations of activity on the EEG can be recorded already in the fetus at the 22–23rd week of gestation. The dominant feature of the EEG of very premature newborns is the intermittent nature of background activity. When recording EEG, intervals of electrocerebral silence, or inter-flash inactive intervals, are noted, which are interrupted with some periodicity by bilateral discharges of high-amplitude slow waves with the inclusion of pointed elements and a small number of fast rhythms in the flash. Bursts of activity in newborns with an extremely short gestation period (up to 26 weeks) average from 1 to 5 s, but can reach 80 s, while the duration of interburst intervals of electrocerebral silence in these children does not exceed a minute.
A premature newborn is normally characterized by the presence of a trace discontinue - an intermittent curve. It must be remembered that rudimentary electrographic patterns of active sleep (REM) may be discernible in children at 25–26 weeks postmenstrual age. With increasing gestational age of newborns, the degree of interhemispheric synchronization of bilateral bursts in the trace discontinue composition progressively increases.
The first stage in premature infants, starting from approximately the 25–26th week of postmenstrual age, is the phylogenetically more ancient stage of active sleep, or REM stage of sleep. During this period, the EEG records regular, continuous activity. The appearance of these physiological and functional phenomena reflects the beginning of the formation of the active sleep stage.
According to the Prechtl principle
The assessment of the neurological status is based on the Prechtl principle of optimality, with optimal indicators of the neurological status of the newborn being assessed as 0, suboptimal indicators as different from 0. The neurological status of the newborn is assessed through the interaction of the processes of excitation and inhibition. An excess of excitation or a lack of inhibition is defined as a positive value, and an excess of inhibition or a lack of excitation is defined as a negative value. The methodology includes 7 scales: general activity with 5 bipolar and 2 unipolar positive subscales of special phenomena (convulsions-tremors), muscle tone, deep reflexes, newborn reflexes, autonomic, additional biochemical, additional neurophysiological. Then the profile of the newborn is determined by summing up the scores of the subscales and calculating the arithmetic mean for this scale. The total score for all subscales is also assessed and the total score for the scales is calculated.
Important for ultrasound
When ultrasound imaging is performed, it is necessary to take into account the increase in echo density of the periventricular zone above the density of the choroid plexus. Foci of infarction and necrosis of the periventricular white matter of the brain are noted at the level of the triangle of the lateral ventricles and the white matter of the frontal lobes; visualization of cysts at 2–4 weeks of life along the lateral or superior border of the lateral ventricle, location of cysts in the parietal and occipital regions of the brain. In some cases, complete, partial or isolated absence of the corpus callosum, signs of holoprosencephaly and hydrocephalus, calcification of the cortex, basal ganglia or periventricular region may be visualized.
Clinical case
Newborn girl weighing 1,600 g, height 43 cm. Head circumference - 31 cm, chest - 28 cm. Apgar score 5/6 points (2-1 (ventilator) -1-0-1 / 2-1 (ventilator) -1-1-1). From the 3rd pregnancy, occurring against the background of a disorder of fat metabolism of the 1st-2nd degree, arterial hypertension II risk 2, cyst of the right kidney, moderate myopia of both eyes in a period of 225 days.
Admission to OA&R for newborns
The condition is extremely serious. She was on a ventilator. Muscle tone and motor activity are reduced, adaptation reflexes are suppressed. Large fontanel - 2.0x2.0 cm, calm. The skin is pink, edema syndrome of the 2nd degree. Estimation of gestational maturity according to Petrussa 32 weeks.
Breathing is mechanical, symmetrically carried out on both sides, scattered wheezing is heard in moderate quantities. Heart sounds are rhythmic, somewhat muffled, no murmur can be heard. Heart rate 144–146 beats/min, blood pressure 52/31→59/37 mm Hg. Art. against the background of titration of dopamine 7.5 mcg/kg/min and norepinephrine 0.05 mcg/kg/min. Hydrocortisone was administered according to the schedule.
The abdomen is soft, palpable, peristalsis can be heard and is reduced. Liver +1 cm, spleen not palpable. Stool after cleansing enema, meconium. I urinated, the urine was light.
Hemodynamics were stabilized for 7 days by titrating dopamine 7.5→3 mcg/kg/min and norepinephrine 0.05 mcg/kg/min for 4 days. Blood pressure 59/37 - 69/44 mm Hg. Art., heart rate 146–160 beats/min.
The child is on mechanical ventilation, breathing is carried out symmetrically on both sides, with a gradual disappearance of wheezing by the 2nd day, SaO2 97%. Taking into account the data of the coagulogram and ultrasound of the brain, FFP O (I) Rh + was transfused to increase the coagulation potential of the blood on the 1st and 4th days of life.
The edema syndrome is dynamic with a decrease; from the 8th day of life there is no edema. There was no jaundice. From the first day of life, feeding with saline solution and switching to Pre-NAN 0 mixture, no residues were noted. From the 6th day of life she was switched to Pre-NAN mixture and absorbs it.
Survey
EEG No. 1–4 : low-amplitude EEG with signs of dyscirculatory disorders in the vascular areas of the brain.
Ultrasound of the brain No. 1: the lateral ventricles are symmetrical, the anterior horns are 3 mm on the right, 4 mm on the left. The cavities of the lateral ventricles are not dilated. The occipital horn is 13 mm on the right, 15 mm on the left. III ventricle 3 mm. Periventricular region: echogenicity is not increased. There is an increased amount of fluid between the gyri. The interhemispheric fissure is median, not widened, 3 mm. The subarachnoid space is not expanded. The pattern of convolutions and grooves is poorly differentiated.
Choroid plexuses: on the right the contours are smooth, the structure is homogeneous, on the left the contours are uneven, the structure is homogeneous. The cavity of the transparent partition is 8 mm. Verge's cavity 4 mm, large tank 6 mm. Optic tuberosities and basal ganglia: the echostructure is homogeneous, the echogenicity is slightly increased. In the area of the anterior horn of the left lateral ventricle, a heterogeneous hyperechoic formation 6x5 mm is visualized.
Doppler: PMA PS-13.2, PD -6.4, RI 0.52.
Conclusion: subependymal hemorrhage on the left, cerebral blood flow is slightly reduced.
Ultrasound of the brain No. 2–3: the interhemispheric sulcus is median. Intrathecal space 4 mm. The gyri and sulci are poorly differentiated. The anterior horns of the lateral ventricles are 4 mm on the right, 4 mm on the left. III ventricle 3 mm. Large tank 8 mm. In the area of projection of the lateral ventricles, hyperechoic formations are 7×4 mm on the left, 6×4 mm on the right.
ACA Doppler: PS-32.4, PD -11.3, RI 0.65 (N).
Conclusion : intraventricular hemorrhages (IVH) of the 1st–2nd degree on both sides.
Ultrasound of the brain No. 4
PMA Doppler: RI 0.72.
Conclusion: immaturity of brain structures. Stage 1–2 IVH on both sides.
Ultrasound of the brain No. 5 : the lateral ventricles are symmetrical, the anterior horns are 4 mm on the right, 4 mm on the left. The cavities of the lateral ventricles are not dilated. The occipital horn is 25 mm on the right, 24 mm on the left. III ventricle 5 mm. Periventricular region: increased echogenicity. The interhemispheric fissure is median, not widened. The subarachnoid space is not expanded. Subcortical zones: increased echogenicity. The pattern of convolutions and grooves is weakly expressed.
Choroid plexuses: on the right the contours are smooth, the structure is homogeneous, on the left the contours are uneven, the structure is heterogeneous. The cavity of the transparent partition is 8 mm. Verge's cavity 3 mm, large tank 10 mm. Optic tuberosities and basal ganglia: the echostructure is homogeneous, the echogenicity is slightly increased. In the area of the lateral ventricles there are hyperechoic formations on the right 6×4 mm, on the left 8×4 mm.
Conclusion: IVH of 1st-2nd degree on both sides. Marked immaturity of brain structures.
Ultrasound of the brain No. 6
Doppler: RI 0.65.
Conclusion: ventriculomegaly, IVH grade 1–2 on both sides.
Ultrasound of the brain No. 7: in the area of the projection of the lateral ventricles, hyperechoic formations are 7x4 mm on the left, 8x5 mm on the right.
Conclusion : no dynamics.
Ultrasound of the abdominal organs No. 1–2: without pathology.
RTG of chest and abdominal organs No. 1
OGK: the lungs are straightened, an increase in the pulmonary pattern is detected in the hilar regions on both sides. The mediastinum is median. Cor - N.
OBP: traces of gas in the stomach.
RTG of chest and abdominal organs No. 2
OGK: over all pulmonary fields, the shading is moderately intense with indistinct contours. The roots can be traced. The mediastinum is median. Cor - N.
Ophthalmologist No. 1: OU: calm, the corneas are swollen, the reflex from the fundus of the eye is dull, the fundus of the eye is not ophthalmoscopically visible due to swelling. Recommended: examination by a pediatric ophthalmologist.
Ophthalmologist No. 2: OU: calm, the corneas are clean, transparent, the fundus reflex is pink, the fundus corresponds to the gestational age. Recommended: examination by a pediatric ophthalmologist.
ECG: reduced voltage, sinus rhythm, heart rate 166–170 beats/min, EOS deviation to the right, disruption of repolarization processes in the myocardium.
Echo-KS: open oval window. Regurgitation on the MV of the 1st degree, on the TC of the 1st degree.
Diagnosis
Spastic diplegia. Cerebral palsy: early stage (?). Respiratory distress syndrome in a newborn at the stage of resolution and formation of bronchopulmonary dysplasia. Cerebral depression in the newborn. Stage 1–2 IVH on both sides. Prematurity 32 weeks. Intrauterine fetal hypoxia, first noted before birth. Moderate asphyxia at birth.
By the 6th month of life, the final diagnosis was made: cerebral palsy, spastic diplegia; cannula carrier.
Prevention of liquorodynamic disorders
Preventive measures include:
- Observation of pregnancy in the antenatal clinic. It is very important to register as early as possible.
- Timely detection of intrauterine infections and their treatment.
At 18-20 weeks, an ultrasound shows the development of the fetal brain and the state of the unborn child’s cerebrospinal fluid. At this time, it is possible to determine the presence or absence of pathologies.
- The right choice of delivery.
- Regular monitoring by a pediatrician. Measuring the circumference of the skull, if there is a need to conduct a fundus examination.
- If the fontanel does not close in a timely manner, it is necessary to conduct neurosonography and consult a neurosurgeon.
- Timely removal of tumors that block the cerebrospinal fluid pathways.
- Regular observation by a doctor and carrying out the necessary studies after suffering injuries to the brain and spinal cord.
- Timely treatment of infectious diseases.
- Prevention and therapy of chronic diseases.
- Quit smoking and alcohol.
- It is recommended to play sports and lead an active lifestyle.
It is easier to prevent any disease or take all measures to reduce the risk of developing pathology. If liquorodynamic disorders are diagnosed, then the earlier therapy is started, the greater the chance that the child will develop normally.
Liquorodynamic study of communicating syringomyelia
A.T. FAYZUTDINOVA1,2, I.M. MIKHAILOV3, E.I. BOGDANOV1,2
1Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, 420064, Kazan, Orenburgsky tract, 138
2Kazan State Medical University, 420012, Kazan, st. Butlerova, 49
3Kazan State Medical Academy, 420012, Kazan, st. Butlerova, 36
Fayzutdinova Aisylu Talgatovna - candidate of medical sciences, associate professor of the department of neurology and rehabilitation of KSMU, neurologist of the clinical expert department of the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, tel. +7-903-306-44-38, e-mail1,2
Mikhailov Igor Marsovich - Candidate of Medical Sciences, Associate Professor of the Department of Radiation Diagnostics, e-mail: [email protected]
Bogdanov Enver Ibragimovich - Doctor of Medical Sciences, Professor, Head of the Department of Neurology and Rehabilitation of KSMU, Head of the Neurological Clinic of the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, e-mail: [email protected] ,2
A clinical and magnetic resonance imaging CSF dynamic (using phase-contrast cine-MRI) examination of patients with communicating syringomyelia was carried out. The anatomical and dynamic components of liquorodynamic disorders that contribute to the formation of a communicating form of syringomyelia have been identified.
Key words: liquorodynamic studies, phase-contrast cine-MRI, communicating syringomyelia.
A.T. FAYZUTDINOVA1,2, I. M. MIKHAILOV3, E. I. BOGDANOV1,2
1Republican Clinical Hospital of the Ministry of Healthcare of the Republic of Tatarstan, 138 Orenburgskiy Trakt, Kazan, Russian Federation 420064
2Kazan State Medical University, 49 Butlerov St., Kazan, Russian Federation 420012
3Kazan State Medical Academy, 36 Butlerov St., Kazan, Russian Federation 420012
CSF circulation study of communicant syringomyelia
Fayzutdinova AT - Cand. Med. Sc., Associate Professor of the Department of Neurology and Rehabilitation, neurologist of the Clinical-Expertise Department, tel. +7-903-306-44-38, e-mail1,2
Mikhailov IM - Cand. Med. Sc., Associate Professor of the Department of Radiological Diagnostics, e-mail: [email protected]
Bogdanov EI - D. Med. Sc., Professor, Head of Neurological Clinic, Head of the Department of Neurology and Rehabilitation, e-mail: [email protected] ,2
The clinical and CSF circulation (by cine-PC MRI technique) study of communicant syringomyelia was performed. Anatomical and functional components of liquorodynamic changes were identified. These factors can be important for the communicant syringomyelia formation.
Key words : CSF circulation study, cine-PC MRI, communicant syringomyelia.
Syringomyelia (from the Greek syrinx - tube, canal and myelos - spinal cord) is a chronic polyetiological disease characterized by the progressive development of longitudinal cavities in the spinal cord, which are filled with cerebrospinal fluid or a liquid similar to it in composition. The classic “portrait” of syringomyelia includes insensitivity to pain and temperature influences in the area of the upper extremities and torso of the “jacket” or “half-jacket” type, while maintaining the sense of touch (tactile sensitivity) and deep sensitivity. The clinical picture is complemented by weakness and atrophy of the arms, as well as various bone deformities: scoliosis, short neck, large hands. The first description of the disease was given in 1824 by the French physician Olivier d'Angers. However, the pathogenesis of this process still remains unclear. The widespread introduction into practice of non-invasive neuroimaging methods, especially magnetic resonance imaging, has made it possible to diagnose syringomyelia at an early stage, and also opened up new prospects for studying its pathogenesis. It has been established that, firstly, syringomyelia is a secondary process; secondly, syringomyelia, regardless of its etiology, is usually based on disturbances in cerebrospinal fluid dynamics due to a block of the subarachnoid space at the level of the spinal cord or spinal canal; thirdly, the development of syringomyelia, in contrast to intramedullary postnecrotic non-progressive cystic formations, is a dynamic process: longitudinal edema of the spinal cord, referred to as “presyringus,” precedes cavity formation, and cessation of the cavity filling mechanism leads to its collapse [1, 2]. Modern systematization of cavities in syringomyelia includes the following forms of pathology: 1. Communicating syringomyelia (dilatation of the central canal communicating with the 4th ventricle) - 10%. 2. Non-communicating syringomyelia, including: a) central and paracentral cavities, b) primary parenchymal cavities. 3. Atrophic cavities (syringomyelia ex vacuo). 4. Neoplastic cavities. The range of etiological factors makes it possible to distinguish between syringomyelia associated with cranial factors and spinal factors. In most cases (up to 70%), syringomyelia is caused by congenital pathology at the level of the craniovertebral junction, mainly Chiari malformation type 1 (MC1). Currently, the prospects for studying spinal cavity formation are associated with the introduction of functional non-invasive liquorodynamic studies, including ultrasound and cine-MRI techniques [1, 2]. The purpose of this work was a clinical and magnetic resonance imaging (MRI) CSF dynamic examination of patients with communicating syringomyelia.
Materials and research methods
From the database of patients with syringomyelia, the results of examination of patients in whom MRI examination (1T) revealed the phenomenon of communication between the syringomyelic cavity and the 4th ventricle were selected (Fig. 1). A total of 7 patients were identified. All of them were included in the main group (MG) of the study. The first comparison group (NC) consisted of 7 patients with non-communicating syringomyelia, corresponding to the patients of the main group by gender, age, presence of concomitant ectopia of the cerebellar tonsils (n=4), number of radiotherapy sessions, history of surgical decompression of the PCF (n=1). The second comparison group (CG) consisted of 7 volunteers without CVP pathology, syringomyelia and severe organic symptoms, corresponding to the patients of the main group by gender and age. All subjects underwent clinical neurological, MRI morphometric and liquorodynamic (cine-PC MRI method [3, 4]) studies. The cine-PC MRI method was used to assess the presence of cerebrospinal fluid movement and spinal cord displacement, maximum systolic and diastolic flow velocities, and the duration of reaching the systolic peak velocity. The statistical significance of the identified differences was determined using the Student's test and the nonparametric paired Wilcoxon method; A level of p<0.05 was accepted as significant.
results
The results of the clinical neurological examination are presented in Table 1. The incidence of reported syringomyelia, according to our data, was 8.4%. A neurological examination did not reveal significant differences in the severity of clinical manifestations between the groups of patients with communicating and non-communicating syringomyelia, both at the time of examination and in relation to the initial symptoms of the disease. At the same time, the same severity of symptoms in combination with a shorter (on average 10 years) duration of clinical manifestations of the disease in the group of patients with communicating syringomyelia suggests a more severe course of this form of syringomyelia.
Table 1.
Results of clinical examination of patients
| Index | SG | NG | KG |
| 6/1 | 6/1 | 6/1 |
| 43±17 | 44±14 | 40±18 |
| 35±15 | 27±11 | — |
| 8±7 | 18±17 | — |
| 6 | 5 | — |
| — | 2 | — |
— decreased sensitivity in the hands, n | 2 | 2 | |
| - pain in the hands, n | 2 | 2 | |
| - pain in the back of the head or neck, n | 2 | 2 | |
| - other | 1 | 1 | |
- swallowing disorder | 2 | 1 | 0 |
| - visual impairment | 4 | 4 | 3 |
| - hearing impairment | 3 | 2 | 1 |
| - sensory impairment | 6 | 5 | 1 |
| - muscle weakness | 6 | 2 | 0 |
| - pain in the neck and arms | 3 | 4 | 0 |
| - headache | 3 | 5 | 2 |
| - dizziness, unsteadiness when walking | 4 | 2 | 2 |
| - pelvic disorders | 0 | 2 | 0 |
| average number of complaints*, ** | 3,4±1,9 | 3±1,5 | 1±1 |
- nystagmus | 3 | 2 | 0 |
| - bulbar disorders | 2 | 2 | 0 |
| - static-locomotor ataxia | 5 | 5 | 1 |
| - dynamic ataxia | 0 | 1 | 1 |
| - segmental-dissociated sensitivity disorders | 7 | 5 | 0 |
| - conduction sensitivity disorders | 0 | 1 | 0 |
| - atrophic paresis | 4 | 4 | 0 |
| - spastic paresis | 3 | 3 | 0 |
| — scoliosis | 3 | 3 | 0 |
| average number*, ** | 3±2,2 | 2,9±1,5 | 0,2±0,4 |
Note: * - differences between groups of patients with syringomyelia are not statistically significant (p> 0.05); ** - differences between patients with and without syringomyelia are statistically significant (p <0.05)
MRI morphometric study - results in Table 2. MRI study showed that patients with syringomyelia in general, compared with the group without syringomyelia, have a less deep posterior cranial fossa (PCF), a higher position of the odontoid process, a flattened base of the skull (large values of the NBO angle between the nasion, basion, occiput points) and a lower level of the cerebellar tonsils, consistent with the literature data [1, 2]. A feature of patients with non-communicating syringomyelia was a uniform expansion of the ventricular system (and the lateral and fourth ventricles), elongation of the intracranial space, a higher “crowding” index at the upper cervical level (the ratio of the axial area of the spinal cord with the cavity to the area of the spinal canal at the level of the CI vertebra) and “ overflow of the PCF with a sharpening of its upper angle (formed by the dorsum of the sella turcica, the upper point of the tentorium of the cerebellum and the internal occipital protuberance) and a decrease in the distance between the pontomedullary joint and the level of the foramen magnum (pm). Patients with communicating syringomyelia compared with non-communicating syringomyelia were distinguished by a higher position of the odontoid process, as well as dilation of the lateral ventricles of the brain in combination with normal sizes of the fourth ventricle. In addition, in patients with communicating syringomyelia, a significant narrowing of the cerebrospinal fluid ducts at the level of the posterior parts of the foramen magnum (c) and a decrease in the size of the cistern magna were revealed, which, according to [5], can lead to a decrease in the shock-absorbing capacity of the cistern magna and correlate with an increase in the pressure wave, spreading along the central canal of the spinal cord.
Table 2.
Results of MR morphometric study
| Index | SG | NG | KG |
| Length of intracranial space, mm (3) | 167±6 | 173±8 | 165±6 |
| Ramp length, mm (2, 3) | 39±4 | 38±3 | 45±5 |
| Claus index, mm (2, 3) | 32±3 | 33±8 | 41±5 |
| Height of the odontoid process above the Chamberlain line, mm (1, 2, 3) | 5±3 | 2±2 | -2±3 |
| Descent of the cerebellar tonsils below the foramen magnum, mm (2, 3) | 3±5 | 5±10 | -2,5±3 |
| Angle NBO, degrees (2, 3) | 177±6 | 175±6 | 166±8 |
| Upper angle of the HFA, degrees (3) | 107±10 | 101±11 | 112±10 |
| Index of the anterior horns of the lateral ventricles (2, 3) | 38±3 | 41±5 | 35±3 |
| Sagittal area of the 4th ventricle, mm2 (1*) | 75±31 | 130±101 | 85±29 |
| Sagittal area of the cistern magna, mm2 (2) | 75±58 | 151±139 | 197±80 |
| s, mm (1) | 1±2 | 3±3 | 6±5 |
| Index of “crowding” at the upper cervical level (1, 3) | 0,30±0,12 | 0,46±0,11 | 0,28±0,07 |
| pm, mm (3) | 16±4 | 13±5 | 17±2 |
Note: (1) - p<0.05 for groups with communicating and non-communicating syringomyelia (Student's t test); (2) — p<0.05 for groups with communicating syringomyelia and without syringomyelia (Student’s t test); (3) — p<0.05 for groups with non-communicating syringomyelia and without syringomyelia (Student’s t test); (1*) — p<0.05 for groups with communicating and non-communicating syringomyelia (Wilcoxon test)
Liquorodynamic ( cine- PC MRI) study. In all subjects examined at the level of the CI vertebra, biphasic systole-diastolic cerebrospinal fluid flows were detected in the anterior and posterior subarachnoid space (SAP) of the spinal canal. A significant displacement of the spinal cord at this level was detected in all patients with syringomyelia and only in two patients without syringomyelia (both with the lowest level of cerebellar tonsil location in their group). In the areas of the anterior subarachnoid space and spinal cord, the corresponding values of maximum systolic and diastolic flow velocities and the duration of reaching the systolic peak velocity (Table 3) did not differ significantly between groups. At the level of the posterior subarachnoid space, speed indicators did not differ between the groups with communicating syringomyelia and without syringomyelia, but significantly exceeded the corresponding values in the group with non-communicating syringomyelia. In patients with syringomyelia, systolic displacement of the spinal cord was ahead of systolic flow in the anterior subarachnoid space in 12 of 14 patients. The onset of systolic displacement in the posterior and anterior subarachnoid spaces coincided in groups with communicating syringomyelia and without syringomyelia, and in the group with non-communicating syringomyelia, systolic displacement in the posterior subarachnoid space began significantly earlier than in the anterior one, coinciding with the onset of spinal cord displacement.
Table 3.
Results of liquorodynamic study at the CI
| Index | SG | NG | KG |
| Maximum systolic velocity, cm/s: - anterior SAP | 1,56±0,53(3,5) | 1,36±0,74 (3) | 1,69±0,49 (5) |
| - rear SAP | 1,28±0,47(3,5) | 0,87±0,45 (2,3,5) | 1,78±0,92 (5) |
| - spinal cord | 0,32±0,10 (5) | 0,30±0,18 | — |
| Maximum diastolic velocity, cm/s: - anterior SAP | 1,04±0,52 (3) | 1,04±0,68 (3) | 0,96±0,32 |
| - rear SAP | 0,79±0,34 (3) | 0,43±0,29 (1,2,4) | 0,87±0,36 |
| - spinal cord | 0,16±0,08 | 0,24±0,17 | — |
| Duration of reaching the systolic peak velocity, ms: - anterior SAP | 131±27 (3) | 141±50 | 130±29 |
| - rear SAP | 120±37 | 180±165 | 112±28 |
| - spinal cord | 97±42 | 113±79 | — |
Note: (1) - p<0.05 for groups with communicating and non-communicating syringomyelia; (2) — p<0.05 for groups with non-communicating syringomyelia and without syringomyelia; (3) - p<0.05 for flow in the subarachnoid space and spinal cord displacement; (4) — p<0.05 for the anterior and posterior subarachnoid space; (5) - p<0.05 for systolic and diastolic flows in the same space
A number of intra-group patterns have been identified. In the group with communicating syringomyelia, diastolic velocity was lower than systolic (for the anterior and posterior subarachnoid spaces and for the spinal cord); the values of the maximum systolic and diastolic flow velocities and the duration of reaching the systolic peak velocity did not differ significantly in the anterior and posterior subarachnoid space, but were significantly higher compared to the corresponding indicators of the spinal cord. Similar patterns for the anterior and posterior subarachnoid spaces were observed in the group without syringomyelia. In patients with non-communicating syringomyelia, other dependencies have been noted. There was no difference between systolic and diastolic flow rates for either the anterior subarachnoid space or the spinal cord; the maximum diastolic flow velocity in the posterior subarachnoid space did not differ from the corresponding indicator in the spinal cord, but was significantly higher in the anterior subarachnoid space; The duration of reaching the systolic peak velocity did not differ significantly in the anterior and posterior subarachnoid space and in the spinal cord.
Thus, analysis of liquor dynamics at the level of the CI vertebra revealed less mobility of the spinal cord in patients without syringomyelia, as well as different liquor dynamics patterns for groups with communicating and non-communicating syringomyelia. A feature of patients with communicating syringomyelia were significant differences between systolic and diastolic flow rates, as well as between liquorodynamic parameters of the subarachnoid space and spinal cord. In the group of patients with noncommunicating syringomyelia, there were no velocity differences between diastolic spinal cord displacement and CSF flow in the posterior subarachnoid space. A liquorodynamic study showed the comparability of our results with the literature data, for example, on the absolute values of speed indicators in healthy individuals and on greater mobility of the spinal cord in patients with Chiari malformation type 1 [6], on higher values of flow velocity in the anterior subarachnoid space compared to posterior in patients with Chiari malformation type 1 [7].
Analysis of intracavitary cerebrospinal fluid flows. In the group of patients with communicating syringomyelia, fluid flow inside the syringomyelitic cavity at the level below the obex was detected in three patients, at the level of the CI vertebra - in 5 patients. Both patients, in whom intracavitary flows were not detected, did not have Chiari malformation type 1: a morphometric study revealed a high position of the odontoid process in one patient, and a Chiari malformation 0 in the second. At the level of the widest part of the syringomyelitic cavity, cerebrospinal fluid flows were recorded in five patients with communicating syringomyelia and four with non-communicating syringomyelia (Table 4). The duration of systole of intracavitary flow in the group with communicating syringomyelia was significantly higher than the corresponding indicator in the group with non-communicating syringomyelia.
Table 4.
Results of a liquorodynamic study of intracavitary cerebrospinal fluid flows in patients with communicating and non-communicating syringomyelia
| Communicating syringomyelia | ||||||||
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | М±m |
| Localization of the cavity | Up to C4 | Up to Th3 | Up to C6 | Up to Th2 | Up to C6 | Holocord | Up to C6 | |
| Measurement level | S2-3 | C6 | C2 | C2 | C3 | C4 | C3 | |
| Maximum systolic velocity, cm/s | 0,44 | 3,78 | — | — | 0,72 | 3,61 | 0,12 | 1,73±1,80 |
| Maximum diastolic velocity, cm/s | 0,43 | 2,48 | — | — | 0,69 | 2,1 | 0,1 | 1,14±1,08 |
| Duration of reaching the systolic peak velocity, ms | 179 | 72 | — | — | 232 | 118 | 265 | 173±79 |
| Duration of systole, ms | 270 | 235 | — | — | 384 | 519 | 530 | 388±137* |
| Diastole duration, ms | 443 | 470 | — | — | 538 | 612 | 378 | 488±90 |
| Noncommunicating syringomyelia | ||||||||
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | М±m |
| Localization of the cavity | С1-Th8 | C2-Th1 | C2-C6 | C2-Th6 | C1-Th4 | C1-Th9 | C2-7 | |
| Measurement level | C6 | C3 | C3 | C3 | C3-4 | C4 | C4-5 | |
| Maximum systolic velocity, cm/s | 1,18 | — | — | — | 0,44 | 1,27 | 0,8 | 0,92±0,38 |
| Maximum diastolic velocity, cm/s | 2,03 | — | — | — | 0,48 | 1,02 | 0,79 | 1,08±0,67 |
| Duration of reaching the systolic peak velocity, ms | 42 | — | — | — | 135 | 63 | 136 | 94±49 |
| Duration of systole, ms | 167 | — | — | — | 325 | 204 | 305 | 250±77 |
| Diastole duration, ms | 498 | — | — | — | 978 | 407 | 505 | 597±258 |
Note: * - differences between groups are statistically significant (p<0.05)
Drawing.
Sagittal MRI of patients with communicating syringomyelia
Discussion
The communicating form of syringomyelia is a rare variant of the disease, the mechanism of development of which, according to Gardner’s CSF-dynamic “water hammer” theory, is associated with obstruction of the CSF pathways at the level of the exit from the fourth ventricle with an increase in pressure in it and the pushing of cerebrospinal fluid through the obex into the central canal of the spinal cord [8 , 9]. In the literature, there are isolated observations of communicating syringomyelia with liquorodynamic confirmation of this theory [10, 11]. The main causes of communicating syringomyelia are hydrocephalus that develops after cerebral hemorrhage or meningitis, Chiari 2 malformation, encephalocele and Dandy-Walker anomaly. In our observation, communicating syringomyelia was predominantly combined with Chiari malformation type 1 or with a high position of the odontoid process; in addition, almost all patients noted the connection between the onset of clinical manifestations of the disease and injuries or physical overload. Another feature identified in our group of patients was the absence of dilatation of the fourth ventricle, which probably excludes stenoses at the level of the foramina of Luschka and Magendie and suggests a different pathogenesis of the disease.
Thus, communicating syringomyelia is a pathogenetically heterogeneous variant of syringomyelia, the determination of the mechanism of formation of which requires the use of MRI liquorodynamic and MRI morphometric studies. Analysis of the data obtained allowed us to identify the structural anatomical and dynamic functional components of liquorodynamic disorders that can contribute to the formation of a communicating form of syringomyelia. Patients with communicating syringomyelia were distinguished by a significant narrowing of the cerebrospinal fluid ducts at the level of the posterior parts of the foramen magnum and a decrease in the size of the cistern magna, as well as significant speed differences between the diastolic displacement of the spinal cord and the flow of cerebrospinal fluid in the posterior subarachnoid space. In addition, the duration of systole of intracavitary flow in the group with communicating syringomyelia was significantly higher than the corresponding indicator in the group with non-communicating syringomyelia.
LITERATURE
1. Bogdanov E.I. Syringomyelia // Neurological Journal. - 2005. - No. 6. - P. 4-11.
2. Syringomyelia. A Disorder of CSF Circulation / Ed. by G. Flint, C. Rusbridge. — Springer-Verlag Berlin Heidelberg, 2014. — 345 p.
3. Badelia RA, Bogdan AR, Wolpert SM Analysis of cerebrospinal fluid flow wave-forms with gated phase-contrast MR velocity measurements // AJNR. - 1995. - Vol. 16. - P. 389-400.
4. Brugie`res P., Idy-Peretti I., Iffenecker C. et al. CSF Flow Measurement in Syringomyelia // Am. J. Neuroradiology. - 2000. - Vol. 21. - P. 1785-1792.
5. Chang HS, Nakagawa H. Hypothesis on the pathophysiology of syringomyelia based on simulation of cerebrospinal fluid dynamics // JNNP. - 2003. - Vol. 74. - P. 344-347.
6. Hofmann E., Warmuth-Metz M., Bendszus M., Solymosi L. Phase-contrast MR imaging of the cervical CSF and spinal cord: volumetric motion analysis in patients with Chiari I malformation // AJNR. - 2000. - Vol. 21. - P. 151-158.
7. Iskandar BJ, Quigley M., Haughton VM Foramen magnum cerebrospinal fluid flow characteristics in children with Chiari I malformation before and after craniocervical decompression // J. Neurosurg. (Pediatrics 2). - 2001. - Vol. 101. - P. 169-178.
8. Gardner WJ, Angel J. The mechanism of syringomyelia and its surgical correction // Clin. Neurosurg. - 1959. - Vol. 6. - P. 131-140.
9. Pamir MN, Özer AF, Zirh TA et al. CT myelography in communicating syringomyelia // Eur. J. Radiology. - 1991. - Vol. 12. - P. 47-52.
10. Kohli A., Gupta RK Neurological picture. Gardner's hypothesis and magnetic reso-nance imaging // JNNP. - 1997. - Vol. 63. - P.143.
11. Kawaguchi T., Fujimura M., Tominaga T. Syringomyelia with obstructive hydroceph-alus at the foramens of Lushka and Magendie successfully treated by endoscopic third ventriculostomy // Surgical Neurology. - 2009. - Vol. 71(3). — P. 349-352.
REFERENCES
1. Bogdanov EI Siringomieliya. Nevrologicheskiy zhurnal, 2005, no. 6, pp. 4-11 (in Russ.).
2. Syringomyelia. A Disorder of CSF Circulation. Ed. by G. Flint, C. Rusbridge. Springer-Verlag Berlin Heidelberg, 2014. 345 p.
3. Badelia RA, Bogdan AR, Wolpert SM Analysis of cerebrospinal fluid flow wave-forms with gated phase-contrast MR velocity measurements. AJNR, 1995, vol. 16, pp. 389-400.
4. Brugie`res P., Idy-Peretti I., Iffenecker C. et al. CSF Flow Measurement in Syringomyelia. Am. J. Neuroradiology, 2000, vol. 21, pp. 1785-1792.
5. Chang HS, Nakagawa H. Hypothesis on the pathophysiology of syringomyelia based on simulation of cerebrospinal fluid dynamics. JNNP, 2003, vol. 74, pp. 344-347.
6. Hofmann E., Warmuth-Metz M., Bendszus M., Solymosi L. Phase-contrast MR imaging of the cervical CSF and spinal cord: volumetric motion analysis in patients with Chiari I malformation. AJNR, 2000, vol. 21, pp. 151-158.
7. Iskandar BJ, Quigley M., Haughton VM Foramen magnum cerebrospinal fluid flow characteristics in children with Chiari I malformation before and after craniocervical decompression. J. Neurosurg. (Pediatrics 2), 2001, vol. 101, pp. 169-178.
8. Gardner WJ, Angel J. The mechanism of syringomyelia and its surgical correction. Clin. Neurosurg., 1959, vol. 6, pp. 131-140.
9. Pamir MN, Özer AF, Zirh TA et al. CT myelography in communicating syringomyelia. Eur. J. Radiology, 1991, vol. 12, pp. 47-52.
10. Kohli A., Gupta RK Neurological picture. Gardner's hypothesis and magnetic reso-nance imaging. JNNP, 1997, vol. 63, p.143.
11. Kawaguchi T., Fujimura M., Tominaga T. Syringomyelia with obstructive hydroceph-alus at the foramens of Lushka and Magendie successfully treated by endoscopic third ventriculostomy. Surgical Neurology, 2009, vol. 71 (3), pp. 349-352.