3 January 2021
28849
0
4.1 out of 5
Spinal injuries today, unfortunately, are far from uncommon. They account for 5.5% to 17.8% of all cases of injuries to the musculoskeletal system. Neither children, nor adults, nor especially the elderly are insured against them. And the consequences of such accidents, especially those leading to spinal cord damage, can be extremely severe, including disability and death, especially if the victim does not receive qualified medical care in the first hours after the incident. Only in the mildest cases or with timely surgery, spinal injuries go away without a trace and are not associated with the risk of complications. Therefore, they always require the fastest possible response and contact a neurosurgeon or spinal surgeon.
Types of spinal injuries
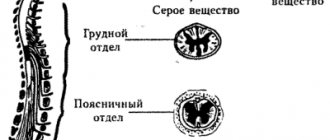
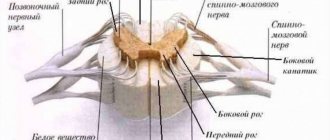
In general, the spine consists of 33 vertebrae, between which are located cartilaginous plates (intervertebral discs). Almost all vertebrae have a bony arch and processes extending from it. A hole is formed between the vertebral body and the arch, the position of which coincides in each spinal motion segment throughout the entire spinal column. The canal formed in this way is called the spinal canal, in which the delicate nervous structure - the spinal cord - is located. A pair of nerve roots depart from it at the level of each vertebra, which together are responsible for the innervation of the entire body.
Each of these anatomical structures can be injured. As a result, they distinguish:
- spinal bruises are the mildest injuries in which mechanical injury to soft tissues is observed, but the integrity of bone structures, intervertebral discs and ligaments is not compromised;
- fractures of the vertebral bodies - can be compression, in which the vertebra is flattened on one side, or comminuted, in which individual bone fragments are formed;
- fractures of the processes and/or arches of the vertebrae;
- vertebral dislocations - a change in the position of the bones that form the joints of the spine (sometimes the dislocation can be self-correcting);
- fracture-dislocations of the vertebrae;
- spondylolisthesis – displacement of the upper vertebral body anteriorly relative to the lower one, which also leads to sprained ligaments;
- partial or complete rupture of the ligaments of the spinal motion segment (distortion) - a minor injury, usually with a favorable outcome;
- intervertebral disc rupture – instantaneous formation of a disc herniation under the influence of a traumatic factor;
- spinal cord concussion – a change in the condition of the spinal cord that is reversible over time;
- contusion of the spinal cord and/or its roots - with rapid restoration of blood flow and elimination of compression, the consequences can be reversible;
- partial or complete rupture of the spinal cord and/or its roots is the main cause of disability.
All these types of damage can be combined with each other in different combinations, so 3 types of spinal injuries can be distinguished:
- uncomplicated spinal injury – accompanied by a violation of the integrity of the spinal structures without affecting the spinal cord;
- spinal cord injury without damage to the spine - consists of damage to the spinal cord;
- spinal cord injury – accompanied by a combination of damage to the spinal column, spinal cord and neurovascular formations of the spinal canal.
In 40-60% of patients with spinal cord injury, damage to internal organs and other tissues is observed.
Like other injuries, spinal injury, depending on the nature of the violation of the integrity of the skin, can be closed, open or penetrating. It is very important to determine exactly how much time has passed since the injury. Depending on this, 5 periods are distinguished:
- acute – up to 8 hours;
- acute – 8-72 hours;
- early – from 3 days to 4 weeks;
- intermediate – 1-3 months;
- late – more than 3 months.
All spinal injuries can be divided into stable and unstable, which largely influences the nature of the necessary treatment.
Accurately determining the type of injury and the period in which the patient is currently in is extremely important for the correct development of treatment tactics. Therefore, after providing emergency care to a patient, a comprehensive diagnosis is always carried out.
Causes
Spinal injury is usually caused by the application of an external force. Most often it occurs as a result of:
- falls from a height, which is called catatrauma – 50%;
- road traffic accidents – 30%;
- diving head down in shallow water – 10%.
This is often accompanied by damage to the spinal cord, i.e., a spinal cord injury initially occurs. In such situations, the spinal cord suffers due to instant or gradually increasing compression by bone structures, displacement of the vertebrae in an unstable segment of the spine. It can also be stretched and ruptured, which leads to disability.
The spinal cord is a sensitive anatomical structure that can also be damaged, even if initially only the spine was damaged at the time of injury. In such situations, spinal cord injury is secondary and becomes a consequence of impaired microcirculation, severe swelling of the surrounding soft tissues, hypoxia (lack of oxygen), disturbances in electrolyte metabolism and the action of a number of other factors.
However, the situation is extremely serious in both cases, regardless of whether primary or secondary spinal cord injury occurs.
Less commonly, the cause of spinal injury, namely vertebral compression fracture, is osteoporosis. This disease is most common in older people, although it can also occur at a young age without long-term use of corticosteroids and some other drugs. It is characterized by a decrease in bone density, which leads to the fact that the vertebral bodies become more fragile and can flatten, forming a wedge-shaped deformity, even as a result of a sudden movement, coughing, not to mention a fall or blow.
Other causes of spinal injury without significant external influence may be tumors of the spine itself or the formation of metastases in it.
Spinal cord injury
Sometimes a spinal injury extends to the spinal cord. This may be due to external factors such as a severe contusion or a compression fracture of the cervical spine, although the injury can occur in any part of the spine.
The following signs usually indicate a spinal cord injury:
- numbness or tingling in the limbs;
- pain and stiffness in the spine;
- signs of shock;
- inability to move limbs;
- loss of urinary control;
- loss of consciousness;
- unnatural head position.
Spinal problems are often the result of accidents or violent acts. Main causes of injuries:
- a fall;
- diving in shallow water (consequences of hitting your head on the bottom of a reservoir);
- trauma after a car accident;
- jumping;
- head injury during a sporting event;
- electric shock injuries.
Symptoms
The main manifestations of spinal injury are pain and a burning sensation, swelling, and redness at the site of injury. A hematoma or even an open wound may also be observed. But the clinical picture largely depends on the level of damage and its severity. Thus, cervical spine injuries are characterized by:
- impaired sensitivity and mobility of the hands up to complete paralysis (tetraplegia);
- difficulty turning your head;
- respiratory failure, shortness of breath, respiratory arrest.
Injuries to the cervical spine are the most dangerous in terms of disability and death.
Damage at the level of the thoracic and lumbar vertebrae may be accompanied by:
- decreased or loss of sensation in the legs;
- disorders of urination and defecation;
- inability to raise a straight leg while lying on your back;
- back muscle tension.
Thus, a high risk of injury is indicated by the appearance of disturbances in sensitivity and motor functions.
Closed reduction
This method is used for dislocations of the cervical spine. The principle of this method is to use heavy weights for traction so that a slow maneuver can be performed to reduce the spine. This is a completely safe method. Neurological deterioration during reduction is a risk that is extremely rare, especially if the reduction is carried out carefully.
This method requires the installation of Crutchfield or Gardner-Wells traction forceps.
Unconscious patients should undergo an MRI scan before reduction.
Reduction is not performed for injuries such as craniocervical dissociation or cervical spine injury with signs of distraction.
Advantages of closed reduction
- Reduces the need for complex surgical procedures
- Improves stability, prevents neurological deterioration, or may improve neurological status
- Reduction in the first few hours of injury can lead to significant improvement in neurological status.
But there is no effective closed reduction method for the thoracolumbar spine yet.
Diagnostics
Diagnosis of spinal injury is always complex, since the slightest omission can have catastrophic consequences. Therefore, the spine is always carefully examined using various research methods.
Initially, a survey is carried out of the victim himself or the person who witnessed the incident that allegedly led to a spinal injury. The main emphasis is on elucidating the mechanism of its production and timing. If the patient is conscious and able to answer questions, they try to find out where the pain is felt and whether sensory or motor disorders are observed, and if so, when they arose.
The further diagnostic algorithm is as follows:
- examination using palpation methods;
- assessment of neurological condition;
- carrying out instrumental diagnostic procedures.
It is also necessary to immediately draw blood for general and biochemical analysis. In addition, it is necessary to perform a general urine test.
Patient examination
As part of the physical examination, it is possible to establish the approximate location of the injury, detect visible deformations and find out which levels of the spine should be examined using X-rays in order to exclude the presence of combined injuries. Therefore, palpation and examination is carried out throughout the patient’s body, but with great care to avoid causing additional damage to the patient.
Determination of neurological status
The degree of sensitivity and preservation of motor functions must also be assessed. In this case, the international ASIA scale is used, which implies 5 degrees of spinal cord injury (A, B, C, D, E), of which A is the most severe injury, accompanied by a complete absence of motor and sensory functions, and E is the norm.
When determining neurological status, attention is paid to:
- muscle strength;
- sensitivity to pain and touch (tested by touching with cotton wool or a special caliper-like instrument called Frey hairs);
- reflex activity in the anogenital area.
Additional information about the patient’s condition can be provided by a test in which passive movements of the fingers or toes are performed, depending on the level of the lesion.
Instrumental diagnostics
The use of special diagnostic equipment allows you to obtain the most accurate information about the patient’s condition, determine the specific level of damage, the degree of spinal cord injury, assess the nature of changes in the condition of the spine, determine the presence of instability and obtain a lot of other data important for selecting the optimal treatment method. Based on them, a decision is made on the need for surgical intervention, as well as the type of operation required and its volume, or the possibility of conservative treatment.
Thus, when diagnosing spinal injuries, the following are carried out:
- X-ray is an outdated method, which is now being abandoned in favor of CT, since X-rays are not always able to detect all existing bone damage and accurately determine the type of fracture.
- Computed tomography (CT) is the main method for diagnosing fractures and dislocations, providing the most complete and accurate information about the state of the bone structures of the spine and not requiring additional movements of the patient on the couch. With its help, you can detect fractures of vertebral bodies, arches and processes, accurately determine the length of fracture lines, assess the degree of divergence of bone fragments, detect displaced fragments, etc.
- Magnetic resonance imaging (MRI) is the most informative study that allows you to accurately assess the condition of the spinal cord, intervertebral discs, ligaments, the presence of hematomas and soft tissue formations in general.
- Myelography is an additional research method used in the presence of neurological disorders, but it is impossible to detect their causes on CT. Using myelography, the presence of a violation of the patency of the subarachnoid space in the spinal cord is determined and it is revealed at what level the deformation occurred, leading to compression of the spinal cord or rupture of its dura mater.
First aid for spinal injury and choice of treatment tactics
It is important not to move or lift the patient after receiving a blow or other traumatic impact and immediately call an ambulance. Under no circumstances should the victim be allowed to sit or stand, but it is worth giving pain medication and attempting to calm him down. If there is no breathing or heartbeat, resuscitation should be performed. Specialists who arrive at the scene carefully immobilize the patient at the scene by securely fixing him on a rigid shield using a rigid head holder, and then transport him to a medical facility.
Any patient who is suspected of having a spinal injury is immediately treated with a spinal injury protocol until a full investigation has been completed and it is proven that no injury has occurred.
If the presence of an injury is confirmed, its type and characteristics are clarified, it becomes clearly clear what treatment is indicated in a particular case. Conservative therapy is carried out only in the mildest cases in the absence of signs of neurological deficit, when only a violation of the anatomy of bone structures is observed without signs and risks of complications, in particular compression of the spinal cord. It is usually indicated for mild compression fractures, dislocations, fractures of processes, arches, and vertebral bodies without the formation of fragments.
Conservative treatment consists of:
- bed rest or immobilization of the affected part of the spine;
- drug therapy appropriate to the situation;
- traction therapy (spinal traction using a special apparatus);
- physiotherapy;
- manual therapy.
If necessary, vertebral reduction is initially performed.
But in the vast majority of cases, surgery is indicated for spinal injuries. Emergency surgery is required when:
- the presence and especially intensification of signs of neurological deficit;
- severe deformation of the spinal canal due to bone fragments, dislocated vertebrae or significant curvature;
- the presence of a large hematoma formed as a result of injury to a herniated intervertebral disc, injury to the yellow ligament, the presence of a foreign body that threatens compression of the spinal cord;
- the presence of isolated hematomyelia, i.e. hemorrhage in the spinal cord;
- compression of a large blood vessel supplying the spinal cord;
- pronounced compression of the spinal roots;
- instability of spinal motion segments when creating a threat of their displacement and compression of the spinal cord;
- the presence of foreign bodies in the spine;
- liquorrhea, i.e. leakage of cerebrospinal fluid through defects at the base of the skull;
- injuries received from gunshot or stab wounds.
But there are also contraindications for performing the operation even if there are compelling indications for it. In such situations, spinal surgery is postponed until the patient's condition is stabilized. This is about:
- traumatic or hemorrhagic shock with unstable hemodynamics;
- the presence of severe damage to internal organs, leading to internal bleeding, associated with the risk of developing peritonitis;
- extremely severe traumatic brain injuries with signs of intracranial hematoma formation.
However, it is also possible to carry out the operation as planned. They are required when conservative therapy is ineffective, but they allow you to carefully prepare the patient for the upcoming surgical intervention and select a treatment tactic that suits him.
Prevention
Unfortunately, spine and spinal cord injuries are unpredictable, but the risk of injury can be greatly reduced by following simple safety precautions.
- You should always wear a seat belt while riding in a car.
- When playing sports, you must wear appropriate protective equipment.
- Do not dive in unfamiliar bodies of water
- Strengthen the muscular system to provide proper support to the spine.
- Do not drink alcohol while driving.
Surgery for spinal injury
The goals of surgical treatment are:
- rapid and complete elimination of the factor leading to compression of the spinal cord and other neurovascular formations;
- restoration of the correct axis of the spine;
- fixation and stabilization of the spine, which will allow the patient to be activated as early as possible and avoid deformation in the future.
If there are signs of spinal cord damage, it is recommended to perform surgery as early as possible, since up to 70% of cases of the development of all irreversible changes occur in the first hours after injury. But there are quite a few types of operations that can be indicated for spinal injuries. The choice of a specific one is made by the neurosurgeon in each case individually.
Halotraction
Halotraction is an operation indicated for complicated or unstable injuries of the cervical spine. It involves dynamic reposition and reliable fixation of the vertebrae while maintaining the patient’s physiological activity using a special halo apparatus.
It is a device, part of which reliably connects the damaged vertebrae to the base of the skull, and the other is located outside the body. Its design features make it possible to gradually perform traction, i.e. stretching of damaged spinal motion segments until complete reposition of the vertebrae is achieved.
On average, the halo apparatus is removed after 2.5-3 months. After this, the use of a head holder is prescribed for 3-4 weeks.
Laminectomy
Laminectomy is a decompression operation widely used for various spinal injuries. It allows you to eliminate compression of the spinal cord and its roots by various anatomical structures by removing the vertebral arches or only their processes, or to provide access to the spinal cord to remove foreign bodies or perform other manipulations on it.
Often the situation requires a discectomy, i.e., removal of the intervertebral disc, and in some cases the surgeon is forced to remove the entire damaged vertebra completely, i.e., perform a corpectomy.
Laminectomy requires further installation of stabilizing systems in order to achieve spinal fusion.
Discectomy
Discectomy is a decompression operation indicated for traumatic injuries of the intervertebral disc that have led to compression of the spinal roots or spinal cord. It involves removing the damaged intervertebral disc and can be combined with laminectomy.
The operation is performed through an anterolateral approach (for injuries to the cervical spine) or posterior (for damage to the thoracic or lumbosacral discs). It is performed under general anesthesia, and the removed disc is replaced with a bone graft, synthetic implant, or spinal fusion is achieved.
In cases uncomplicated by serious spinal cord injuries, microdiscectomy may be performed. This operation involves making a much smaller incision and may involve removing only a formed hernia while preserving the disc. Endoscopic surgery can also be an alternative, but spinal injuries are rarely limited to isolated disc damage, so discectomy is often only one of the stages of surgical intervention.
Spinal fusion
Spondylodesis is an operation whose main goal is the reliable fusion of several spinal motion segments with each other, which leads to their complete immobilization, and therefore eliminating the risk of displacement and subsequent injury to the spinal cord. For this purpose, a fragment of the patient’s own bone (autograft) or artificial bone can be used. But more often special titanium structures are used, i.e., transpedicular fixation of the vertebrae is performed, since this technique is associated with fewer risks and is more reliable.
Transpedicular fixation involves a strong connection of adjacent vertebrae using special screws and rods passed through their heads. Titanium screws are screwed into the intersection of the transverse process of the vertebra with the superior articular process. In this case, it is necessary to fix at least 3 vertebrae, even if only one of them is affected, since otherwise the proper degree of stabilization of the spine will not be achieved.
The transpedicular fixation method is the main way to achieve stabilization of the spinal column in various spinal injuries.
Spinal fusion can be performed in isolation or as one of the stages of surgical treatment of spinal injury, for example, after decompression of the spinal cord or its roots. The operation may also involve removal of the intervertebral disc, which is especially important in case of traumatic damage. In this case, a modern, precisely sized cage is installed in place of the removed disc.
If initial decompression of spinal structures is necessary, this task can be solved through an anterior or posterior approach. Most often, the operation is performed through a posterior approach, since this is associated with lower intraoperative risks and is less likely to lead to postoperative complications.
Vertebroplasty and kyphoplasty
Vertebroplasty and kyphoplasty are two similar techniques that can be used for vertebral compression fractures. Their essence is to restore the strength of a broken vertebral body using specially developed, quickly hardening bone cement.
Both operations are minimally invasive and involve the introduction of a thin cannula into the body of a broken vertebra, through which its integrity will be restored by injecting freshly mixed bone cement into it. It will fill all natural bone pores and provide high strength to the vertebra within 10 minutes, since this is exactly the time it takes for it to completely harden.
But when choosing kyphoplasty, a special balloon is first inserted into the vertebral body through the same cannula and filled with liquid. As a result, it swells and helps restore the anatomy of the fractured vertebral body. After this, the balloon is deflated and removed, and the resulting space and the entire vertebral body are filled with bone cement. Once it has hardened, the cannula is removed and the remaining puncture is covered with a sterile bandage.
The features of these two percutaneous surgery techniques determine the specifics of their application. Thus, vertebroplasty is indicated for mild compression fractures, when the height of the vertebral body decreases by less than 70%. At the same time, kyphoplasty has wider possibilities, so it can be used for severe compression fractures with a decrease in vertebral height by more than 70%.
Thus, no one is immune from spinal injury. But if it happens, it is important not to try to cope with the situation on your own, but to immediately call an ambulance, ensuring the victim is completely immobile. The prognosis of a spinal injury largely depends on both its type and the speed of receiving qualified medical care. In mild, uncomplicated cases, complete recovery usually occurs, but if the spinal cord is damaged, there is a high risk of complications, including loss of control over urination and defecation, and disability.
SPINAL CORD INJURYInjury to the spine and spinal cord occurs much less frequently than brain injury and in peacetime accounts for 1-4% of the total injury rate. In most cases this is an indirect injury. The most common cause is a fall from a height onto the buttocks, back, head, compression of the bent torso during landslides, hitting the head on the bottom when jumping into water, etc.
Spinal cord injury is divided into open (with violation of the integrity of the skin at the site of injury) and closed (without violation of the integrity of the skin), the latter making up the majority of injuries of this kind. In relation to the spinal cord, injuries are divided into three groups: spinal injury without impairment of spinal cord function; spinal injury with dysfunction of the spinal cord; damage to the spinal cord without damage to the spine.
According to the nature of the spinal cord injury, there are: concussion, contusion, compression, crushing of the spinal cord with partial or complete interruption, hematomyelia and traumatic radiculitis. Severe injury to the spinal cord and its elements occurs with a fracture, dislocation and fracture-dislocation. The XII thoracic, I-II lumbar and V-VI cervical vertebrae are most often damaged. As a rule, one vertebra is damaged, less often two, and very rarely three or more. The most common fracture of the vertebral body occurs; fragments can protrude into the lumen of the spinal canal, causing compression of the spinal cord. With a compression fracture of the vertebral body, compression occurs with an Urban wedge - a wedge-shaped bone fragment. Damage to the spinal cord can also occur when a vertebral arch is fractured.
Spinal injuries without spinal cord injury are more common. They do not pose a great danger to life and with proper treatment, complete recovery occurs.
Neurosurgical treatment includes spinal injuries associated with spinal cord damage. They are among the most severe and prognostically unfavorable injuries to the body. There is no strict parallelism between the degree of injury to the spine and spinal cord: for minor injuries
The most severe, irreversible damage to the spinal cord can be observed in spinal injuries; however, with more severe spinal trauma and especially with significant narrowing of the spinal canal, the frequency of severe brain damage increases.
The mechanism of spinal cord injury can be very different, which determines the dynamics of post-traumatic changes and the prognosis of the disease, but often has little effect on the picture of the acute period. Post-traumatic changes in the spinal cord (tear or complete break) and persistent hemodynamic disturbances arising in it are irreversible. The spinal cord can be further damaged as a result of compression by bone fragments, increasing hemorrhage, and swelling. Timely elimination of these pathological factors can lead to regression of the disorders caused by them and restoration of the functions of the spinal cord in accordance with the degree of preservation of its structures. It is necessary to take into account that all post-traumatic changes in the spinal cord occur in a narrow bone canal and with focal compression or pathological enlargement (edema-swelling, hematomyelia), the spinal cord is pressed against the walls of the canal. In this case, additional compression of all its elements occurs, primarily the vessels, which causes legal structural and functional changes.
The study of pathophysiological mechanisms immediately after spinal cord injury shows that the phenomena of spinal shock come to the fore. Under the influence of trauma, deep dynamic disturbances occur in nerve cells and complex connections of the spinal cord, which is characterized by temporary inhibition of all functions of the nerve cell, loss of nerve fiber conductivity, and absence of reflex activity of the spinal cord. The depth and duration of spinal shock depend on the severity of the injury. However, in the initial period of injury, the picture of severe spinal shock turns out to be identical to the picture of a complete anatomical break of the spinal cord, which greatly complicates diagnosis. Spinal shock is most pronounced in the first days and weeks after injury. Then signs of it
gradually smooth out. The nature and severity of spinal cord damage are determined only after complete recovery.
the patient's progress from the state of spinal shock (on average 4-8 weeks after injury).
In the clinical picture of injury to the spine and spinal cord, also called complicated spinal injury, it is important to clearly understand that in the initial period the symptoms are identical for a wide variety of types and degrees of spinal cord injury. Typically, following an injury, there is a sudden loss of motor, sensory and reflex functions below the level of injury. Patients complain of pain in the area of the injured vertebra, which intensifies with passive movements in it. In the first hours, dysfunction of the pelvic organs is detected (retention of urine and feces, sensation of passing urine and feces, absence of pain when squeezing the testicles); Gross disturbances of autonomic functions are observed; below the level of damage, a decrease in skin temperature and sweating disorder are characteristic.
Spinal cord concussion.
The submicroscopic picture corresponds to that of a concussion. Pathophysiologically, concussion is characterized by the reversibility of functional changes. In the clinical picture, dysfunctions of the segmental apparatus often prevail; conduction tracts are less frequently and less affected. Regression of pathological symptoms occurs in the next few hours after the injury, sometimes in the next few days or 2-3 weeks.
Spinal cord contusion.
With a bruise, hemorrhages of varying sizes, swelling, softening of parts of the spinal cord, and imbibition of the brain matter by blood are observed. Spinal cord dysfunction occurs immediately following injury. Regardless of the degree of morphological changes, in the first 2-3 weeks after the injury, complete loss of spinal cord functions is observed - paralysis and anesthesia below the level of injury, urinary and fecal retention. Then neuro-dystrophic and inflammatory complications (bedsores, cystopyelonephritis, pneumonia) may occur. The so-called physiological break of the spinal cord in the first days and even weeks cannot be distinguished from the anatomical one.
In the case of a bruise, an admixture of blood is noted in the cerebrospinal fluid; the patency of the subarachnoid space is not impaired.
Restoration of impaired functions following a spinal cord injury begins gradually, after 2-5 weeks. The phenomena of spinal shock disappear, tendon and then skin reflexes and muscle tone are restored, pathological reflexes arise, active movements first appear in the most massive muscle groups, and then in the feet and fingers, and finally, the patient begins to move independently. The upper limit of anesthesia drops, anesthesia gives way to hypoesthesia, and the function of the pelvic organs gradually normalizes. The timing and degree of restoration of functions are directly proportional to the severity of the bruise. In case of severe injury, restoration of movements, sensitivity and functions of the pelvic organs occurs within several months; pronounced residual effects persist for a long time in the form of paresis of individual muscle groups, especially in the extremities, hypoesthesia, paresthesia, and trophic disorders.
Spinal cord compression
usually combined with a bruise or crush. Compression of the spinal cord itself occurs when the vertebrae are fractured with displacement of the fragments towards the spinal canal. A fracture of the arch entails predominantly posterior compression; with a fracture of the vertebral bodies, anterior compression occurs with an Urban wedge. Bone fragments embedded in the spinal canal not only compress the spinal cord, but also damage it
Symptoms of compression due to a vertebral fracture develop immediately after the injury. Conductive motor and sensory disorders are approximately the same as with contusion and crushing of the brain. With less pronounced compression, sensitivity is disturbed asymmetrically and at different levels, anesthesia is gradually replaced by hypoesthesia, its upper limit decreases, movement disorders are asymmetrical, and there are no changes in trophism. The symptoms of spinal shock pass faster and earlier. With severe compression of the spinal cord, the clinical picture resembles that of an anatomical break in the brain.
When an epidural hematoma occurs due to rupture of the epidural veins, the gushing blood quite easily spreads up and down along the epidural space, compressing segments of the spinal cord. At the same time, the clinical picture is quite often
characterized by the presence of a light interval of varying duration, then radicular girdling pain, reflex tension of the back muscles at the level of the hematoma, positive shell symptoms, limitation of movements in the spine due to pain and muscle tension appear. Soon, conduction and segmental disorders appear in the form of paresis of the limbs, sensitivity disorders, extinction of tendon and skin reflexes, difficulty urinating and defecating. During lumbar puncture, a partial or complete cerebrospinal fluid block is often determined; the fluid itself is without pathological changes. Bleeding from epidural veins, which have a small diameter, stops on their own; in addition, due to the lack of a tendency to limit the accumulation of blood, compression relatively rarely leads to a complete transverse disruption of the conductivity of the spinal cord. However, the resulting partial conduction disorder is not always restored and is a cause of disability.
Spinal cord crush
is a consequence of a penetrating wound by any object or, much more often, bone fragments or displacement of one vertebra in relation to the adjacent one due to a vertebral fracture, dislocation or fracture-dislocation.
When the spinal cord is crushed, which leads to a complete anatomical break, below the level of damage there is a loss of motor and sensory functions, there is no bladder reflex, pain when the testicles are compressed, the trophism is severely affected (bedsores, hemorrhagic cystitis and gastritis, hard swelling of soft tissues). Restoration of lost spinal cord functions does not occur.
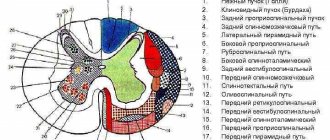
Hematomyelia
- hemorrhage into the gray matter of the spinal cord. Most often occurs at the level of the cervical and lumbar thickenings. In the clinic, a combination of segmental and conduction disorders is observed. Symptoms of the lesion occur following the injury and can progress over several hours as bleeding increases. One of the important symptoms is a dissociated sensitivity disorder - preservation of deep and loss of superficial sensitivity on both sides, according to the level of the lesion. In case of defeat before
Paresis and peripheral paralysis are observed in the horns of the spinal cord. In cases of compression of the lateral cords by shed blood below the level of damage, paresis and paralysis of a central nature, a decrease or loss of conduction-type superficial sensitivity, and dysfunction of the pelvic organs occur.
Damage to the spinal cord roots.
There are primary injuries resulting from exposure to a directly wounding object, and secondary injuries resulting from a vertebral fracture, displacement of the intervertebral disc, or the yellow ligament. In this case, bruise of the roots with intra-stem hemorrhage, stretching, compression (partial or, less often, complete) may occur. With certain types of injury, one or more roots may be torn from the spinal cord, usually in the cervical spine. Clinically, according to the area of damage, sensitivity disorders occur in the form of hyper-, hypo-, or anesthesia (depending on the degree of damage). When the anterior roots are damaged, peripheral paralysis and paresis occur, followed by atrophy of the corresponding muscles. Autonomic disorders occur (hyperhidrosis or anhidrosis, etc.).
Clinic and topical diagnosis of spinal cord injuries.
The upper limit of spinal cord injury is determined primarily by the study of skin sensitivity, the lower limit by tendon reflexes, protective movements, and on the basis of reflex dermographism. It must be emphasized that determination of the lower limit of damage is possible only after the disappearance of the phenomena of spinal shock. In addition, spinal shock, aggravated by hemodynamic disorders and edema, which spreads to the parts of the spinal cord above the injury, in the acute period does not always make it possible to correctly determine the upper limit of the injury. Spinal shock makes it difficult to determine the degree of damage to the spinal cord and often mimics the clinical picture of a complete cord interruption.
Damage at the cervical level.
Damage to the upper cervical spinal cord (Ci-Civ) is characterized by tetraplegia of the central type, loss of all types of sensitivity below the level of damage.
waiting, radicular pain in the shen area, radiating to the occipital region, dysfunction of the pelvic organs of the central type (urinary and fecal retention). If the Civ segment is damaged, the center of innervation of the diaphragm is destroyed, respiratory failure occurs: the patient gasps for air, the neck muscles are tense, exhalation occurs passively, cyanosis of the skin and mucous membrane is noted due to hypoxia. When the edema spreads to the brainstem, bulbar symptoms develop, respiratory and circulatory disorders become even more aggravated, vomiting, hiccups, swallowing problems appear, and the voice becomes quiet. Patients usually die in the first days or weeks after injury.
With damage to the lower cervical spinal cord (Cv-Cvin), peripheral flaccid paralysis of the upper limbs and central spastic paralysis of the lower limbs, loss of all types of sensitivity below the level of damage, radicular pain in the upper limbs, shallow breathing due to paralysis of the intercostal muscles are observed; inhalation occurs actively, due to the preservation of the innervation of the diaphragm, scalene, sternocleidomastoid and trapezius muscles. Disorder of the functions of the pelvic organs according to the central type.
When diving into water and hitting the head on the bottom, a fracture-dislocation of the VII cervical vertebra with damage to the spinal cord at the level of the segment of the same name most often occurs. In this case, central paralysis of the lower extremities and torso is observed with partial preservation of movements in the upper extremities, namely in the shoulder joints and flexion movements in the elbow joints. Upon examination, the victim’s arms are bent at the elbow joints, usually lying on the chest, the small muscles of the hand and fingers are paralyzed.
As a result of damage to the spinal cord at the level of the Cvin-Ti segments, the ciliary spinal center on one or both sides is involved in the process, the sympathetic innervation of the eye is disrupted with the development of unilateral or bilateral Horner's syndrome.
With a complete anatomical break of the spinal cord at the level of the cervical spine, patients usually die.
Damage at the thoracic level.
If the spinal cord is damaged at the level of the thoracic segments at
there is central paraplegia of the lower extremities;
damage at the level of Ti-Tup also causes paralysis of the intercostal muscles, as a result of which breathing is impaired. Sensitivity decreases according to the level of damage. In case of damage at the level of the Tu segment, loss of sensitivity is determined along the line of the nipples, Tush - at the costal arches, Tx - at the level of the navel and Txp - at the level of the inguinal ligament. At the level of damage, radicular pain may occur. Dysfunction of the pelvic organs of the central type.
Damage at the level of the lumbar enlargement
(Li-
Sn ) -
Peripheral paralysis of the lower extremities with pronounced atrophy and atony of muscles is noted. Cremasteric, knee, and heel reflexes are absent, all types of sensitivity below the level of the inguinal ligament and in the perineal area are lost. Trophic cystitis with hematuria and bedsores often develop early. Sometimes the picture of an acute abdomen can be simulated. The functions of the pelvic organs are impaired centrally, but peripheral disorders may occur, in which urinary and fecal retention is replaced by incontinence.
Damage at the level of the conus medullaris
(Sin-
Sy ).
Characterized by loss of all types of sensitivity in the perineum and genital area (in the shape of a saddle), atrophy of the gluteal muscles. The functions of the pelvic organs are disturbed in a peripheral manner, usually true urinary and fecal incontinence and sexual weakness occur. The lower extremities are not affected. Isolated damage to the conus medullaris is rare.
Damage to the cauda equina
occurs with a fracture of the lumbar vertebrae (usually III and IV). Symmetrical clinical manifestations are not typical, since rarely all roots are affected to the same extent. With severe damage to all elements of the cauda equina, peripheral paralysis of the lower extremities is observed with loss of tendon reflexes and muscle atrophy, loss of all types of sensitivity in the corresponding innervation zones, urinary and fecal incontinence. In addition, it is characterized by constant, sometimes extremely intense pain, which occurs immediately after the injury or after some time and is localized in the area of the lower extremities, perineum, genitals, often in the area of complete lack of sensitivity.
With incomplete damage to the cauda equina, paraplegia is not observed; certain types of movements are preserved in the lower extremities. An uneven sensitivity disorder is noted when areas of anesthesia alternate with areas of hypoesthesia or normal sensitivity.
If only the sacral roots are damaged,
which occurs with injury to the III-V sacral vertebrae, there are no motor and sensory disorders in the lower extremities. The main symptoms are loss of sensitivity in the perineal area, pain, often intense, in the buttocks, rectum, penis or vagina, dysfunction of the pelvic organs of a peripheral type (sacral herringbone syndrome).
When diagnosing injuries to the spine and spinal cord, radiography in at least two projections is mandatory - anteroposterior and lateral. The presence of a fracture, especially with displacement of the vertebrae and their fragments, and clear clinical manifestations often make further clarification of the diagnosis unnecessary. If a fracture is not detected by x-ray, a study of the cerebrospinal fluid and mandatory liquorodynamic tests are necessary, since treatment tactics depend on their results.
Complications of spinal cord injury.
One of the early and severe complications is
traumatic shock
and
collapse,
which usually occurs with a combination of damage to the spine and spinal cord.
Below the level of spinal cord damage, trophism of tissues and internal organs noticeably suffers. Frequent and serious complications of this kind include bedsores and maceration.
They usually develop in the area of bony protrusions (sacrum, greater trochanter, heel, elbow joint, scapula, etc.). Bedsores, as a rule, form in patients who remain in bed in one position for a long time. Contamination of the bed with urine and feces and failure to comply with hygiene rules contribute to the development of bedsores. Bedsores develop more quickly in cases of severe damage to the spinal cord, in particular with its anatomical break, with injuries in the thoracic and lumbar parts of the spinal cord, and less often with injuries to the cervical spine.
The development of bedsores begins with redness and swelling of the skin, the formation of blisters with the rapid addition of foci of necrosis of the skin and subcutaneous tissue, which gradually spreads to the muscles and even bones, and the disintegrated tissues are rejected. Bedsores often reach very large sizes. In patients with bedsores, a large amount of protein is lost through the wound surface, hypoproteinemia occurs, which significantly reduces the body's reactivity. In some cases, bedsores quickly become infected, sometimes purulent streaks form, which can serve as a source of sepsis.
The sepsis clinic is characterized by remitting body temperature, chills, profuse sweating, vomiting may occur, hysteria of the sclera and skin is often associated, leukocytosis in the blood, a shift in the formula to the left, a sharp increase in ESR. Often, cachexia gradually increases with sepsis.
Against the background of a paralytic state of the bladder and urinary retention, neurodystrophic and inflammatory changes develop in the bladder wall, and catarrhal, hemorrhagic or ulcerative cystitis occurs.
It is accompanied by
pyelitis and pyelonephritis.
In the future, this can lead to the development of urosepsis.
With injuries to the cervical and upper thoracic spinal cord, acute trophic disorders often occur in the lungs and in the form of bronchopneumonia, pleuropneumonia
with rapid transition to
pulmonary edema.
The prerequisite for this in the early period after injury is not only neurodystrophic changes in the lung tissue itself, but also disorders of external respiration as a result of impaired innervation of the diaphragm and intercostal muscles. The development of pneumonia is also promoted by aspiration of mucus from the upper respiratory tract, vomit, and food. Damage to the spinal cord and its roots at the level of tiv-Tu in some cases causes disruption of the activity of the heart and blood vessels.
Neurotrophic disorders in the abdominal organs are most pronounced in injuries of the lower thoracic and lumbar spinal cord and are manifested by disorders of the stomach functions
and
intestines, pancreas, adrenal glands.
Paralysis of the intestines, dyskinesia, stasis, disruption of digestive processes sometimes give the picture of an acute abdomen.
With spinal cord injuries, the functions of the pelvic organs are always impaired:
urination and defecation, as well as sexual function, are affected. These disorders usually occur immediately after injury. Depending on the level of damage to the spinal cord, urination disorders are distinguished by the conductive (central) type, when the lesion is located above the spinal centers (Sin-Sv), which regulate urination, and by the peripheral type, in cases of damage to the spinal centers themselves and their roots. With the central type of urination disorder, which occurs as a result of bilateral shutdown of the corticospinal motor tracts passing in the lateral cords, urinary retention occurs as a result of increased reflex excitability. When the corticospinal tract is not completely switched off, imperative urges are characteristic: urination is carried out frequently and in small portions. When the conus medullaris and its roots are damaged, flaccid paralysis of the muscle that pushes out urine occurs, and urine, without being retained in the bladder, is released out, urinary incontinence occurs (a peripheral type of urinary disorder). However, there is a delay at first. Damage to the spinal cord above the spinal center leads to spastic paralysis of the rectal sphincter, causing stool retention, sometimes very persistent. When the spinal center is damaged, fecal incontinence and involuntary passage of gases are observed.
The primary erection centers are located at the level of the Si-Sn segments, and damage to the spinal cord above these centers leads to involuntary congestion of the corpora cavernosa of the penis, which can remain erect for a long time. If the center itself is damaged, an erection does not occur. Lack of ejaculation is observed when the primary centers located in the conus medullaris are damaged.
Disturbances in the functions of internal organs in severe spinal cord injuries are very persistent and in some cases do not recover for many years.
Treatment. The choice of therapeutic measures is determined by the type of traumatic injury to the spinal cord, the nature of the complications that have developed, and the time elapsed since the injury.
When providing first aid, depending on the severity of the patient’s condition, they combat shock and collapse, disruption of vital functions,
primarily breathing and blood circulation. Victims are transported on rigid stretchers or on boards in a supine position for cervical injuries and on the stomach for thoracic and lumbar injuries, preferably with immobilization of the injured spine. Hospitalized without intermediate steps directly to a neurosurgical or trauma hospital.
The main thing is the correct organization and precise implementation of treatment in the acute post-traumatic period.
Therapeutic tactics, i.e., carrying out only conservative therapy or combining the latter with surgical intervention, is determined by a single criterion - the presence of spinal cord compression. If it is present, then regardless of what and to what extent the spinal cord is compressed, surgical intervention is necessarily indicated as early as possible, preferably in the first hours after the injury. Without eliminating compression of the spinal cord, improvement in its functional state, as a rule, does not occur. The operation is inappropriate in cases where there is a complete anatomical break of the spinal cord. However, it is usually impossible to deliberately decide the issue of complete or partial interruption of the spinal cord in the preoperative period.
Refusal of surgery can be justified only by the presence of contraindications, but not by diagnostic doubts. Carrying out an operation on a patient with a complete crush of the brain will not worsen his condition, and failure to eliminate compression in the case of partial brain damage will make it impossible to achieve a certain improvement.
The surgical technique for a spinal fracture is conventional, but takes into account the preservation of the physiological axis of the spine. When skeletonizing the spinous processes (Fig. 78) and arches, care must be taken, since brain injury can be aggravated by bone fragments. Then a laminectomy is performed, as a rule, the arches of three vertebrae are subject to biting - the damaged one, the one above and the one below (Fig. 79). Carry out thorough hemostasis. A linear incision along the midline is used to open the dura mater (Fig. 80) and inspect the spinal cord. Carefully use cotton balls to remove blood clots; if the brain substance is damaged, wash the brain detritus with isotonic sodium chloride solution and suction it with an aspirator with a thin tip through a cotton strip.
When the spinal cord is completely interrupted, all free tissue and necrotic areas are removed. When the roots of the cauda equina are ruptured, the latter are sutured, if possible, using magnifying optics and microsurgical techniques. Be sure to resect the displaced part of the vertebral body (Urban wedge) towards the spinal canal and remove the damaged intervertebral disc. The dura mater is hermetically sutured and only in cases of severe swelling of the spinal cord, guiding sutures are placed on it. Laminectomy is completed with posterior spinal fusion (Fig. 81), which ensures fixation of the damaged area of the spine and prevents secondary displacement of the vertebrae - an unstable fracture is converted into a stable one. For spinal fusion, auto- or allografts (lyophilized or frozen bone), as well as wire, lavsan, metal clamps, and plastics are used.
Stabilization of the spine allows the patient to freely change points of support and turn the patient after surgery. Spinal dislocation is corrected surgically with mandatory fixation of the vertebrae.
For compression fractures of the cervical vertebral bodies, an anterior approach is recommended. A skin incision along the inner edge of the sternocleidomastoid muscle is 10-12 cm long. The subcutaneous muscle of the neck and the superficial fascia are dissected. The sheath of the sternocleidomastoid muscle is bluntly isolated and retracted outward, the trachea and esophagus are retracted in the opposite direction.
The next step is to open the middle fascia and bluntly dissect the tissue to the prevertebral fascia. This fascia is then incised longitudinally to expose the anterior longitudinal ligament, vertebral body and intervertebral disc. The latter, together with bone fragments, is removed, and the defect is replaced with a bone graft. The wound is sutured layer by layer in the reverse order.
In case of subluxation in the cervical spine, as well as in case of a fracture, which is accompanied by general severe
severe condition of the patient, traction is performed on the parietal tuberosities (Fig. 82) or zygomatic arches, then surgical treatment is carried out and a Shants collar is applied. Under traction, the patient may turn in bed.
In the acute period, it is necessary to ensure that the patient is positioned correctly in bed. The requirement of immobility may not be acceptable due to the possibility of pressure sores. The patient is placed on a functional bed or a regular bed with a shield. Mattresses should be cotton wool or foam rubber, i.e., allow air to pass through well, and the sheets should be dry and smooth. Air and water rubber mattresses and backing pads are not suitable. Special bags filled with flax grains, millet, or cotton rolls are placed under the shoulder blades, sacrum and heels. Changing the support points and position of the patient in bed (on the back, stomach, side) is carried out in the first weeks strictly every 2 hours, at this time massage the skin, treat it with the use of tanning agents (cologne, aqueous solution of tannin, etc.). Maceration areas are treated with a concentrated solution of potassium permanganate.
It is necessary to protect the sacral area from contamination with feces and urine
The primary goal in caring for patients with spinal cord injury is to ensure systematic and timely emptying of the bladder and colon. Emptying the bladder is carried out by repeated catheterization, which is periodically replaced by a more rational method of removing urine - the Monroe system Antiseptic solution (ethacridine lactate - rivanol, furatsilin 1 5000) from the reservoir through
drip, tube and catheter flow into the bladder in slow drops. Considering that normally the bladder reflex occurs at a pressure of 150 mm of water column, the outlet end of the tee is raised 15 cm above the level of the bladder (pubes), which maintains the required pressure in it. During the first time after the injury, purely mechanical washing out of urine occurs. Under the influence of constant irritation of the muscle that pushes urine out, involuntary contractions of the bladder begin to occur. This helps to train the muscle and maintain normal bladder capacity, which facilitates the normalization of the act of urination while restoring the function of the spinal cord, and in case of an irreversible process, the development of automaticity. In these cases, it is advisable to change the catheter once a week while observing the strictest asepsis.
A high section of the bladder is performed only in exceptional cases - in case of destruction of the conus medullaris, fracture of the pelvic bones and rupture of the bladder, as it leads to a sharp decrease in bladder capacity and prevents the development of the bladder reflex.
Much attention is paid to organizing the diet. Food should be easily digestible, high in energy value, and initially rich in carbohydrates. In order to improve digestion, hydrochloric (hydrochloric) acid and gastric juice are prescribed. To stimulate intestinal motility, intravenous administration of a hypertonic solution of sodium chloride, proserine, physostigmine, high enemas with turpentine, and glycerin are most effective. Transfusions of blood, plasma, albumin, protein hydrolysates, and amino acids are recommended. For bedsores, in addition to medications, ultraviolet irradiation, dressings with antiseptics and antibiotics, hypertonic solutions, and ointment dressings are used. Surgical treatment consists of excision of necrotic tissue
The complex of treatment measures includes symptomatic therapy and measures are taken to prevent complications.
Prevention of pneumonia involves breathing exercises, exercise therapy, and massage. Certain types of injuries require special additional treatment.
In cases of concussion or mild contusion of the spinal cord without damage to the spine, medications are prescribed that increase metabolism in the nerve cell, excitability and conductivity of the spinal cord (amina-
lon, parmidin - prodectin, galantamine, glutamic acid, dibazol, piracetam - nootropil, pyriditol - encephabol, prozerin, etc.), absorbent agents (aloe, vitreous, FiBS, lidase, pyrogenal, iodine preparations). Much attention is paid to exercise therapy and physiotherapy (galvanization along the spine, iontophoresis of iodine, proserine, and novocaine for pain).
After 3-4 months, patients are transferred to the rehabilitation department. The first preparatory period of medical rehabilitation lasts 3-6 months and is considered completed when the patient independently cares for himself in bed. Subsequently, the patient is taught to walk in therapeutic gypsum gelatin splints, and after 2-3 months - the ability to use fixing splint-sleeve devices. In parallel with medical rehabilitation, labor readaptation is also carried out. Patients are taught work performed in a sitting position. Every 2-3 years they are hospitalized for re-examination and monitoring of labor readaptation. Persons who have suffered a spinal cord injury are subject to dispensary observation.
Table of contents