Table 2 Psychophysiological characteristics and prognosis of conditions occurring with disorders of consciousness
| State | Self-centeredness | Sleep-wake cycle | Feeling pain and suffering | Forecast |
| Persistent vegetative state | Absent | Saved | No | Depends on the reason |
| Coma | Absent | Absent | No | Recovery of consciousness Persistent vegetative state Death within 2-4 weeks |
| Brain death | Absent | Absent | No | No recovery |
| Locked-in syndrome* | Saved | Saved | Yes | Recovery is unlikely, persistent tetraplegia, with good care, patients live a long time |
| Akinetic mutism** | Absent | Saved | Yes | Recovery is extremely unlikely (depending on the cause). |
| Dementia | Preserved, but lost in later stages | Saved | Yes. In later stages it is lost. | Progressive deterioration. Rate of progression depends on cause |
*Locked-in person syndrome is characterized by anarthria and tetraplegia, with preservation of the main manifestations of consciousness; this condition should be clearly distinguished from other types of disorders of consciousness.
**Akinetic mutism: refers to the condition originally described by Cairns (1941), complete wakefulness with absence or weakness of speech activity and voluntary movements. These patients show signs of conscious behavior, but the desire or attempts to speak or move are grossly disorganized. A large number of clinical and pathological variants of this condition have been described. Most often, akinetic mutism occurs with bilateral damage to the reticulocortical and limbic-cortical connections in the central part of the brain, extending from the paramedian areas of the reticular formation to the midbrain and diencephalon, basal and medial areas of the frontal lobes (Plum & Posner, 1980). N Engl J Med 1994; 330:1499. quoted from https://www.uptodate.com/contents/approach-to-the-adult-patient-with-syncope-in-the-emergency-department
Determining whether a patient belongs to any of the groups is important for prognosis, development of approaches to treatment, distribution of resources, and resolution of medico-legal issues.
Clinical examination of the patient
Recommendations for assessing response in neurocognitive disorders
- Adequate stimulation is carried out only when it is certain that the patient's level of wakefulness is maximum.
- It is necessary to eliminate the causes that cause quantitative disorders of consciousness (taking sedatives, epileptic seizures).
- Attempts to elicit a response to verbal stimulation should not be aimed at eliciting movements, which are often performed reflexively.
- Research into the ability to carry out commands should include the types of motor activity available to the patient.
- Many different behavioral responses must be examined using a diverse range of stimuli.
- The study should be carried out in a calm environment.
- Initial estimates should be verified repeatedly using multiple re-assessments and acceptable response measurement approaches.
- Specific quantification techniques and tools may be useful.
A systematic approach to assessing patients with impaired consciousness includes the following steps:
Assessment of the functioning of the brain stem and other subcortical formations
- Pupillary reactions, blink reflex to visual stimuli.
- Eye movements, gaze deviations.
- Oculovestibular reflexes (oculocephalic reflex, calorimetric test).
- Corneal reflexes.
- Vomiting reflex.
- Breathing pattern.
- Decerebrate postures.
- Other postural reflexes, assessment of muscle tone.
Assessment of cortical functions
- Evaluation of voluntary actions
- Purposeful complex movements (including isolated motor control involving the cortex) compared with postural (decortication, decerebrate) or reflexive or stereotyped, monotonous (subcortical structures mediated) movements. Note: Pilon & Sullivan note different profiles of postural tone relationships for VS and SMS. Patients with VS exhibit classic decerebrate, decortication, and hypotonic postural features, whereas patients with SMS exhibit symmetrical or asymmetrical global flexor postures. However, there is no characteristic reflex posture with absolute diagnostic significance for separating these two groups.
- Involuntary vocal and verbal activity.
- Eye movements (signs of fixation of gaze or tracking of an object, differentiated from involuntary eye movements not related to the stimulus, or fixed gaze); responses to artificial or natural external stimuli.
- Tracking or fixating the gaze on various stimuli (use objects that do not make sounds: family photos, pictures of faces, money, mirror)
- Verbal stimulation (patient's name, commands, greeting): Begin with simple commands that encourage actions within the patient's ability.
- Eye commands: “look here”, “blink twice”.
- Commands for limbs: “show thumb”, “show 2 fingers”, “raise your hand”.
- Commands for the oral muscles: “open your mouth”, “show your tongue”
- Commands for the whole body or axial muscles: “turn your head”, “lean forward”.
- Ask the patient to stop the movement or hold the limb to highlight spontaneous repetitive movements.
- Painful stimulation.
- Assess the localization and purposefulness of defensive reactions, compare them with reflexive and generalized, stereotypical movements, evaluate facial expression
- Responses to random external stimuli.
- Assess attempts to grasp or perform actions with objects surrounding the patient (clothing, objects at hand).
- Observe changes in facial expression as you respond to stimuli such as a familiar voice, dialogue, pictures, music, etc.
- Notice attempts at purposeful movement in bed, in a chair, and while walking.
- Note gestures when communicating emotionally (yes/no signals).
Neuropsychiatric complications of brain injury
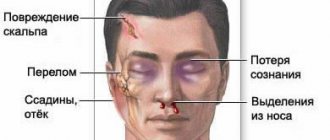
Traumatic brain injury (TBI) is the most common cause of hospitalization in young adults, with a higher prevalence in men. TBI is a leading cause of disability and death between ages 1 and 45 years. TBI can be either a direct result of the injury or occur as a complication of the primary injury. . The most common etiologic factors for TBI are falls, motor vehicle accidents, physical assault, and sports-related injuries. Significant neurological complications can occur following a TBI, which include seizures, dementia, and cranial nerve injuries. In addition, patients who have suffered a traumatic brain injury may suffer from a variety of mental health disorders, such as depression, post-traumatic stress disorder, generalized anxiety disorder, obsessive-compulsive disorder, and other cognitive and behavioral disorders.
Literature data indicate that only about 25% of patients who have suffered a traumatic brain injury achieve long-term “functional independence.”
Traumatic brain injury (TBI) primarily refers to brain dysfunction caused by external trauma. In the US, high school football players alone suffer 100,000 diagnosed concussions per year. Similarly, boxing can cause concussion from a punch to the head, causing rupture of bridging veins (subdural hematoma), microhemorrhages in the brain, and diffuse axonal damage.
Risk factors that worsen outcome include age, existing illnesses such as tumors, repeated trauma, and alcohol abuse. Each year, 10 million people suffer from TBI worldwide, of which 5.3 million are from the United States. Every year, about 52,000 people die from TBI. Falls are the most common cause of TBI in children aged 0-4 years and adults aged 75 years and older. Other common causes are motor vehicle accidents (14%) and brain injuries due to physical shock during violent acts (12%). TBI rates were nearly 30% higher in men compared to women in 2010. Alcohol intake is a major factor leading to traumatic brain injury (blood alcohol concentration was positive in 56% of patients with traumatic brain injury).
There are many different types of traumatic brain injury: concussions (a brief loss of consciousness in response to a head injury); penetrating injury (a foreign object enters the brain); closed head injuries (blow to the head); skull fractures (bone fractures or ruptures); hematomas (bleeding in the brain); lacerations (torn blood vessels or tissue); anoxia (lack of oxygen supply to brain tissue); shell shock; and diffuse axonal damage, which leads to the destruction of connections between neurons.
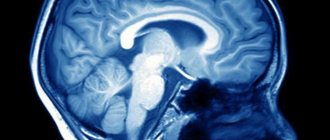
Pathological studies of coma patients with diffuse axonal damage tested with computed tomography scans have shown widespread white matter axonal damage. Diffuse axonal injuries are the result of severe acceleration or deceleration. Even if patients experience diffuse axonal injury, permanent neurological deficits persist throughout their lives. On MRI, we can see focal lesions in the corpus callosum, which appear as clusters of petechial hemorrhages and can lead to intraventricular hemorrhages. Cranio-brain injuries also include petechial hemorrhages in the brainstem. More severe trauma results in hemorrhagic softening of the dorsal midbrain. Surviving patients with diffuse axonal injury usually have severe brain atrophy, dilatation of the lateral and third ventricles, and thinning of the corpus callosum. Microscopic examination reveals diffuse axonal damage in the corpus callosum, superior parasagittal cerebral white matter, brainstem, and various tracts.
As is known, patients who have suffered a traumatic brain injury must be on bed rest for a certain period of time to prevent further brain injury. Adequate oxygen supply, maintenance of adequate blood flow and blood pressure control are critical variables that are considered in the treatment of the effects of brain injury. About half of patients with traumatic brain injury require surgery to repair brain tissue and treat other injuries.
The most common (short-term) complications associated with traumatic brain injury are cognitive impairment, sensory processing difficulties, hydrocephalus, cerebrospinal fluid (CSF) leakage into tissue, vascular or cranial nerve damage, tinnitus, and certain deficiencies. organs and polytrauma. Polytrauma may include: pulmonary, cardiovascular, gastrointestinal dysfunction and hormonal imbalance, deep vein thrombosis, increased blood clotting and nerve damage. . Patients with traumatic brain injury have an increased metabolic rate, which results in an excessive amount of heat generated in the body. Cerebral edema is secondary to TBI and contributes to increased intracranial pressure as a result of vasodilation and increased cerebral blood flow. Long-term complications associated with traumatic brain injury include Parkinson's disease, Alzheimer's disease, dementia and post-traumatic epilepsy.
Penetrating trauma may produce psychopathological symptoms depending on the specific function of the affected region (eg, aggression and behavioral disinhibition in bifrontal brain injury). Symptoms following trauma can be explained by cytotoxic processes such as Ca + 2 and Mg + 2 dysregulation, neurotransmitter excitotoxicity, free radical-induced injury, and diffuse axonal injury.
Damage to the ascending monoaminergic tracts can cause abnormal functioning of systems dependent on these pathways. Several studies show that TBI in these areas leads to decreased dopamine levels, which predicts a poor prognosis. Psychotropic drugs that improve dopaminergic transmission contribute to improved cognitive functions (eg, activation, information processing speed, processes associated with attention and memory).
Serotonin tracts that travel to the frontal cortex are interrupted by contusions, as well as axonal damage, causing dysfunction in this neurotransmitter system. These pathways can also be damaged by secondary mechanisms of neuronal injury, such as excitotoxins and lipid peroxidation, which mediate serotonin activity. Cerebrospinal fluid (CSF) 5-HIAA levels vary depending on the size of the injury, for example, patients with frontotemporal contusions show decreased 5-HIAA levels, whereas increased levels are seen in diffuse brain contusions.
After traumatic brain injury, there is an increase in cholinergic transmission followed by a chronic decrease in the function of this neurotransmitter and cholinergic afferents. In experimental studies, increased levels of acetylcholine are observed during the placement of interventricular catheters or lumbar puncture in the acute period after traumatic brain injury. In the chronic course of the consequences of traumatic brain injury, there is a loss of cortical cholinergic afferents with simultaneous preservation of postsynaptic muscarinic and nicotinic receptors.
The prevalence of mental disorders after traumatic brain injury is as follows: 14% -77% for major depression, 2-14% for dysthymia, 2% -17% for bipolar affective disorder, generalized anxiety disorder - 3% -28%, panic disorder disorders - 4% -17%, phobic disorders - 1% -10%, obsessive-compulsive disorder (OCD) 2% -15%, post-traumatic stress disorder (PTSD) 3% -27%, substance abuse or addiction 5% - 28% and schizophrenia - 1%. Many factors are known to influence and determine the neuropsychiatric complications of TBI, including severity and type of injury, past psychiatric diagnosis, sociopathy, premorbid behavioral problem (especially in children), social support, substance abuse, pre-existing neurological disorders, age, and apolipoprotein levels. E.
Patients suffering from direct axonal injury typically experience problems with activation, slow cognitive processing and attention. Age is an important factor in the development of psychiatric symptoms, for example, older people affected by TBI have a longer period of agitation, greater cognitive impairment, and a higher likelihood of developing global body damage. Damage to the olfactory nerve, located near the orbitofrontal cortex, can cause post-traumatic anosmia. Impaired functioning of the olfactory system can often occur in patients with moderate to severe traumatic brain injury associated with damage to the frontal and temporal lobes.
Agitation occurs in 96% of patients who have suffered a traumatic brain injury, and cognitive impairment - in 70%, depression - in 61%, generalized anxiety disorder - in 28%, post-traumatic stress disorder - in 27%, panic disorder - in 17% , obsessive-compulsive disorder - in 15%, phobic disorders - 10% and mania - in 4% of cases.
Depression is one of the most well-known mental disorders caused by the consequences of traumatic brain injury. Sadness is the most common reaction after TBI as patients regret their past life. Note that high scores on the Beck Depression Inventory represent hyperreactivity to symptoms following traumatic brain injury and do not indicate the severity of depression. Patients with TBI may not have typical signs of depression, such as physical symptoms, which are traditionally needed to diagnose depression. Mood changes have also been observed in temporal, limbic, and basal forebrain lesions, and such depressions have been reported to respond to antidepressants. Other symptoms that appear after traumatic brain injury are apathy, decreased motivation, “schizotypal behavior,” impaired thinking and cognitive dysfunction, which, however, in their clinical manifestations may resemble depression. An increased risk of suicide has been reported following TBI (at one year, 10% of patients had contemplated suicide and 2% had attempted suicide).
Some patients suffer from bipolar disorder or manic episodes after a traumatic brain injury. Damage to the basal region of the right temporal lobe and the right orbitofrontal cortex causes the development of manic symptoms after traumatic brain injury in patients with a positive family history of bipolar disorder.
A patient may experience psychosis at any time after a traumatic brain injury, in the acute phase, or even after several months of normal functioning. Delirium often occurs after waking from a coma. Typical symptoms in this case are restlessness, confusion, disorientation, hallucinations, agitation and delusions. The latter can develop as a result of the mechanical effects of injury, cerebral edema, hemorrhage, infection, subdural hematoma, hypoxia (cardiopulmonary or local ischemia), increased intracranial pressure, alcohol intoxication or hangover syndrome, Wernicke encephalopathy, decreased heperfusion due to multiple trauma. Other contributors to delirium include fat embolism, pH changes, electrolyte imbalances, and medications (steroids, opioids, barbiturates, and anticholinergics).
Many psychiatric disorders following traumatic brain injury, such as mania, depression, and epilepsy, can lead to psychotic symptoms. These symptoms may persist despite improvements in the cognitive deficits caused by the injury. In one study of Finnish war veterans who had suffered traumatic brain injury, 26% of these veterans had psychotic disorders (14% had paranoid schizophrenia). Researchers have found a correlation between TBI and a genetic predisposition to schizophrenia.
Many anxiety spectrum disorders can develop after traumatic brain injury (TBI). In a study of 66 patients with TBI, 11% of patients developed generalized anxiety disorder in addition to major depression. In a study that assessed 120 soldiers suffering from moderate to severe TBI, 9% of patients experienced a panic attack. In another study conducted on patients with TBI, 18% developed PTSD, 14% OCD, 11% panic disorder, 8% generalized anxiety disorder, and 6% phobic disorder.
TBI and substance abuse disorders are common.
Instrumental studies and neuromonitoring
Neuroimaging
Computed tomography (CT)
brain -
the “gold standard for diagnosis”
of traumatic brain injury, allows you to assess the condition of the brain matter and bones of the skull. The method is highly sensitive to detecting intracranial hemorrhages. It has sufficient accuracy to identify areas of contusion, signs of edema, as well as secondary infectious and ischemic injuries while monitoring the patient’s condition over time. There are small-sized devices that allow the patient to be assessed directly in the department, without the need for long transportation. CT can be performed without significant difficulties in patients on mechanical ventilation. A short scanning time (2-5 minutes) minimizes problems associated with psychomotor agitation and/or lack of patient cooperation.
According to the requirements of modern guidelines, a CT scan of the brain is indicated for all patients with persistent disorders of consciousness - with a Glasgow Coma Scale score of ≤14 points.
Magnetic resonance imaging (MRI)
brain - a more sensitive method for identifying areas of contusion without a hemorrhagic component. Based on the characteristics of intracranial hemorrhages in various modes, it allows us to judge their duration. It can be used when necessary to assess the dynamics of structural changes in the brain substance: atrophy, cysts, areas of gliosis, as well as in the diagnosis of infectious and secondary ischemic complications. Using functional research methods - functional MRI and positron emission tomography, it is possible to obtain objective data on the functioning of the brain, their results are used to distinguish between a vegetative state and a state of minimal consciousness.
Types of concussion
Head contusion refers to the primary consequences of head trauma resulting from direct exposure to a blast wave.
The result of an explosion of ammunition or explosives is the release of a large amount of energy in a short period of time. Under its influence, several moving zones with different pressures are formed in the atmosphere at once: at the epicenter of the explosion there is a region of compressed air, and behind it there is a rarefaction zone in which the pressure is significantly lower than atmospheric pressure.
If a person is in close proximity to an explosion, then his body is exposed to sudden changes in pressure, temperature and density of the environment, which has a negative impact on the physical condition of the internal organs of the body; the consequences of complications from the explosion include concussion in the brain, and this, as is known, threatens various complications in the organization of the central nervous system.
Experts distinguish several degrees of human brain contusion, characterized by certain abnormalities in brain function:
- I degree, mild. Immediately after injury, a brief loss of consciousness may occur. After the victim comes to his senses, headache, dizziness, ringing in the ears, increased heart rate and increased blood pressure are noted. After a few days, usually 1-3 days, these symptoms disappear without serious consequences, however, in order to avoid worsening the situation, the patient remains under observation for some time.
- II degree, average. It is characterized by a more prolonged loss of consciousness, severe headache, impaired body thermoregulation, the appearance of convulsions, ear and nosebleeds, and rapid breathing. Often the victim cannot remember the events that preceded the shell shock. All these manifestations of trauma can appear and disappear over several weeks, significantly complicating the life of the victim. Subsequent recovery of the body can be complete or partial.
- III degree, severe. There is a serious disruption in the functioning of the subcortical structures of the brain and the entire nervous system. The victim experiences a prolonged loss of consciousness (more than 3 weeks) up to coma, convulsions, amnesia, loss of hearing and vision. Such a patient needs to maintain the operation of life support systems. With a successful combination of circumstances, disability occurs, in the worst case – death.
Symptoms of concussion
Signs of concussion are similar to those characteristic of a concussion. A person may begin to bleed from the nose and ears, and hearing and speech function sharply deteriorates. With correct, timely treatment, the disorders are reversible. The recovery period may vary.
Symptoms of contusion:
- Pain in the head, dizziness, which intensifies when performing rotational movements of the head.
- Nausea, attacks of vomiting.
- Amnesia of retrograde and anterograde types.
- Visual and speech dysfunction.
- Hearing impairment that develops as a result of barotrauma - damage to organs that occurs due to the difference in pressure inside the body and in the external environment.
- Increased sensitivity to noise and loud sounds.
When there is an amplitude difference between external and internal pressure due to an explosion, damage to the hearing organs in military personnel is often manifested by rupture of the membrane, decreased hearing acuity, and malfunction of the vestibular apparatus. The internal organs of the upper body are damaged due to compression between the spinal column, chest bones and diaphragm.
The consequences of concussion can last for a long period of time and are expressed in increased fatigue, irritability, epileptic seizures, insomnia, and poor health. In people who have suffered a bruise of brain tissue, alcohol tolerance worsens. The dose required for intoxication is significantly reduced.
Types of pathology
To be contused in pathogenesis means to expose internal organs to the influence of inertial forces that arise within the body under the influence of external factors. As a result, organic changes occur in tissues. There are general and severe types of pathology. In the first case, disorders occur as a result of damage to large areas of the body and head. Severe contusion is accompanied by significant damage, ruptures and displacement of internal organs. Depending on the severity, they are divided into: mild, moderate and severe. Pathology of 2 and 3 degrees of severity is manifested by malfunctions in the functioning of all organs and systems.
Severe bruise
The word “concussion” itself comes from the Latin “contusio”, which is translated into Russian as “bruise”. The author of “The Beginnings of General Military Field Surgery,” the legendary Russian doctor Nikolai Pirogov, speaks of shell shock in exactly this sense.
Only during the Great Patriotic War did they begin to talk about shell shock in the sense in which we now know this expression. Contusion is a severe injury not to just one part of the body, as happens with bruises, but to the entire body. Moreover, this defeat must be the result of a powerful and instantaneous mechanical shock during an explosion, a fall from a great height, etc.
In a military context, concussion is one of the consequences of an explosion. After all, after it, explosive gases begin to rapidly expand. They powerfully hit the surrounding air and compress its layers. They become highly dense and compressed, while at the same time heating to high values.
These layers of air, being compressed, tend to expand. This puts pressure on the nearest layers of air, and they also begin to compress. At the moment, there is an abrupt increase in pressure, which spreads in the air at supersonic speed. As soon as the zone of highly compressed air reaches its limits, an area of rarefaction forms immediately behind it, where the pressure is much lower than atmospheric pressure.
Consequences
Sometimes the consequences of an injury may not appear immediately, but after several days, months or even years. Even some time after treatment, various symptoms may occur: dizziness, headaches, shortness of breath, high/low blood pressure, stuttering, depression, neuroses, phobias.
Often, even a mild form of contusion leads to delayed consequences in various areas of human health. One of the most common disorders are psychological disorders due to concussion.
Under normal conditions, it is almost impossible to get a cerebral contusion. Most often, the cause of concussion itself is psychologically traumatic for a person . For example, if it was received during military operations, then first of all one should expect such changes in human behavior as the appearance of aggression, depression, apathy, and an increased level of anxiety.
As a result of hemorrhage, cerebral edema, epilepsy, or even brain death may occur; in this case, a person’s life can be maintained artificially, but, in fact, he will already be dead. If damage occurs to the base of the skull or midbrain, this usually means instant death, because in that part of the brain the centers of instinctive regulation of the body are localized. A person will simply stop breathing or his heart will no longer beat, because signals from the brain will not arrive.
It is worth considering the location of the damage: which hemisphere is damaged, which gyrus, etc. If the occipital part of the cortex is damaged, disturbances may occur on the part of the visual analyzer; if the temporal lobes are damaged, hearing may occur; if the tissues of the parietal lobe are damaged, the center is disrupted - stereoagnosia (recognition of objects by touch).
One of the most common conditions after a concussion is asthenic syndrome . It manifests itself in chronic fatigue and drowsiness. Along with this, symptoms such as irritability, tearfulness, fatigue, and problems with concentration are observed.
Contusion is also characterized by the appearance of hysterical syndrome. Such patients are demonstrative, tearful, capricious, hypochondriacal, suspicious, react sharply and emotionally to any life difficulties, and are selfish.
Such patients are usually afraid of loud noises or places similar to the one where they were injured for the rest of their lives.
Treatment of concussion
When choosing treatment methods, the degree of tissue damage is taken into account. Treatment is usually conservative and involves taking medications. Additionally, if paresis and paralysis occur, physiotherapy, massage and physical therapy are prescribed. First aid for head bruises and contusions can be provided by eyewitnesses to the incident.
Medical care in a hospital setting includes measures to prevent the development of cerebral edema and other complications. In the treatment of pathology, antidepressants, sedatives, painkillers, and nootropic drugs are used. One of the effective treatment methods in the later stages is psychotherapy sessions.
Consequences and rehabilitation
Typically, the consequences of a brain contusion are minor, and the injury goes away without negative effects on the body. The person recovers quite quickly. If the injury is of moderate severity, there may be consequences, but usually without dangerous complications. The person makes a full recovery unless there is a skull fracture or hemorrhage. For a complete recovery, you must follow all doctor’s prescriptions and undergo rehabilitation.
The worst prognosis is for a patient who has suffered a severe brain injury. Patients who survive often experience the following consequences:
- epilepsy;
- acute inflammatory processes in the lining of the brain;
- colloid cysts;
- hydrocephalus with intracranial hypertension;
- the appearance of scars in the brain tissue or membrane;
- brain death.
In case of concussion, the consequences for the psyche are in any case unfavorable. The patient often has a headache, dizziness, irritability and aggression. In severe cases, the patient becomes insane.