Echoencephalography is a diagnostic neurophysiological study of the structure of the brain, aimed at identifying its pathological processes and changes. The method is non-invasive and requires the use of ultrasonic waves. Thanks to it, it is possible to determine intracranial pressure and identify volumetric processes due to which structures are displaced.
At the same time, it does not allow one to accurately determine the type of detected formations, therefore it is accompanied by computed tomography or magnetic resonance imaging. These are more accurate ways to make an accurate diagnosis.
Echo-EG of the brain involves scanning and calculations by a doctor. They are necessary in order to determine the parameters of the internal volume of the skull and the presence of displacements of brain structures, to identify an increase in intracranial pressure after injuries or due to neoplasms.
You can undergo an Echo-ECG in Moscow at the CELT multidisciplinary clinic. We have everything necessary to obtain all the necessary information and correctly interpret research data.
Echoencephalography of the brain (Echo-EG) - 1,200 rubles.
15 minutes
(duration of procedure)
Outpatient
Advantages of echoencephalography of the brain in CELT
We employ specialists with many years of experience, allowing them to carry out diagnostic studies as accurately as possible and obtain all the necessary data. They have modern equipment in their arsenal that allows them to get a complete picture. Thus, Echo-EG of the head in our clinic allows:
- identify neoplasms in the early stages of their development;
- conduct a qualitative study of the midline structures and periosteal space;
- determine ICP indicators and the nature of pulsations;
- minimize the human factor and increase diagnostic accuracy.
You can find out the price of Echo-EG in our clinic in the corresponding section of our website or by calling us!
Indications for testing
Doctors refer for ECHO of the head for the following pathologies:
- Neoplasms are malignant and benign.
- Tuberculosis, ischemia, cerebral infarction.
- Encephalopathy.
- Swelling, abscess.
- Shaking paralysis.
- Tumor of the anterior pituitary gland.
Two-dimensional echoEG is necessary for:
- Traumatic brain and neck injuries.
- Migraines.
- Noise, ringing in the ears.
- Head spinning.
- Headache attacks.
- Shell shock.
- Acute cerebrovascular accident.
- Vascular or hypertensive encephalopathy.
- Vertebro-basilar syndrome.
- Increased intracranial pressure.
- Necrotic processes in the brain.
- Vegetative-vascular dystonia.
- Poor circulation due to damage to the vertebral artery.
Indications for ultrasound echoencephalography
The study is carried out as part of primary neurological diagnosis when the patient complains of:
- headache;
- constant feeling of nausea;
- frequent loss of consciousness;
- feeling of pressure on the eyes;
- incessant noise in the head;
- disturbances in concentration and memory.
The indication for this is an increase in ICP or the need to measure it, suspicion of the presence of neoplasms, foreign objects, cysts and hematomas in the cranial cavity if computed tomography and magnetic resonance imaging are not available. The study is carried out if necessary:
- confirm the presence of diseases such as epilepsy, brain damage of a degenerative, vascular or inflammatory nature;
- identify the patient’s simulation of hearing and visual impairments;
- assess the brain functioning of comatose patients;
- determine the cause of sleep disturbances and abnormal surges in blood pressure;
- determine the efficiency of functioning of blood vessels and tissues.
Features of the technique
Echo ES, otherwise called echoencephaloscopy by specialists, is a modern method of instrumental examination of brain structures. The study is carried out quickly and does not require any effort on the part of the patient or the introduction of a contrast solution. Therefore, no harm is caused to human health.
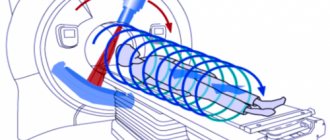
The procedure itself is non-invasive; there is no opening of the skull bones. The study is based on the ability of ultrasound waves to bounce off brain tissue.
Typically, wave frequencies in the range of 0.5–15 MHz/s are used.
In this case, the image may differ due to the fact that different constituent elements of the brain reflect ultrasound in their own way - blood, blood vessels, bone and brain tissue.
To carry out the procedure, special sensors are placed on a person’s head, which transmit and record reflected brain signals.
Duration of the study – no more than 20-30 minutes.
During this period, thanks to manual and computer processing, the doctor receives information: the symmetry of the location of structural units, the dimensional volumes of the ventricles, the presence of foreign formations.
The study can be carried out in two modes - obtaining a graphic or flat image on the screen. The best option is determined by the doctor individually.
Indications for use
Examination of the head space - Echo Es, as doctors' practice shows, is more accurate due to the fact that there is no air inside the skull. The specialist sees different parts more clearly, so with the help of echoencephaloscopy it is possible to distinguish between congenital and various acquired diseases at an early stage of their formation.
Indications for echo examination:
- headache - frequent and prolonged attacks of discomfort in various parts of the head, practically resistant to analgesics;
- neurological symptoms that do not correspond to any one pathology;
- suffered traumatic brain injuries;
- persistent dizziness for no apparent reason;
- various neurotic reactions - for example, enuresis, tics;
- hyperreactivity or attention deficit syndrome in a child;
- consequences of perinatal trauma;
- sleep disorders;
- increased muscle tone of unknown etiology.
The doctor will finally determine the need for an echo examination after collecting an anamnesis of the disease - when and under what circumstances the person felt a deterioration in health, as well as based on the results of a neurological examination.
Diseases requiring echo procedures
In most cases, Echo ES is used by doctors to clarify the diagnosis when the following diseases are suspected:
- Pathologies accompanied by a failure of intracranial circulation: coronary artery disease - blockage of blood vessels with cessation of nutrition in a separate area of the brain.
- Neuroendocrine disorders: Parkinson's syndrome, Farah's disease, Alzheimer's disease, multiple system atrophy.
- Pathologies associated with the accumulation of cerebrospinal fluid in the ventricles of the organ: hydrocephalus - enlargement of the ventricle due to overcrowding with fluid, failure of the venous outflow from the skull.
- Volumetric neoplasms: consequences of traumatic brain injuries - hematomas, cysts, abscesses, tumors.
However, when deciphering the results of the study, the “human” factor should be taken into account - a diagnostic specialist and a neuropathologist may evaluate the image on the device differently, based on personal experience. In some cases, other additional examinations are recommended, for example, computed tomography with intravenous enhancement with a contrast solution.
Research stages
The Echo Es procedure itself is simple - performing all stages does not require special training from the diagnostician. Difficulties will arise when evaluating the resulting images.
The room where echoencephaloscopy is performed is a very ordinary room, in which you only need an outlet to connect the device to the mains.
In some cases, it is possible to conduct an examination at the patient’s home.
The position of a person’s body does not have a significant impact on the result - you can lie down or sit . The main stages of obtaining Echo Es:
- taking anamnesis - duration of pathological symptoms;
- examination of the skull - whether there are deformations on it, noticeable asymmetries in areas;
- applying a special solution to the sensors that increases the tightness of contact with the skin, creating an acoustic signal.
Echo examination can be carried out in two modes:
- with the application of two sensors on the head, with their fixation on the skin of the temporal part of the skull opposite each other - the transmission method;
- using one sensor, which is applied alternately to one or another part of the skull - the emission method.
As a rule, an experienced diagnostician performs an ultrasound several times, gradually changing the angle of the sensors to obtain the clearest and most informative images.
Preparation rules
Despite the simplicity of the echo procedure, you should properly prepare for the study. Experts point out that to obtain information about the functioning of the brain, you will not need to change your diet or take medications.
However, the reliability of the result may be affected by:
- sleep disturbance – it is recommended to get a good night’s sleep the night before the examination;
- hunger – on the day of the diagnostic visit, a light breakfast is necessary;
- stress – the procedure is absolutely painless, so no need to worry;
- bad habits - doctors advise to refrain from abusing tobacco and alcohol products.
In addition, you should be prepared that for some time, while the specialist performs ultrasound diagnostics, you will need to keep your head and body still in order for the result to be accurate and informative. Therefore, echoencephaloscopy in young children is performed in the presence of parents who hold their heads in the desired position.
If there are damage to the scalp, even superficial to the skin, they can distort the ultrasonic waves. The study must be postponed until the wounds have healed or resort to other techniques that allow such tissue defects.
Result evaluation
Each structure of the brain, from a small vessel to the bones of the skull, reflects ultrasonic waves in its own way. The procedure for obtaining an echo image on the device screen is based on this. Decoding the result is a comparison of information from quantitative indicators. Both the distances between groups of signals and their total number are measured.
It is customary to distinguish 3 groups of signals:
- formed in the vicinity of the ultrasound sensor - they are reflected from the tissues and bone elements of the skull, as well as the cerebral cortex with the formation of the initial complex;
- reflection of ultrasound waves from the hemispheres - the central complex of signals;
- reflection of impulses from brain tissue and cranial bones, but from the side opposite to the sensor.
In a healthy person, the length of the initial and final complexes is identical. If Echo ES moves more than two millimeters, then it is assumed that a space-occupying formation has formed in the hemisphere opposite to the sensor - a hematoma, neoplasm, cyst.
Whereas interhemispheric asymmetry is revealed due to the different number of echo signals from the left as well as the right hemisphere. The cause of such a failure can be both cerebral hydrocele and malignant neoplasm.
Disadvantages of the method
Echoscopy has such a significant disadvantage as the insufficient accuracy of the technique for small defects in the structures of the brain - for example, at the initial stage of the formation of a cyst or hematoma.
Therefore, if the results of the study are questionable, doctors necessarily insist on conducting more accurate modern methods for diagnosing brain diseases - computer or magnetic resonance imaging.
The procedure is not advisable in the acute period after traumatic brain injury , since the outcome of the examination is influenced by external injuries, as well as significant swelling of the integumentary tissues of the head. In addition, the experience of the diagnostic specialist also plays a role. So, if the study is carried out on a small child who behaves restlessly, the image loses clarity.
Contraindications to echoencephalography in M-mode
Echoencephalography of the brain in children and adults is a safe procedure. It does not require the use of painkillers (or any other pharmacological drugs) and has no physiological contraindications. However, it should be postponed during acute respiratory diseases accompanied by a runny nose and/or cough. It is not used if the patient has open wounds or suffers from psychological disorders in the areas where the sensors need to be installed. The latter can cause hysterics due to the unfamiliarity of the situation.
How to properly prepare a child for research?
Without preliminary preparation, the research procedure may cause fear in young children due to the specific preparatory manipulations performed. Therefore, it is recommended that parents prepare their baby in advance. Young children can be prepared in a playful way, for example, by telling the child that he will try on the helmet of an astronaut, pilot or superhero. Older children need to be explained in detail how the EEG procedure will be performed, even shown if possible. With such preparation, children come for diagnostics with pleasure and are not afraid of anything, which guarantees a successful recording of the study.
Preparation for the procedure and its implementation
One- and two-dimensional echoencephalography does not require the patient to prepare independently. All he needs to do is visit the diagnostic room at the appointed time. Before starting the examination, the diagnostician will ask him to remove from his head any accessories that may interfere.
During the process, the doctor installs an ultrasound sensor in certain areas of the head. To ensure high-quality contact, a contact gel is first applied to them. This prevents air from entering and causing interference. The sensor is placed:
- above the ear canals;
- near the outer edges of the eyebrow arches (at the temples);
- behind the ears at a distance of four to five centimeters.
By sending ultrasound signals, the sensor catches them in reflected form and transmits them to the device, which displays them on the monitor in the form of a graphic image similar to the teeth of an electrocardiogram.
When carrying out the procedure in a two-dimensional format, the sensor is not rearranged sequentially - it is moved along the surface of the head, providing an image of the slice in a horizontal plane along the line of its movement. An image of the formations located at this level is displayed on the screen. The duration of the procedure is no more than 15 minutes.
Who is prescribed this test?
Due to the fact that m-echo is only part of an ultrasound examination, not all ladies know why exactly they need this indicator. Meanwhile, m-echo data is necessary for women of any age.
- In the reproductive period, m-echo allows you to assess readiness for conception and successful gestation.
- In premenopause, a study is carried out to exclude the formation of adhesions.
- During menopause, the procedure is recommended for all women every year, since it is at this age that the risk of cancer of the uterine body increases several times.
Decoding echoencephalography of the brain
The results of the diagnostic study are interpreted by a neurologist. As already mentioned, the norm provides for the same distance from the central signal to both sides. The permissible deviations are no more than two millimeters for adults and three for children.
During volumetric processes in the GM substance, a shift in the central signal occurs, changes in the shape and duration of responses. Thus, the following pathological conditions can be identified:
- intracranial neoplasms of benign and malignant etiology;
- tuberculomas;
- hematomas localized in the intracranial space;
- cerebral infarctions;
- focal accumulations of pus in the GM substance;
- syphilitic granulomas.
Their localization is determined by median deviations. The distance to the central signal on the side of the formation is greater than on the healthy side, although in certain inflammatory diseases and stroke the opposite may be true. A similar phenomenon can be triggered by a decrease in the volume of one hemisphere during recovery processes, when scarring or resorption is observed.
The doctor determines the presence of a problem based on echo-EG readings:
- with tumors of malignant etiology, a serious shift is observed;
- infarction states of the brain are characterized by small transient changes;
- in case of traumatic injuries, displacements of no more than three millimeters are observed due to swelling;
- hydrocephalus is characterized by expansions of the central signal from five minimeters and the appearance of a large number of lateral ultrasound signals;
- suspicion of hemorrhage arises with the most serious asymmetry.
It is important for patients to understand that the diagnostic accuracy of this method directly depends on the qualifications and experience of the specialist, as well as on the characteristics of the device involved in the process.
Make an appointment with our specialists by filling out and sending us an application online or by calling us by phone! Trust the diagnostics to professionals!
Normal m-echo of the uterus
During menopause, the m-echo indicator should not be more than 0.5 cm. On average, the normal endometrial thickness for women in the reproductive period of life does not exceed 1.5 cm. However, an ultrasound examination evaluates the m-echo norm depending on the phase of the menstrual cycle.
If we take an average 28-day menstrual cycle, then in the first 2 days the thickness of the outer layer of the uterus ranges from 0.5 to 0.9 cm. Over the next couple of days, the value decreases from 0.3 to 0.5 cm. The end of bleeding is marked by an increase in data from 0.6 to 0.9 cm. This is followed by a period of increasing layer thickness up to the 14th day (presumed ovulation) - at this time the indicator reaches 1.3 cm. After this, a rapid thickening of the endometrium occurs, so until the 23rd day of the cycle its thickness can reach 2.2 cm. By the end of the cycle, the layer becomes a couple of millimeters thinner - about 1.8-2 cm.
What is the essence of the procedure
Echoeg is based on ultrasonic waves, which, upon reaching the tissues, are reflected and recorded by sensors. Sensor plates are placed on the patient's head. They form ultrasound, spreading to the structures of the brain and skull. When the signal reaches the interface between the brain and the skull, or between the ventricle and the medulla, it undergoes echolocation and is reflected back. The returned waves are recorded by sensors, and an image of the structures appears on the computer screen. An echoencephalogram is a picture that shows reflected waves.
In the human body, each tissue has its own acoustic resistance: it reacts differently to ultrasonic waves. For example, dense bone tissue produces one type of reflected signal, while tumors and cysts produce another. Echoencephaloscopy is based on this property of tissues, thanks to which the diagnostician determines healthy and diseased areas of the brain and skull.
The examination of the skull and brain is carried out using ultrasound with a frequency of 2 to 20 MHz. This is too little to potentially cause harm to the body of a child and an adult. Ultrasound energy is too low to somehow change the state of a biological object.
The impulse is formed in the following successive stages:
- Initial complex. The frequency of the sent wave is determined.
- M-echo. Echo is the main signal formed during the passage of dense and liquid structures.
- Ultimate complex. The signal bounces off the bony wall of the skull on the opposite side.
- Lateral signal. This is the difference between the sent signal of the first sensor and the received signal in the second.
Echo examination of the brain has several negative aspects:
- In comparison with modern methods (MRI, neurosonography) it has a low diagnostic value.
- Shows only a ready-made picture of the disease, without the possibility of establishing its cause.
What diseases are detected
An ultrasound with determination of the endometrial indicator can reveal:
- hyperplasia;
- hypoplasia;
- cancer.
Hyperplasia is a benign pathological process. In this case, the endometrium grows. The walls thicken and the volume increases. With hypoplasia, the endometrium does not grow enough. Women with menopause usually face cancer. It is important to correct the deviation in a timely manner.
It is worth noting that deviations from the norm do not always indicate disease. That is why only an experienced doctor should decipher the results.
What pathologies does the examination reveal?
Uterine echography is the only non-invasive method for diagnosing endometrial pathologies.
The following conditions are common:
- Hyperplasia is excessive growth of the inner mucous membrane of the uterus. Due to increased proliferative processes, the mass and thickness of the endometrial layer increases. The pathology is classified as benign neoplasia, not prone to malignancy. However, hyperplasia can cause menstrual irregularities, abnormal uterine bleeding and infertility.
- Hypoplasia is atrophy, causing a decrease in the thickness and mass of the mucosa. More often, changes are associated with age-related involution or hormonal imbalance.
- Uterine cancer is a malignant process characterized by the formation of poorly differentiated cells. Despite the seriousness of the disease, if treatment is started in a timely manner, it has a relatively favorable prognosis and the possibility of achieving stable remission.
- Endometriosis is a common disease in which endometrial cells grow beyond the inner layer of the mucous membrane. With timely diagnosis, it has a favorable prognosis.
In addition to identifying endometrial pathologies, M-Echo is a mandatory study when planning pregnancy. This procedure helps assess the readiness of the endometrium for implantation of the embryo.
For implantation of the fertilized egg, the thickness of the mucosa must be 11–14 mm. Thin, atrophic endometrium is not able to hold the embryo on the uterine wall. Excessive growth of the inner membrane significantly increases the risk of rejection of the fertilized egg.
In addition to the size of the endometrium, its structure is of great importance. The loose and spongy layer, rich in blood vessels, promotes implantation and growth of the embryo.
In the video, endometrial disease: