Ependymoma is a brain tumor that develops when the cells lining the surface of the brain ventricles mutate. Refers to the primary formations of the central nervous system; it can have a benign or malignant course. Most often localized in the posterior cranial fossa or the region of the lateral ventricles, it grows slowly, but is capable of penetrating into adjacent brain structures. Brain ependymoma is dangerous because it can go unnoticed for a long time, and the first signs of the disease appear when the tumor has reached a large size or has metastasized. The main approach to treating a tumor is an integrated approach, which consists of resection of the tumor followed by chemotherapy and radiation therapy. Why does pathology develop, what are its symptoms and what treatment gives a positive prognosis?
Causes of brain ependymoma
What serves as a prerequisite for the development of a tumor is unknown, but still there are several factors that can influence the development of pathology:
- heredity;
- long-term use of potent drugs;
- ionizing radiation;
- trauma to the skull or central nervous system;
- oncogenic viral diseases (human papillomavirus, herpes);
- poor environmental conditions;
- smoking and alcohol abuse.
The cancer trigger was initially thought to be the SV40 virus, which was discovered in ependymoma cells. However, subsequent studies did not confirm this theory, so the etymology of the disease is still unknown. As practice shows, cerebral ependymoma most often occurs in children and adolescents, less often in adults.
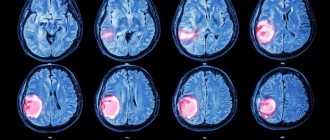
Contrast enhancement
Fig.583-585
Heterogeneous accumulation of the contrast agent in the tumor stroma, as well as contrast adsorption along the walls of the tumor cyst, reflecting the presence of tumor cellular elements in it (Fig. 583-588).
Fig.586-588
Symptoms
Unlike other types of brain tumors, ependymoma is rare. Cancer cells can have different levels of malignancy. Some tumors grow slowly, while others grow quickly, compressing surrounding vessels and tissues, causing characteristic symptoms.
Clinical signs of ependymoma directly depend on the location and size of the formation. As with other types of cancer, in the early stages it does not cause obvious symptoms and only as the tumor grows do the symptoms become more noticeable and, in some cases, severe.
The main signs of the disease are blurred vision and hearing, convulsions, difficulty swallowing and speech impairment, which are manifested as a result of increased intracranial pressure. Other characteristic symptoms include:
- headache of a bursting or aching nature;
- dizziness;
- impaired coordination of movements;
- unsteady gait;
- tremor of the limbs;
- chronic fatigue;
- a sharp decrease in body weight;
- nausea, urge to vomit;
- memory loss;
- sudden change of mood;
- “floaters” or “fog” before the eyes;
- convulsions, numbness of extremities;
- difficulty swallowing.
Symptoms depend on where the formation is located. If the tumor is located in the cerebellum, balance and gait will be affected. Its location in the cerebrum causes seizures. The presence of a formation in the spinal cord - numbness of the face, disturbances in the functioning of the digestive system. The exact location of cancer can only be recognized with the help of comprehensive diagnostics, which is prescribed by a doctor if an oncological process is suspected.
Signs of the disease
When the tumor expands, the following symptoms appear:
- progressive pain in the head;
- feeling of pressure on the eyes;
- nausea and vomiting, independent of food intake;
- irritability, behavioral changes;
- loss of coordination control, unsteadiness of gait;
- violations of fine motor skills (the patient loses the ability to write accurately and quickly);
- decreased level of memorability;
- impairment of auditory (hearing loss) and visual perception (double vision).
With subsequent growth of ependymoma, the cerebrospinal fluid channels may become blocked, hydrocephalus develops, internal pressure increases, and the described symptoms tend to worsen. The pain syndrome increases in intensity and is not relieved even by strong analgesics; vomiting does not stop and does not bring relief. Systematic seizures are often found in the pediatric clinical picture.
Types of ependymoma
In oncology, ependymomas are divided into 4 main stages, which differ in the level of benignity and developmental features:
- Myxopapillary (papillary) is a benign tumor that is localized in the conus of the spinal cord and is characterized by slow growth. With timely treatment, it has a good prognosis. Refers to the first stage of malignancy, since there is a risk of its degeneration.
- Subependymoma - develops from subependymal glia. Externally it has the shape of a node and is located in the ventricular system of the brain. As in the first case, it develops slowly and has a good prognosis.
- Classic ependymoma is the most common type of tumor, which is localized in the ventricles of the brain. It often relapses and can degenerate into malignant cancer. It has 2 degrees of malignancy.
- Anaplastic ependymoma is a severe form of cancer with a poor prognosis. Characterized by rapid growth and metastases. Refers to stage 3 oncology.
The last 2 stages of the disease are considered the most dangerous, since even with surgery and therapy they are capable of relapses and metastases. According to the localization of the tumor process, it is divided into:
- supratentorial - the location of the tumor is diagnosed above the cerebellar tentorium. Such ependymomas are formed outside the ventricles of the cerebral hemispheres, have a nodular shape, a bumpy or smooth surface, and can fill all the cavities of the ventricles.
- infratentorial - located in the posterior cranial fossa, often affecting the brain stem and fourth ventricle.
Cancerous tumors in brain structures, regardless of location, should be diagnosed in a timely manner, this increases the chances of a positive prognosis from treatment.
Ependymomas grow slowly compared to other cancers, but they are capable of displacing tissue in the brain or spinal cord, but not growing into them. Such cancer cells rarely metastasize beyond the central nervous system. In the case of grade 3 malignancy and surgery is performed, a new focus of formation appears at the local level (close to the original process).
Table of contents
- What are ependymomas?
- Where do ependymomas grow and how do they spread throughout the central nervous system?
- How common are ependymomas in children?
- What are the histological types of ependymomas?
- Why do children get ependymoma?
- What are the symptoms of the disease?
- How is ependymoma diagnosed?
- How is a treatment plan made?
- How is ependymoma treated?
- What protocols and registries are used to treat children?
- What are the chances of being cured from ependymoma?
- Additional Information
Diagnostics
To diagnose brain ependymoma, you need to consult a neurologist. The specialist will examine the medical history in detail and prescribe a number of tests and studies:
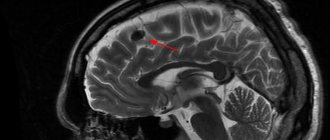
- MRI is an informative examination method that allows you to accurately determine the size and location of the tumor, its structure, and shape.
- CT scan – determines the focus of the disease, reveals whether there are metastases to other organs and systems.
- Electroencephalography – examines the functioning of the blood vessels in the brain.
- Ophthalmoscopy - the procedure consists of examining the fundus, assessing the optic nerve and retina.
- Angiography is performed using contrast to assess the condition of the blood vessels in the brain.
- A biopsy is a procedure that allows you to determine the type of tumor. During the process, tumor tissue is collected and then tested in the laboratory.
The examination results allow the doctor to obtain a complete picture of the disease. If necessary, the doctor prescribes a consultation with doctors from other areas of medicine: ophthalmologist, otolaryngologist, psychologist. Comprehensive diagnostics is the basis for making a final diagnosis and determining further treatment tactics.
Diagnosis
Ependymomas are diagnosed using imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI). If a child is admitted to the emergency department, they will first have a CT scan. A CT scan uses X-rays to take a series of pictures of the brain from different angles. Before the CT scan is performed, the child may be given intravenous contrast or anesthesia. CT scans are very quick, but young children may need to be sedated to lie still during the test. If a CT scan shows a possible tumor, the child is given an MRI to confirm the diagnosis. It provides clearer images for diagnosing ependymoma. MRI scans use magnets to take detailed pictures of the brain from different angles. A chemical called gadolinium is injected into a vein before an MRI to help certain parts of the brain show contrast.
note
The MRI takes several hours and the child must lie still the entire time. Therefore, medications are used to keep children asleep during the study period.
On MRI, ependymoma is visible due to contrast. The tumor is usually located along the ventricles and may extend through the openings between the ventricles. There may also be evidence of obstructive hydrocephalus on MRI due to blockage of CSF flow by the tumor.
While most ependymomas are localized, sometimes tumors can spread to other parts of the brain or spine. Children with ependymomas usually have an MRI of the spine to make sure there is no tumor along the spine. Children usually also require a lumbar puncture to look for tumor cells in the cerebrospinal fluid. A lumbar puncture is a small needle inserted into the lower back to obtain a sample of cerebrospinal fluid. A specially trained doctor, a pathologist, will look at cells from the cerebrospinal fluid under a microscope to see if the tumor has spread.
Although ependymomas are usually detected on MRI, the diagnosis cannot be officially made until a biopsy or surgical removal of the tumor is performed. A biopsy is when the surgeon takes a small piece of tissue from the tumor. The pathologist will look at the tumor cells under a microscope to determine the type of tumor.
Treatment of brain ependymoma
Modern oncology and neurosurgery has the latest equipment for the diagnosis and treatment of brain tumors. Research Institute of Neurosurgery named after. Burdenko is one of the few where complex operations to remove ependymoma are performed. The clinic employs a team of high-level doctors who, over several years, have performed many complex operations to remove tumors from brain structures. The oncology center is equipped with modern equipment for diagnosis and treatment. An integrated approach and an affordable price allow us to consider the Burdenko Clinic one of the best in Moscow.
To get a full consultation and detailed information about treatment at the Burdenko Clinic, you can go to the website of the neurological center, where all the necessary information for patients is provided. The cost of treatment at the oncology center is calculated individually for each patient. If a person is unable to pay for treatment, the clinic has a quota for free treatment.
Considering that brain ependymoma has a high degree of malignancy, therapy is most often complex, consisting of surgery and radiation therapy. Chemotherapy treatment is carried out only if surgery is not possible. This treatment of ependymoma does not give a good prognosis; it can only prolong the patient’s life by several months.
I consider surgery to be the optimal method for treating such a tumor. It is performed using microscopic technology, which allows intervention into brain structures with minimal risk to health and the highest accuracy. During the operation, there is often a need for craniotomy. This allows access to the tumor and its complete or partial excision. Removing brain ependymoma does not provide a 100% guarantee for the complete destruction of cancer cells, so surgery is often combined with radiation therapy. The procedure has a detrimental effect on cancer cells that could not be eliminated by surgery.
Stereotactic radiosurgery, which involves exposing tumor tissue to radioactive rays, is often used to destroy tumor cells. Thanks to this technique, it is possible to stop tumor progression and destroy cancerous tissue, without affecting the healthy membranes of the brain.
Treatment of ependymoma in the clinic takes a long time, since the patient, even after the operation, must be under medical supervision. After therapy, the patient requires rehabilitation, which includes diet therapy, consultation with a speech therapist, psychologist, and therapeutic exercises. The recovery period may take several months.
Considering the complexity of the operation and intervention in the structures of the brain and central nervous system, there are always risks of postoperative complications. They can manifest themselves in the form of neurological disorders - seizures, loss of memory, vision and hearing. Sometimes patients learn to speak, read and write again. They require constant care and examinations. Medical supervision after surgery allows you to monitor the dynamics of the disease, the appearance or absence of relapses. In case of complications, the patient is prescribed special restorative therapy to eliminate symptoms and improve the patient’s quality of life.
Any tumor in the brain, regardless of whether it is malignant or benign, requires immediate treatment, since even a small tumor can have a negative impact on the functioning of the body and a person’s well-being.
What protocols and registries are used to treat children?
In Germany, almost all children and adolescents with ependymoma or recurrence of these types of tumors are treated according to standardized protocols called therapy optimization studies and treatment registries.
German protocols, or therapy optimization studies, are clinical studies and are strictly controlled. Their goal is to treat sick children using the most modern developments. At the same time, these studies provide an opportunity to improve treatment approaches and thereby achieve progress in treatment.
Children who are not treated according to the research protocol (for example, if at the time of illness the old protocol was closed and a new one has not yet opened; or if the form of the child’s illness does not meet the criteria described for admission to the current protocol), go through treatment registries . Treatment registries are created and operate in order to advise all patients from modern scientific positions. To ensure high quality of treatment, the research team for a particular protocol typically develops detailed therapeutic recommendations. And when attending physicians contact them, they advise them on choosing the optimal therapy for each individual child.
In Germany, at the end of 2011, the long-term protocol HIT 2000 (study of optimization of therapy for children and adolescents with ependymoma) completed its work. Numerous children's clinics throughout Germany and Austria have used this protocol. SIOP Ependymoma II protocol, is currently under development . The new protocol should begin work in 2015. Then sick children from Germany will be taken for treatment under this protocol.
Currently in Germany they work according to the following protocols and registers:
- HIT 2000 Interim Registry (abbreviated as I-HIT-MED): Children with ependymoma who are currently or in the future unable to be treated under a clinical trial protocol, or who refuse to be treated as required by a clinical trial, are enrolled in a therapeutic registry (HIT 2000 Interim Register). / register I-HIT-MED). These children receive an individual treatment plan, that is, depending on the specific form of the disease. Therefore, experts have drawn up therapeutic recommendations, based on the HIT 2000 protocol. These therapeutic recommendations can be used by all doctors in Germany. The registry is managed by the research office HIT-MED, which is located in the pediatric clinic at the University Hospital of Hamburg (the head of the research group is Prof. Dr. Stefan Rutkowski).
- HIT-REZ 2005 protocol: Another treatment optimization study is the HIT-REZ 2005 protocol (part of the E-HIT-REZ 2005 trial), which treats children with recurrent ependymoma. The central research office is located at the Center for Pediatric and Adolescent Medicine at the University Hospital Essen (headed by Prof. Dr. Gudrun Fleischhak). Please note: this protocol no longer accepts new patients as of January 1, 2013. New patients with relapse are treated according to the therapeutic recommendations developed by the central research office. These recommendations are based on the E-HIT-REZ 2005 protocol. A therapeutic registry should be opened for these children in the near future.
Prognosis after surgery
Life after treatment for ependymoma largely depends on the stage of the disease. If the disease is diagnosed in time and treated appropriately, the survival rate for more than 5 years is 70%. A less favorable prognosis is present with an anaplastic tumor, which can grow rapidly and metastasize. In this case, the chances of life are not great, and the treatment provided will prolong life by 1 - 2 years. If surgery is not possible, supportive care may increase life expectancy by just a few months.
If the operation fails to completely remove the tumor, there is always a risk of its recurrence. In such cases, the prognosis worsens, and the risk of its metastases to other organs and systems increases significantly. Unfortunately, there are no preventive measures that can protect against brain cancer. However, if you follow some rules, you can reduce tumor formation:
- proper and healthy nutrition;
- rejection of bad habits;
- eliminate the effects of radiation on the body;
- undergo regular medical examinations;
- monitor the state of the immune system.
By following basic rules, you can significantly reduce the risk of any cancer. Ependymoma is a type of brain cancer that requires timely diagnosis and quality treatment. By treating this pathology in the early stages of the disease, the chance of a positive prognosis is quite good, and the patient himself has the opportunity to return to a full life.
Bibliography:
- Timmermann B: Die Protonentherapie. Chancen zur besseren Verträglichkeit der Tumorbestrahlung bei Kindern. Wir 2010, 1: 33 [URI: https://www.kinderkrebsstiftung.de/ servicenavigation/ presse/ zeitschriften/ wir/ wir-einzelansicht/ article/ zeitschrift-wir-12010.html] TIM2010
- Kaatsch P, Spix C: Registry - Annual Report 2008 (Jahresbericht 2008 des Deutschen Kinderkrebsregisters). Technischer Bericht, Universität Mainz 2008 [URI: https://www.kinderkrebsregister.de/ extern/ veroeffentlichungen/ jahresberichte/ jb2008/ index.html] KAA2008a
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P: The 2007 WHO classification of tumors of the central nervous system. Acta neuropathologica 2007, 114: 97 [PMID: 17618441] LOU2007
- Kühl J, Korinthenberg R: ZNS-Tumoren. In: Gadner H, Gaedicke G, Niemeyer CH, Ritter J (Hrsg.): Pädiatrische Hämatologie und Onkologie. Springer-Verlag 2006, 777 [ISBN: 3540037020] KUE2006
- Timmermann B, Kortmann RD, Kühl J, Rutkowski S, Dieckmann K, Meisner C, Bamberg M: Role of radiotherapy in anaplastic ependymoma in children under age of 3 years: results of the prospective German brain tumor trials HIT-SKK 87 and 92. Radiotherapy and oncology 2005, 77: 278 [PMID: 16300848] TIM2005
- Gutjahr P: Tumoren des Zentralnervensystems, in: Gutjahr P (Hrsg.): Krebs bei Kindern und Jugendlichen. Deutscher Ärzte-Verlag Köln 5. Aufl. 2004, 373 [ISBN: 3769104285] GUT2004a
- Timmermann B: Therapie von Ependymomen im Kindesalter - Eine aktuelle Übersicht. WIR Informationsschrift der Aktion für krebskranke Kinder eV (Bonn) 2002, 4: 21 [URI: https://www.kinderkrebsstiftung.de/ fileadmin/ KKS/ files/ zeitschriftWIR/ 2002_4/ behandlungsnetzwerk08.pdf] TIM2002a
- Kaatsch P, Rickert C, Kühl J, Schuz J, Michaelis J: Population-based epidemiologic data on brain tumors in German children. Cancer 2001, 92: 3155 [PMID: 11753995] KAA2001
- Timmermann B, Kortmann R, Kühl J, Meisner C, Bamberg M: Combined postoperative irradiation and chemotherapy for anaplastic ependymomas in childhood: results of the German prospective trials HIT 88/89 and HIT 91. Int J Radiat Oncol Biol Phys 2000, 46: 287 [PMID: 10661334]TIM2000
Ependymomas (summary in PDF format) (350KB)
Forecast
After tumor treatment, the patient will be closely monitored to monitor for cancer recurrence, help manage ongoing side effects, and assist with rehabilitation. Children who have had ependymoma will be closely monitored with MRI for many years to assess whether the tumor is in remission. This is usually done every 3 months for the first 1 to 2 years after treatment, and then every 6 months for the next 3 years.
Alena Paretskaya, pediatrician, medical columnist
1,399 total views, 1 views today
( 49 votes, average: 4.41 out of 5)
Follicular thyroid cancer
Adrenal tumors: symptoms, diagnosis, treatment (removal)
Related Posts
Complications
It is possible for a child to have a recurrence of ependymoma, then the best approach is to surgically remove the recurrent tumor, if possible. Additional radiation is often also suggested. The most common site of ependymoma recurrence is the site of the primary tumor. Recurrent disease is often curable. Sometimes radiation for recurrent ependymoma should include the entire brain and spine, but not always. Even when recurrent ependymoma cannot be cured, a combination of surgery, chemotherapy, or radiation therapy may help the child reduce symptoms and improve quality of life.