Among all tumors in the central nervous system, spinal cord lesions account for approximately 12% in adults and about 5% in children. What is the cause of these pathologies and how are they treated?
ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists ALEXANDER SERYAKOV MD, professor, oncologist, hematologist, radiologist (radiation therapist) of the highest category, leading oncologist of the SM-Clinic holding »
Most often, tumors localized in the spinal cord are detected in people aged 30 to 50 years. Mostly, in about 85% of cases, they affect the membranes of the brain and surrounding structures.
What is a spinal cord tumor
“Spinal cord tumors,” says oncologist Alexander Seryakov, “are pathological neoplasms of a malignant and benign nature that are localized in the spinal cord.
They are rare. By location there are:
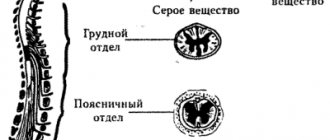
- intramedullary (18 - 20% of cases) - grow inside the spinal cord;
- extramedullary (80 - 82% of cases) - located near the spinal cord, developing from nearby tissues.
Among benign lesions, the most common are ependymoma (63%) and astrocytoma (30%). Much less common are non-malignant hemangioblastoma and malignant oligodendroglioma.
Causes of spinal cord tumors in adults
The true causes of tumor growth that occurs in the spinal cord have not been determined to date. Scientists have identified a number of risk factors that may increase the likelihood of tumor growth in children or adults, but definitely do not lead to the formation of pathology. These include:
- hereditary predisposition (features of genes passed on from parents to children);
- exposure to substances with carcinogenic effects (chemical dyes, petroleum products);
- development of lymphoma (this is a malignant lesion in the lymphatic system);
- the presence of Hippel-Landau disease (a tendency to grow tumors, both benign and cancerous, is inherited);
- development of neurofibromatosis type 2 (this is a disease associated with gene breakdowns in which multiple tumors are formed - schwannomas or meningiomas in the area of nerves and the nervous system);
- exposure to harmful environmental factors (chemical pollution, radiation exposure);
- maintaining an unhealthy lifestyle - smoking, drinking alcohol, poor nutrition;
- constant stress;
- a sharp decrease in immunity;
- Excessive tanning (in a solarium, on the beach).
Often several factors influence at once and special conditions must be created for the tumor to begin to grow.
Reasons for education
Spinal tumors can develop in the bones, nerves, spinal cord, and other tissues of the spinal column. But due to the rarity of their occurrence, they have not yet been thoroughly studied, so it is still difficult to establish exactly what exactly was the reason for their formation. Modern medicine is inclined to believe that the main reasons for the formation of tumors in the spine may be:
- genetic predisposition;
- poor nutrition with a predominance of harmful foods rich in carcinogens and a deficiency of fruits and vegetables, which are sources of antioxidants;
- smoking and alcohol abuse;
- regular contact with toxic substances;
- influence of radioactive radiation;
- the presence of severe autoimmune diseases or immunodeficiency;
- the presence of chronic diseases of the spine, as well as frequent injury;
- prolonged, severe or frequent stress;
- abuse of visiting solariums and sunbathing.
Be that as it may, the formation of a tumor is caused by changes in the genetic apparatus of cells, which causes “errors” in their growth and differentiation. As a result, cells divide too actively and change morphologically.
Cancer is a consequence of the shutdown of the natural cell death mechanism, which can be the result of various external factors, including the activity of free radicals (oxidative stress), etc. Cells must divide, which is the basis of life. But this cannot go on forever. Normally, the ends of its chromosomes, called telomeres, are gradually shortened. As soon as they are shortened to a certain length, the apoptosis mechanism is triggered, which leads to natural cell death. When the genetic information of a cell is damaged by one factor or another, this mechanism is turned off. As a result, the cell is able to divide endlessly, which leads to the formation of a whole cluster of cells, i.e., a tumor, at its location. In addition, cancerous or malignant cells are able to imitate extracellular growth signals, which leads to a constant increase in tumor size at different rates, depending on the nature of the cells.
After a malignant neoplasm reaches a certain size (an average of 2-4 mm), it begins to need its own blood vessels, which will provide its nutrition. This is what happens in practice, although the nature of the growth and formation of new vessels inside the tumor is not yet fully understood. But it has been absolutely established that cancer cells have the ability to separate from the mother tumor and enter the blood and lymph through the extracellular matrix. With them, they can enter absolutely any organ and tissue of the human body, including the spine, giving rise to a new tumor. Such secondary neoplasms are called metastases.
Symptoms of a spinal cord tumor in adults
There are no typical or characteristic symptoms only for a tumor; all signs can mimic other diseases, especially in the early stages.
Therefore, you should consult a doctor to determine or rule out the problem with the following complaints. Pain syndrome. The most common manifestation of a tumor is pain that occurs in the area of the spine where the tumor began to grow. In the early stage, the pain may be mild or more severe, but there are no significant neurological symptoms. As the tumor progresses, disturbances in sensitivity and movement occur, the pain becomes stronger against the background of coughing or sudden movements, sneezing, physical activity, at night and when moving, tilting the head.
Movement disorders. Muscle weakness is also possible, which occurs in combination with sensitivity disorders, the phenomenon of muscle atrophy, sharp and sudden contractions, twitching of muscle groups that are relaxed.
Sensitivity disorders. Sometimes there is no pain, but superficial sensitivity may suffer, while maintaining a deep tactile sense. The patient may not feel pain, temperature, or touch, but perceives pressure and vibration.
Problems with the functioning of the sphincters. Possible disturbances in urinary functions and, less commonly, bowel movements. This leads to retention of urine or stool.
Also, as the process progresses, scoliosis of the spine may occur, which is formed due to pain, motor dysfunction or destruction of the vertebral bodies.
It is impossible to identify spinal cord tumors externally; they are located quite deep in the spinal canal.
Primary malignant tumors of the spine
Osteogenic sarcoma
The only malignant tumor arising from its own bone tissue.
Osteogenic sarcoma is one of the most malignant and common skeletal tumors with a favorite localization in the metaphyses of long tubular bones, accounting, according to many authors, from 30% to 50% of all bone tumors. In the spine, osteogenic sarcoma is much less common and accounts for 1.7% to 2% of all primary spinal tumors. The tumor is predominantly localized in the lumbar spine. Males are more often affected. This tumor can occur at any age. The clinical picture of osteogenic sarcoma has features characteristic of malignant tumors. The history of the disease is short, from 1-2 months to 1 year. Patients are bothered by intense pain in the affected area, which becomes permanent. There is a restriction in the mobility of the spine, patients take a forced position. Neurological complications appear very quickly in the form of paresis, paralysis, pelvic dysfunction, and a general serious condition.
Combined treatment: after maximum surgical removal of the tumor, radiation and/or chemotherapy are used.
Chondrosarcoma
A malignant cartilaginous tumor that accounts for 7% of all primary spinal tumors and 5% of all skeletal chondrosarcomas.
The tumor is more common in men between 20 and 60 years of age. Chondrosarcoma can affect both the arch with its processes and the vertebral body, with transition to adjacent vertebrae or ribs in the thoracic region. The neoplasm is most often found in the lumbar and sacral regions. Chondrosarcomas are divided into primary, which are much more common, and secondary, which develop as a result of malignancy of osteochondral exostoses. The clinical picture consists of 2 leading symptoms: pain and swelling. Chondrosarcomas are prone to frequent recurrence and are resistant to radiation therapy. You can count on a favorable prognosis only if the tumor is radically surgically removed.
Ewing's sarcoma
A malignant tumor that occurs mainly in childhood and adolescence and very rarely in adults. The tumor is usually localized in long bones; in the spine, Ewing's sarcoma occurs in 6.4% of all spinal tumors. The predominant localization of the tumor is the lumbar and sacral spine. The first symptom of the disease is usually pain, accompanied by a rise in temperature to 38-39C. Subsequently, against the background of increased pain, limited mobility of the spine occurs, and neurological complications due to compression of the spinal cord and roots are added. Given the vagueness of the x-ray picture, the diagnosis is usually clarified by a puncture biopsy. If compression of the spinal cord occurs, urgent surgical intervention is necessary. Given the high sensitivity of the tumor to radiation and chemotherapy, treatment should be combined.
Chordoma
Accounts for 1.3% to 4.1% of malignant tumors.
The tumor is most often localized in the sacrum, less often in the base of the skull and other parts of the spine. Chordoma most often affects men, 3/4 of cases occur between the ages of 45 and 70 years with a disease duration of up to 10 years. The clinical course of chordoma is determined by its localization, direction of growth and relationship with surrounding tissues. The clinical picture of sacrococcygeal chordoma in the initial stages of the disease is similar to discogenic radiculitis, which leads to diagnostic errors and unreasonable treatment. The main complaint is pain in the sacrum, sometimes radiating to the perineum or legs. Sacral root syndrome often develops: nagging pain radiating to the perineum, legs, genitals; sensitivity disorders in the anogenital zone and dysfunction of the pelvic organs. The leading diagnostic method is CT examination. Chordoma is a long-growing, aggressive tumor characterized by infiltrative growth, a tendency to relapse, malignancy and late metastasis. Treatment is surgical.
Primary malignant bone lymphoma (reticulosarcoma, non-Hodgkin's sarcoma)
Frequent malignant lesions of the spine, which account for up to 4-8% of all malignant tumors, arise from the reticular stroma of the bone marrow or its derivatives.
Lymphoma can occur in any age group. Women get sick more often. The leading clinical symptom, as with most bone tumors, is aching pain, which is periodic for a long time (from 1.5 to 4 years). A number of patients experience limited spinal mobility and reflex scoliosis. The general condition remains satisfactory for a long time and only in the later stages is weight loss and anemia noted. By destroying a vertebra, lymphoma often causes a pathological fracture, which dramatically changes the clinical picture and causes the addition of neurological symptoms.
Lymphoma is highly sensitive to radiation therapy. Some authors indicate that it regresses without surgical intervention. However, if compression syndrome occurs, the first step is surgical treatment.
Lymphogranulomatosis (Hodgkin's disease)
It is a systemic disease of reticuloendothelial tissue, which predominantly affects the lymph nodes with frequent involvement of the skeletal bones (the frequency of localization of lymphogranulomatosis in the bones is 15-35%).
There are both multiple (more often) and single lesions. The localization of the tumor in the spine is the most common among all bone lesions with predominant localization in the thoracic and lumbar regions. Clinical manifestations of lymphogranulomatosis of the spine are diverse and depend on the localization and extent of the process. The earliest clinical symptom is pain, which quickly becomes constant and increases in intensity. The most characteristic radiological sign is the osteolytic type of destruction, with preservation of the intervertebral discs. Pathological fractures of one or more vertebrae often occur. Often, the process spreads paravertebrally and to the ribs.
Generalized cases are treated with chemotherapy. If pathological fractures and neurological complications occur, surgical intervention is required.
Plasmacytoma and myeloma (Rustitsky-Kahler disease)
Refers to malignant tumors consisting of immunocompetent (plasma) cells and is characterized by multiple diffuse lesions of the bone marrow. Currently, plasmacytoma (solitary myeloma) and multiple myeloma are considered not as separate nosological forms, but as variants of the manifestation of the same tumor process. The criterion for classifying a tumor as solitary is the mandatory histological confirmation of the presence of a single focus of destruction, identified using X-ray, radioisotope and other research methods. Plasmacytoma is usually observed in adulthood, although it also occurs at an earlier age. Mostly men get sick. Most often the tumor is localized in the thoracic region, which determines the initial symptoms in the form of periodic pain between the shoulder blades of moderate intensity. As the process progresses, the pain becomes constant, debilitating, and sharply intensifies with movement. Sometimes there is an asymptomatic course of the disease and the tumor is detected only when a pathological fracture occurs with the development of neurological complications. During X-ray examination, the vertebral body is almost always affected; sometimes the arch, processes, and adjacent discs are involved in the process. In half of the cases, solitary plasmacytoma is polycystic in nature. In advanced stages, the height of the vertebrae decreases sharply with the formation of the so-called. "fish vertebrae" Most patients develop multiple myeloma after a latency period of 5-10 years.
Metastatic lesion of the spine
Metastatic lesions can affect various structures of the spinal column.
Up to 50% of patients who have compression lesions of the vertebrae as a result of metastatic lesions do not have a verified primary tumor site. The most common sources of metastases are tumors of the breast, prostate, lungs and kidneys - they cause up to 80% of metastases of the entire skeletal system. The duration of the disease ranges from 2 months to 3 years. The clinical picture of metastatic lesions of the spine does not have specific symptoms and is characterized by a short history, intense pain, impaired spinal mobility and neurological complications resulting from compression by a pathological fracture.
Radionuclide scintigraphy helps to identify common lesions of skeletal bones in metastatic disease, however, due to the lack of specificity, it does not exclude myeloma and other diseases with polyostotic lesions. MRI plays a leading role in the diagnosis of metastases, as it allows one to accurately localize the lesion in large parts of the spine, determine its nature and relationship with the structures of the spinal cord.
Classification of spinal cord tumors in adults
There are many options for classifying tumors localized in the spinal cord.
It is possible to divide into groups according to a number of characteristics - the location of the tumor focus relative to the spinal cord, spine or meninges, features of the histological picture, as well as the specific location of the lesion. If we divide tumors by origin, they can be classified into two groups:
- primary is tumor tissue that developed from the cells of the spinal cord itself, its roots or membranes;
- secondary are tumors of a different localization that affect the spinal cord (including metastatic ones).
Based on the location of the tumor, they can be divided into several groups:
- extradural tumor - a lesion above the area of the dura mater;
- intradural – tumor under the dura mater;
- intramedullary - grows inside the spinal cord, originating from its cells.
Tumors can be located behind the spinal cord, in front, on the sides, affecting the cervical or thoracic, lumbar or sacral regions.
There is a very wide classification based on the origin and type of cells; tumors are determined based on biopsy data.
Extramedullary type
Such neoplasms, which in medicine are given the name “extramedullary,” are concentrated not inside the spinal component, but in close proximity to it. Simply put, they originate in the structures that surround the SC (developing from the meninges, nerve roots, fatty tissue and other tissues passing nearby).
This category of harmful process is the most common; it develops 4 times more often than true intracerebral pathogenesis, and, fortunately, is more represented by pathologies of benign origin. But this does not mean at all that a non-malignant disease cannot portend anything terrible. In the absence of the necessary treatment, it threatens severe disability due to compression of the spinal cord and its elements, up to the complete loss of the ability to move and self-care. Sudden death cannot be ruled out. This is not to mention the fact that due to such neoplasia, irreversible destruction of the bone and cartilaginous units of the spinal column often occurs. Therefore, both extra- and intramedullary tumors equally require timely diagnosis, as well as the rapid involvement of adequate methods of therapy.
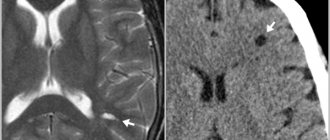
MRI.
Extramedullary OSM can have extradural (31.5%) or intradural (68.5%) localization. The extramedullary-extradural type is distinguished by its large size and the predominance of malignant forms; in turn, the malignant focus progresses at a fairly intensive pace and is predominantly recognized as a secondary (metastatic) formation. The extramedullary-intradural type of pathology, which is also the most common, is characterized by a predominance of primary neuromas (40%) and meningiomas (25%).
- Meningioma (arachnoidendothelioma) is a benign tumor that grows slowly and gradually. Formed from cells of the arachnoid meninges. Diagnosed over the age of 50 years, and in predominant numbers in women (80%). With a high frequency it affects the spinal membrane in the thoracic region. Rarely, but can recur and produce multiple growths, causing transverse damage to the spinal column. Although the size of this neoplasia, which externally resembles a small dense node, rarely increases by more than 1.5 cm, such a tumor even a few millimeters in size can directly put pressure on the nerve structures, provoking a severe neurological clinical picture of symptoms.
- Neuroma (schwannoma) is a round-shaped benign OSM with clear boundaries and a dense structure, which develops as a result of metaplasia of lemmocytes (Schwann cells), namely auxiliary cells of the peripheral nerve fiber involved in the formation of the myelin sheath. Female patients are more likely to experience this disease; people of middle age and older have the greatest predisposition. At first, the disease proceeds latently, and later it is expressed by severe radicular pain, paresis and paralysis of the muscles in the area of innervation, loss of sensitivity according to the conduction type. The neck and thoracic region are common areas that neuromas affect.
Other extramedullary neoplasms with intradural concentration (angiomas, lipomas, metastases, etc.) are much less common.
Diagnostics
Diagnostics is a step-by-step process that allows you to determine the size and type of tumor and create a plan for its treatment.
First of all, the doctor is interested in the patient’s complaints, symptoms, and medical history. What is important is when the symptoms developed and how they changed over time. A full neurological examination is also carried out - determination of muscle tone, reflexes, muscle strength, spinal mobility, sensitivity.
To refine the pathology you need:
- MRI with contrast - this method helps to determine the condition of the entire spinal cord, its structures and determine the tumor;
- CT myelography is a technique for assessing the tumor border;
- diffusion-weighted and diffusion tensor MRI;
- scintigraphy.
- direct angiography.
After clarifying the type, location and size of the tumor, a treatment plan is drawn up.
Modern methods of treatment
“The main type of treatment,” says oncologist Alexander Seryakov, “is a neurosurgical operation in which the tumor is completely removed and decompression (removal of compression) of the spinal cord is performed.
Micro-neurosurgical techniques, intraoperative neuroimaging and neuronavigation are often used. For malignant tumors of the spinal cord, in addition to surgical treatment, the patient may be prescribed chemotherapy and radiation therapy (stereotactic radiotherapy and radiosurgery using linear accelerators of the CyberKnife type).
Rehabilitation
After treatment, each patient requires long-term rehabilitation in the following 3 areas:
- Restoration of internal organs – cancer treatment methods have an extremely negative effect on the patient’s body as a whole. This includes disruption of the functioning of many organs, the appearance of chronic weakness, lack of appetite, etc.
- Psychological recovery - a person who has overcome long-term treatment for cancer is in great need of restoring his psycho-emotional state.
- Physical recovery (exercise, physical therapy, etc.). Physical activity helps to launch all processes and systems, which has a beneficial effect on the patient’s recovery.