Risk factors for stroke and heart attack
Planning a preventative treatment regimen is based on addressing risk factors that are largely similar for heart attack and stroke.
Metabolic risk factors include:
- dyslipidemia (impaired lipid metabolism - organic compounds, including fats and fat-like substances);
- arterial hypertension;
- obesity;
- metabolic syndrome;
- diabetes mellitus and other endocrinopathies;
- coagulopathies (diseases that develop as a result of disorders of the blood coagulation and anticoagulation systems).
Common markers of heart attack and stroke are:
- previous cardiovascular diseases;
- peripheral vascular pathology;
- calcium index;
- stress test results;
- hypertrophy (thickening of the wall) of the left ventricle.
Atherosclerotic stenosis of the carotid arteries and brain tumors increase the risk of stroke. The provoking factors of a heart attack are:
- atrial fibrillation;
- dysplasia (developmental disorder) of connective tissue;
- arteritis;
- diabetes.
Although the incidence of stroke is higher in men, it is more severe in women, and about half of deaths from stroke occur in women.
Make an appointment
Signs of a stroke
To diagnose cerebral blood supply disorders, it is necessary to use stroke recognition techniques:
- When trying to smile, you need to pay attention to the corners of the mouth - in case of a stroke, it can be directed downwards, the smile looks crooked and asymmetrical;
- When trying to speak, it may be difficult to pronounce even the simplest words and sentences;
- When trying to raise both arms, asymmetry is observed;
- The protruding tongue falls to the side.
If at least one of the symptoms is positive, you must immediately call an ambulance. Under no circumstances should you give him water, feed him, lift him, or take him by handy transport to the nearest hospital, as this can cause harm.
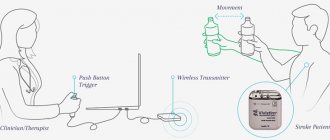
A set of active movements for the hands
You can make independent movements with your hands up to 20 times in one approach:
- clench and unclench your fingers into a fist;
- circles in both directions in the wrist joint (it is recommended to keep your fist clenched);
- flexion and extension at the elbows;
- from a position along the body, slowly rise and fall, while loading the shoulder joints;
- swing to the sides.
Exercises with dumbbells use flexor muscles and hold by clenching the hand into a fist.
Help in the acute period
Which doctors are needed in the treatment of stroke depends on the period of the disease, but in any case, they must be experienced, highly qualified specialists who know how to properly provide assistance in this situation.
When diagnosing an ischemic stroke in a patient, the doctor’s goal is to restore blood supply with subsequent rehabilitation. This may require blood thinning medications or mechanical removal of the clot using a catheter. To remove atherosclerotic plaques, endarterectomy is performed, and to increase the diameter of blood vessels, plastic surgery with stenting is performed.
For the shoulder joint
Restoration of the forearm and shoulder joint takes place with the help of flexion and extension exercises, rotation, push-ups, muscle tension and relaxation, clapping, and massage. To do this, use exercise machines, dumbbells, and various devices. First, the arm is kneaded, then a set of exercises is performed; therapeutic exercises are always combined with a massage of the limbs. A set of exercises for the shoulder joint:
- The patient lies on his back, arms extended along the body. The instructor holds his hand at the elbow to avoid bending, takes the patient's palm with his other hand and moves the patient's arm up and down.
- The instructor performs circular movements with the patient's arm fixed in a straightened state.
- The patient lies on his back, with his arm slightly to the side. The instructor turns the straightened arm over, palm down, then up.
How long to stay in hospital if you have a stroke
Poor blood circulation in the brain, in other words, stroke, treatment involves three stages:
- prehospital;
- stay in the intensive care unit;
- treatment in a general ward.
The length of stay of a patient in a hospital, according to treatment standards, is 21 days, provided the patient has no violations of vital functions, and 30 days in case of serious violations. When the length of a patient’s stay in a hospital is insufficient, a medical examination is carried out followed by the development of an individual course of rehabilitation.
All patients diagnosed with stroke are subject to hospitalization. The length of stay in intensive care depends on a number of factors, including:
- depression of vital functions;
- degree of damage to brain tissue. With a major stroke, patients stay in intensive care longer;
- the need for constant monitoring if there is a high risk of recurrent stroke;
- severity of the clinical picture;
- level of depression of consciousness and others.
Basic and differentiated therapy
Treatment of a patient in the intensive care unit involves basic and differentiated therapy.
Basic treatment is aimed at:
- fight against cerebral edema;
- restoration of normal functioning of the respiratory system;
- patient nutrition;
- maintaining hemodynamics at an acceptable level.
Differentiated therapy involves:
- normalization of arterial and intracranial pressure, elimination of cerebral edema after hemorrhagic stroke. In the first two days, a decision is made regarding the need for surgery. Neurosurgeons at the Yusupov Hospital daily perform surgical interventions to eliminate the consequences of stroke and save the lives of hundreds of patients. All manipulations are carried out using modern medical equipment using effective proven techniques;
- accelerating metabolic processes, improving blood circulation and increasing the resistance of brain tissue to hypoxia when diagnosed with ischemic stroke. The length of stay in intensive care directly depends on the timely and adequate course of treatment.
In most cases, young people recover much faster than older patients.
It is possible to transfer a victim from the intensive care unit to a general ward after meeting a number of criteria:
- the patient can breathe independently, without the support of devices;
- the patient is able to call a nurse or doctor for help;
- there is a stable level of heart rate and blood pressure;
- the possibility of bleeding is excluded.
Only after the patient's condition has stabilized can the doctor transfer the patient to the ward. In a hospital setting, various rehabilitation procedures are prescribed to quickly restore lost functions.
In the neurology department of the Yusupov Hospital, patients are not only developed an individual course of rehabilitation therapy, but also given psychological support.
If necessary, psychologists work with loved ones and relatives of the patient to teach them the basics of caring for a person who has suffered a stroke.
A set of active exercises for legs
For the legs, exercises can also be started with a period of strict bed rest and continued while sitting. The number of repetitions should not tire the patient and increase gradually to 20.
- The toes actively perform flexion and extension.
- Pull your socks towards you, then move them to the opposite extreme position (it is recommended to mentally imagine the pressure on the pedals).
- Slow knee flexion, extension.
- Abduction to the side due to the work of the hip joint.
Recovery period
The rehabilitation period is aimed at restoring lost functions and improving the quality of life of patients who have suffered a stroke. The doctor develops a rehabilitation program individually for each patient, taking into account the scale of the vascular accident, age, comorbid pathology, etc.
In case of strokes, doctors assign a special role to the prevention of recurrent strokes, which includes proper nutrition, giving up bad habits, eliminating excess weight, and regular monitoring by a doctor.
Is full recovery possible after a stroke?
The patient’s relatives play a significant role in the rehabilitation of a patient after a stroke. It depends on their attention, care, patience and correct actions whether the patient’s lost functions can return.
The recovery process after a stroke is a difficult period, both for the patient himself and for his loved ones. The rehabilitation time depends, first of all, on the degree of damage to brain tissue. Patients may have impaired coordination of movements, mobility of limbs, speech, memory, hearing, and vision.
The patient’s persistence and positive attitude can speed up the recovery time of lost functions.
An experienced team of doctors will speed up the rehabilitation process thanks to a well-designed individual treatment program.
Levels of recovery after stroke
After hemorrhagic and ischemic strokes, there are three levels of recovery:
- the first is the highest. We are talking about the complete restoration of lost functions to their original state. This option is possible in the absence of complete death of nerve cells in a region of the brain;
- the second level is compensation. The early stage of recovery, usually in the first six months after a stroke. Lost functions are compensated by the involvement of new structures and functional restructuring.
- The third level involves readaptation, that is, adaptation to the emerging defect. The patient’s relatives and friends play a significant role in this process. They are the ones who help the patient learn to live with the emerging defect.
Specialists at the Yusupov Hospital, if necessary, work with the patient’s relatives, teaching them the specifics of care, as well as providing them with psychological support.
Active gymnastics
Passive movements and massage are preparatory measures before active gymnastics, which plays an important role in developing isolated movements in paretic limbs.
Active gymnastics begins with exercises for healthy limbs, alternating them with gymnastics for paretic ones, as well as breathing exercises. The load on the cardiovascular and respiratory systems should increase gradually, otherwise the patient may become overfatigued. It is recommended to monitor the pulse after each exercise performed 1-5 times. Exercises should be separated by rest breaks lasting 1-2 minutes.
Active gymnastics begins with exercises in isometric mode. Isometric muscle contraction is a contraction without shortening, that is, without movement in the joints. When performing exercises in this mode, it is often necessary to provide assistance to the patient.
To achieve isometric contraction of the extensors of the hand and fingers, the patient is placed on his back, the arm is bent at the elbow and the forearm is placed in a vertical position. Then you should extend (straighten) the hand and fingers (so that they are 180 degrees with the forearm). Holding the paretic arm by the forearm, the patient is asked to keep the hand and fingers in this extended position. In the same starting position, but holding the paretic arm by the hand, the patient is asked to hold the forearm in a given vertical position.
This exercise is aimed at training the forearm flexors in an isometric manner. To train the forearm extensors, the patient’s paretic arm is extended at the elbow and raised vertically upward. When fixing the patient's shoulder, they are asked to hold the arm in a raised position. To do this, he must tense the extensors of the forearm.
Isometric contraction of the abductor muscles of the shoulder is carried out with the patient positioned on the healthy side. The paretic arm is raised up and bent at the elbow at an angle of 90 degrees. While supporting the forearm, ask the patient to hold his hand in this position.
The hip flexors are trained isometrically with the patient in the supine position. The paretic leg is bent at the knee, lightly holding it by the shin. And the patient is asked to hold the leg in this position, not allowing it to straighten at the knee. In the same starting position, you can train the hip abductors. Slightly moving the leg bent at the knee to the side, ask the patient to hold it in a fixed position.
These exercises make up the initial complex of active gymnastics. In the first days of classes, they should be performed 2-3 times, gradually increasing the number of exercises to 5-10 times.
When patients begin to develop independent isolated movements, they begin to train them. For this purpose, light exercises are used, the purpose of which is to eliminate the unwanted influence of gravity. “It is best to carry them out using various suspensions, hammocks and blocks.
Lightweight exercises should not cause pain. They are performed at a slow pace, in a volume accessible to the patient. First of all, exercises are carried out for muscles whose tone usually does not increase. So, for example, supporting a paretic arm with a hammock, the patient is asked to perform those active movements that he has already developed.
This includes abduction and adduction of the shoulder, flexion and extension of the forearm, and extension of the hand. Facilitated abduction and adduction of the hip is trained with the patient in the supine position. And by turning the patient onto the healthy side and supporting the affected leg, they train the extension and flexion of the lower leg.
As the range of active movements increases over time, you should add exercises with light, measured resistance. It works like this; for example, when actively extending the lower leg, you should try to slightly impede this movement by pressing on top of the lower leg and not allowing the leg to extend at the knee. Exercises with light resistance are carried out similarly for the remaining muscle groups.
It must be remembered that resistance exercises are included in the complex of active gymnastics only when active isolated movements appear in a sufficiently large volume.
These exercises are recommended mainly for muscles in which the tone does not increase. The person performing them needs to pay special attention to breathing. The patient should not delay him. Resistance exercises should be combined with passive relaxation exercises.
Prognosis for recovery after stroke
Favorable factors for recovery after a stroke include:
- timely early start of rehabilitation therapy;
- spontaneous early recovery of lost functions.
Among the unfavorable factors of recovery after a stroke are:
- advanced age of the patient;
- large area of brain tissue damage;
- poor blood circulation around the affected brain tissue;
- damage to cells in functionally important areas of the brain.
Basics of Stroke Recovery
In the process of rehabilitation, the positive attitude of the patient himself and his desire to return to independent life are important. Psychological support and assistance from the patient’s relatives plays a huge role. You can make an appointment with a neurologist by phone.
Memory recovery after stroke
Treatment of patients after a stroke takes place in the neurological department. Memory restoration depends on many factors: the size of the area of brain damage, the location of the damage, and the timeliness of medical care. The faster blood circulation in the brain is restored, the greater the chance of memory recovery after a stroke.
Memory restoration after a stroke is possible with the participation of several specialists - a neurophysiologist, psychologist, neuropsychologist, neuropsychiatrist. Help for a patient after a stroke is provided at the rehabilitation clinic of the Yusupov Hospital. In the hospital, the patient is treated according to an individual recovery program; many specialists take part in the development of such a program. When developing the program, the patient’s health condition, the severity of brain damage, and memory impairment are taken into account.
In some cases, it takes several years to restore memory and speech; during recovery, the doctor prescribes medication, a special diet, various trainings - color therapy, rhythm therapy, music therapy and others. Memory restoration at home is not always successful due to the lack of a training program and knowledge in the field of rehabilitation of patients after a stroke.
You can make an appointment with a neurologist at the Yusupov Hospital by phone. Consultation with a specialist, full patient care, rehabilitation using innovative equipment, massages and exercises will help the patient regain full memory.
Restoring a hand after a stroke
A positive attitude and support from family have an impact on rapid recovery from illness. Partial paralysis of the arm is a common occurrence after a stroke and is characterized by stiffness of movement and limited motor ability of the arm. Functional paresis (partial paralysis) refers to neurological syndromes, caused by disruption of the nervous system, damage to the nervous system pathway due to damage to the cerebral cortex after a stroke. Paralysis of the arm is the complete absence of voluntary movements of the limb.
Recovery from a stroke may involve the hand or the entire limb. With partial paralysis, the ability to move the arm or hand freely is impaired; the person cannot fully care for himself or perform basic actions. To restore motor ability, the patient must perform daily exercises for finger motor skills and limb motor skills.
The rehabilitation process of restoring motor activity of the limbs requires patience from the patient and a lot of work - this will allow you to return to a full life after a stroke. You can make an appointment with a neurologist by phone. The rehabilitation doctor will develop individual exercises for the patient, the patient will be under constant medical supervision and receive qualified assistance from specialists.
Exercises in a sitting position
If the patient already has the physical ability to sit independently, you can proceed to the next stage - gymnastics in a sitting position. It is aimed at improving the functioning of the limbs, strengthening the back muscles and preparing for walking. Let's look at recovery exercises:
- Sit on the bed, lower your feet to the floor. Hold onto the bed with your hands. Bend your back, pushing your chest forward. In this case, the deflection should be while inhaling, you need to relax while exhaling;
- In a sitting position, place your legs on the bed. Lift each limb up in turn. The legs should be straight;
- Lean your back on the pillow, stretch your legs forward, arms up. Bend your leg at the knee, clasp it with your hands. In this case, you must try to touch the knee joint with your chest. Hold for a couple of seconds, tilt your head forward, and exhale. Then raise your head and slowly return to the starting position. Do the same manipulation with the second leg;
- Lean back on the pillow, taking a comfortable position. Grasp the edges of the bed with your hands. Throw your head back, trying to bring your shoulder blades together. Remain in this position for a few seconds, return to the starting position;
- Sit on the bed with your legs dangling. Turn your head in different directions, then make circular movements. Manipulations should be slow;
- It is also useful to simply sit on the bed with your legs down. But the main condition is to not hold on. This exercise helps restore coordination and prepare for walking.
Important! At this stage, fine motor skills should be developed by sorting small objects.
We invite you to watch a video on how to exercise in a sitting position:
Factors influencing the speed and quality of rehabilitation
There are many factors that influence the speed of recovery after a stroke, so predicting the duration of rehabilitation and likely results is quite difficult.
How long rehabilitation after a stroke will last depends on the individual parameters for each person, as well as on other factors:
- volume of damage: an extensive stroke significantly worsens the severity of the patient’s condition, and also causes many neurological complications that adversely affect the timing of recovery and its quality;
- patient’s age: the older the victim, the longer the recovery;
- localization of damage: circulatory disorders of deep structures are difficult to treat;
- type of stroke: hemorrhagic strokes are less common, but occur in a more aggressive form, and also have a high mortality rate, although the prognosis for rehabilitation is more favorable than for ischemic stroke;
- caused by disorders: the presence of multiple cerebral symptoms, comatose states, severe paralysis and sensory disturbances give an unfavorable prognosis for recovery;
- timeliness of therapy: the most positive results of therapy can be achieved by starting treatment measures in the first 4 hours after the onset of the first symptoms; seeking help at a later time worsens the prognosis;
- compliance with medical recommendations: after the patient is discharged from the medical institution, the patient is given recommendations that can improve the quality of life, prevent the formation of relapse and negative complications.
The severity of the lesion has the greatest impact on the likelihood of restoration of lost functions and the timing of rehabilitation. With extensive strokes, violations of the most important functions are observed, even if the prescribed rehabilitation program is followed, the prognosis is rather disappointing. The greatest difficulties arise with the complete return of speech and motor functions. Close relatives who will devote a lot of time to special activities with the patient can positively influence the situation.
Treatment by positioning on the back and on the healthy side
The paretic limbs are positioned with the patient in a supine position so that the muscles in which tone usually increases after a stroke (shoulder adductors, arm flexors, hip adductors, leg extensors and dorsal flexors of the foot) are stretched. To do this, place a chair with a pillow at the patient’s bedside, on the side of the paralyzed limbs, on which the sore hand is placed, palm up.
The arm is straightened at the elbow and moved to the side at an angle of 90 degrees. A cotton swab covered with oilcloth is placed under the patient's armpit. The fingers are extended. The hand and forearm are bandaged to a splint, which can be cut out of some hard material (for example, plywood) and covered with gauze.
To fix the position of the hand, place a bag of sand or salt (weighing 0.5 kg) on it. The paralyzed leg is bent 15-20 degrees at the knee, under which a bolster is placed. The foot rests against a wooden box (“boot”) covered with soft material. It is recommended to put a small pillow in the boot to better support the foot.
The patient can remain in the supine position for 1.5 to 2 hours. Then it should be turned onto its healthy side.
When laying the patient on his healthy side, as opposed to laying him on his back, the paralyzed limbs are given a flexion position. The sore arm is bent at the shoulder and elbow joints and a pillow is placed under it, and the paralyzed leg is bent at the knee and hip joints and also placed on a pillow. Just as in the supine position, it is very important to ensure the correct position of the hand and foot. The fingers of the hand should be straightened, the hand should be tied to the splint and lie on the pillow, palm down. The foot should rest against the box. The patient can remain in a lying position on the healthy side for 30 to 50 minutes.
During the first days after the disease, they regularly alternate between placing the paretic limbs in the position of the patient on the back and the healthy side. Treatment by position is not performed during meals, sleep at night, or other therapeutic measures.
Styling paretic limbs prevents the development of muscle contractures, helps reduce muscle tone and prevents the development of pain in the joints (especially in the shoulder). In addition, changing the patient's position in bed every 1-2 hours prevents the development of bedsores.
Stroke Prevention
Prevention of heart attack and stroke in women and men are links in one chain of measures that prevent disability and death in people suffering from cardiovascular diseases.
Cardiologists and neurologists at the Yusupov Hospital use modern diagnostic methods to examine patients, allowing them to identify risk factors for vascular diseases and take measures aimed at preventing diseases. Medicines for the prevention of stroke and heart attack allow you to control the course of the disease, reduce the incidence of acute cardiovascular crises, and the likelihood of complications.
Chance of full recovery after stroke
The rehabilitation period is individual; for some, a few months are enough; for others, it will take years to achieve a positive result. The earlier restoration procedures are started, the more favorable the prognosis. At the same time, the patient’s attitude and focus on results is important; The greater a person’s desire to return to a full life, the more effective the classes and exercises.
At the Yusupov Hospital, a well-coordinated team of professionals (neurologists, rehabilitation specialists, therapists, cardiologists, speech therapists, psychologists) takes part in the rehabilitation of patients after a stroke. Doctors create an individual program for each patient, aimed at the best possible result, observing the following principles:
- early start of restorative procedures;
- systematicity and duration of events;
- complexity of procedures;
- multidisciplinarity of classes;
- compliance of procedures with the patient’s condition;
- active interaction between doctors and the patient and his family.
You can make an appointment with the doctors at the Yusupov Hospital and find out how much rehabilitation after a stroke costs by calling.
Passive movements and massage
Simultaneously with positional treatment, they begin to engage in passive gymnastics (movements in the joints of paretic limbs, which are carried out by a physical therapy methodologist or a person replacing him). Passive movements are carried out without active muscular assistance from the patient. They are performed carefully, at a slow pace.
Passive movements are carried out as fully as possible, isolated in each joint. To do this, the person working with the patient clasps the paretic limb above the joint being worked on with one hand, and with the other below this joint. And the development is carried out in the following sequence: shoulder, elbow, wrist joints and fingers, hip, knee, ankle joints and toes. The volume and tempo of movements gradually increase, their number for each joint can be from 5 to 10. Passive movements in the first days after a stroke are recommended to be carried out 2-3 times a day for all joints of the limbs.
When performing movements, the initial position of individual parts of the limbs is of great importance.
For example, during passive movements in the shoulder joint, the patient is placed on his healthy side, and the affected arm is bent at the elbow. With one hand they fix the shoulder joint of the sore arm, with the other they clasp the arm bent at the elbow joint and make circular movements, pressing towards the shoulder joint, as if screwing the head of the humerus into the glenoid cavity. Abduction of the hip is more complete when the leg is bent (at the hip and knee joints), since this reduces muscle tension in the adductor muscles of the thigh, and the resistance of these muscles decreases.
On these same days, you should begin to do a light massage of both healthy and paretic limbs. If you can use a variety of massage techniques when massaging healthy limbs, then when massaging paretic limbs you need to be very careful. The fact is that excessive massage can lead to a sharp increase in the tone of certain muscle groups, which is undesirable. Therefore, when massaging paralyzed limbs, it is recommended to use the following rules.
Massage on the arm should begin from the shoulder, and on the leg - from the buttocks and thigh (the patient's position is lying on his back or on his healthy side). Then they move on to massage other parts of the limbs.
When massaging muscles in which the tone is usually increased (pectoralis major muscle, biceps brachii, flexors of the hand and fingers, quadriceps femoris, triceps surae), only light stroking should be used. In this case, the pace of massage movements should be slow. When massaging their antagonists, in which the tone is usually also increased (extensors of the forearm, hand and fingers, posterior femoral group, tibialis anterior and peroneus longus muscles), you can still use other massage techniques: rubbing and shallow kneading. These muscles can be massaged comparatively more energetically and at a faster pace.