Stroke is an acute disease that is accompanied by the death of brain cells due to acute cerebrovascular accident. It manifests itself with general cerebral and local symptoms. The development of a stroke is possible in two scenarios: either after 24 hours from the onset of the disease, its symptoms persist, or death occurs.
Diagnostic examination for developing stroke includes:
- clarification of complaints and history of the disease;
- neurological examination;
- blood tests (determining the level of enzymes and blood glucose, the state of the coagulation and anticoagulation systems).
- Dopplerography - study of blood flow in the vessels of the neck and brain;
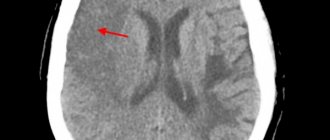
- computed tomography helps distinguish between ischemic and hemorrhagic strokes;
- Magnetic resonance imaging is more informative in cases of developing stroke;
- magnetic resonance angiography and computed tomography angiography are non-invasive methods for assessing the carotid and cerebral arteries;
- an electrocardiogram allows you to assess the condition of the heart muscle;
- Echocardiography (EchoCG) is a research method with which doctors at the Yusupov Hospital identify blood clots in the cavities of the heart, which allows them to assess the risk of developing a recurrent stroke.
Make an appointment
Types of brain strokes
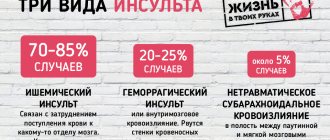
The most common ischemic stroke (infarction) of the brain - 85% of cases, hemorrhagic stroke occurs in 15% of cases. Strokes can be caused by several reasons:
- formation of thromboembolism in heart diseases;
- acute circulatory disorders in the cervical and large cerebral arteries;
- disturbance of blood circulation in the small arteries of the brain during the acute course of the process.
First aid for stroke
A quick reaction from relatives who can provide first aid to an old person after a stroke will help prevent serious consequences and provide the necessary treatment in the future.
So what needs to be done:
- position the patient so that the legs are 25–30 degrees below the head;
- try to determine blood pressure and pulse indicators, record them;
- if the patient has lost consciousness, do not try to move him to the bed, just lay him down correctly and leave him alone;
- After the ambulance doctors arrive, talk clearly and intelligently about the person’s previous condition, the medications he is taking, and the visible symptoms of the attack.
There are actions that doctors strictly prohibit taking. Under no circumstances should you:
- use ammonia when recovering from a fainting state;
- hold limbs during convulsions;
- try to offer the patient medications that may get stuck when swallowing (it is better to completely stop taking medications until specialists arrive).
We recommend
“Low blood pressure in an elderly person: treatment and prevention” Read more
Classification of strokes
Strokes are classified according to the causes of circulatory disorders and the duration of neurological symptoms. At the Yusupov Hospital, the patient will undergo a diagnostic examination, which will allow the type of stroke and the area of brain damage to be very quickly and accurately determined. When a patient is admitted to the clinic, a number of studies are carried out as prescribed by the doctor:
- MRI – magnetic resonance imaging;
- CT – computed tomography;
- Doppler ultrasound;
- cerebral angiography.
Classification of ischemic stroke (infarction) of the brain:
- hemorheological blockage of cerebral vessels. This condition develops with increased blood clotting and platelet aggregation;
- embolic stroke. Occurs in 20% of cases of ischemic stroke, develops when an artery is blocked by emboli (intravascular substrates) that enter small vessels from larger blood vessels;
- atherothrombotic stroke. Found in 50% of patients with ischemic stroke. A blood clot forms at the site of the atherosclerotic plaque, leading to blockage of the vessel;
- lacunar stroke. Arterial hypertension leads to the development of atherosclerosis, which causes narrowing of small arteries and reduced blood flow to areas of the brain. Occurs in 25% of cases;
- hemodynamic stroke. The pathological condition is caused by a sharp narrowing of a large vessel in the brain due to a drop in blood pressure during heart failure. Blood flow to a part of the brain stops, and an ischemic stroke develops.
Classification of hemorrhagic strokes:
- an outpouring of blood when a vessel ruptures in the brain tissue - parenchymal hemorrhage;
- formation of hematoma in the ventricles of the brain - intraventricular hemorrhage;
- hemorrhage into the cavity between the pia mater and the arachnoid membrane is called subarachnoid;
- Epidural, subdural and mixed forms of hemorrhages are quite rare.
Classification according to the duration of neurological symptoms:
- minor stroke – symptoms manifest from one day to three weeks. Recovery from one day to three weeks;
- transient ischemic attack - symptoms last for about a day, recovery within a day;
- Completed ischemic stroke – symptoms of the disease have been observed for more than three weeks, recovery does not occur for more than three weeks.
Detection of stroke: diagnosis
Detection of brain diseases is complicated by their location deep in the skull. However, it is possible to diagnose a disease such as a stroke in a timely manner!
80% of people who have had a stroke become disabled, a third of whom need help from strangers. Only 20% recover from the disease and can return to normal life!
The initial diagnostic stage includes a number of necessary studies:
- Blood tests: clinical and biochemical;
- Electrocardiogram;
- Computed tomography and MRI.
Periods of stroke
Among the huge number of neurological diseases, stroke is the most important problem. Hemorrhage in the brain leads to disruption of intracranial circulation, neuronal necrosis and disruption of vital body functions.
In ischemic stroke, a number of processes are observed that together lead to the death of neurons. Cell destruction occurs against the background of cerebral edema. At the same time, the brain increases in volume and intracranial pressure increases.
Due to cell swelling, displacement of the temporal lobe is observed, as well as infringement of the midbrain.
Compression of the medulla oblongata may also occur due to wedging of the cerebellar tonsils into the foramen magnum. This process quite often leads to death. Therefore, early hospitalization of the patient is extremely important.
When the first signs of an ischemic stroke appear, medical assistance should be provided within the first three hours, otherwise the prognosis is disappointing.
There are several periods of ischemic stroke:
- acute;
- spicy;
- early recovery period of stroke;
- late recovery;
- stage of residual effects.
The most acute period
In the first three hours, it is possible to restore blood flow and eliminate or reduce neuronal death through the use of thrombolytics. It is also possible to administer drugs into the stroke area itself, which helps prevent the development of complications.
Then doctors take measures to restore pressure, carry out rehydration, dehydration and oxygen therapy.
During the most acute period of a stroke (from 4 to 5 hours after the attack), the patient should be under the close supervision of a doctor in a hospital setting.
Acute period
The period up to 14 days after the attack is considered acute. The patient continues to undergo treatment in a specialized department of the hospital. He is undergoing drug therapy aimed at:
- reduction of cerebral edema;
- maintaining normal blood viscosity and coagulability;
- maintaining normal functioning of the cardiovascular system;
- relapse prevention;
- maintaining normal blood pressure.
Early recovery period
The early recovery period is considered to be the period from 2 to 6 months after a stroke. At this stage, complex treatment is carried out:
- the patient takes medications according to an individual treatment regimen;
- in case of speech impairment, a speech therapist works with the patient;
- various manipulations are prescribed to restore sensitivity of the limbs and other parts of the body (massages, baths, acupuncture and others);
- physical therapy – the method helps strengthen ligaments and muscles.
Late recovery period
The late recovery period is the time six months after the stroke. At this stage, the results of treatment and rehabilitation measures taken during the early recovery period are already visible.
The patient's finger sensitivity is restored and motor skills improve. It is extremely important not to stop the complex of procedures. Rehabilitation after a stroke is a long and labor-intensive process.
Period of residual effects
The time from one to two years after a stroke is considered the residual period. At this stage, it is important to follow all doctor’s instructions and take measures to prevent a recurrent stroke.
Rehabilitation specialists and neurologists at the Yusupov Hospital create a treatment and rehabilitation program individually for each patient, which allows achieving high results in recovery after a stroke.
Expert opinion
Author: Vladimir Vladimirovich Zakharov
Neurologist, Doctor of Medical Sciences, Professor, Head of the Center for Diagnostics and Treatment of Memory Disorders
According to statistics provided by WHO, stroke ranks third in prevalence among all neurological diseases. Doctors note an annual increase in incidence. In Russia, 400 thousand new cases of stroke are registered every year. More than 30% of them are fatal. Acute cerebrovascular accident is not a disease characteristic of older people. The disease can be diagnosed in 5-year-old children. A distinctive feature of old age is considered to be a greater number of factors predisposing to the development of stroke.
At the Yusupov Hospital, diagnosis of cerebrovascular accidents is carried out using modern medical equipment. CT and MRI make it possible to assess the size of the pathological lesion, its location, and the type of stroke. Treatment is developed individually for each patient. The drugs used meet quality and safety standards. If necessary, surgical intervention is performed. During the rehabilitation period, each patient is prescribed a course of physiotherapy and a complex of physical therapy. Experienced massage therapists work the muscles, helping to restore lost functions.
Ischemic stroke
Stroke can be ischemic or hemorrhagic. Ischemic stroke occurs on average five to six times more often than hemorrhagic stroke
- Etiopathogenesis of ischemic stroke
Most often, two types of ischemic stroke are observed: thrombotic, caused by primary thrombotic occlusion of cerebral vessels, and embolic, caused by embolism from a distant source. Primary thrombotic occlusion usually develops in a vessel whose lumen is narrowed as a result of atherosclerosis, for example in the carotid or basilar artery. The most common source of embolism is the heart. Cardiogenic embolism can occur with atrial fibrillation or myocardial infarction (due to mural thrombus formation), with prosthetic valves, infective endocarditis, and atrial myxoma. Less commonly, the source of emboli is ulcerated atherosclerotic plaques in the aortic arch and the mouth of the great vessels. Atherosclerosis of the carotid artery can be the cause of its primary thrombotic occlusion, but more often it is the source of embolism of the intracranial arteries. Rare causes of ischemic stroke include cerebral vein thrombosis, erythrocytosis, meningovascular syphilis, arteritis due to tuberculosis and collagenosis, dissecting aortic aneurysm.
- Classification of ischemic stroke
Strokes are classified according to their suspected pathophysiological mechanisms. First of all, clinical manifestations and their dynamics are assessed. Depending on how long the neurological defect persists, transient cerebral ischemia (PIM), also called transient ischemic attack (TIA) with complete recovery within 24 hours, minor stroke (full recovery time is more than 24 hours, but less than one week) are distinguished. ) and completed stroke (the defect persists for more than one week). Neurological disorders during embolism usually develop suddenly and immediately reach maximum severity; Stroke may be preceded by attacks of transient cerebral ischemia, but they are observed much less frequently than in the case of primary thrombotic occlusion. In thrombotic strokes, neurological symptoms usually increase gradually or stepwise in a series of acute episodes over several hours or days (progressive stroke). In the future, the diagnosis is based on the definition of:
- localization of the lesion;
- the nature of the vascular pathological process;
- information about preserved pathways of collateral blood flow in the ischemic zone.
If an accurate diagnosis can be called an inevitable factor in adequate therapy, then a necessary condition for the correctness of the latter is the study of the clinical picture of the disease, that is, the neurological condition of the patient directly at his bedside.
Thus, the diagnosis of a stroke symptom complex is based on the dynamics of the clinical picture and a characteristic set of subjective and objective symptoms.
- Ischemic Stroke Clinic
Strokes in 80% of cases are observed in the middle cerebral artery system, and in 20% in other cerebral vessels.
Ischemia in the middle cerebral artery basin. Available clinical experience shows that before the development of cerebral infarction, vessel narrowing is usually “prevented” by TIA in the middle cerebral artery basin. Their symptoms are similar to those of TIA, associated with deterioration of hemodynamics as a result of severe stenosis of the internal carotid artery, however, in contrast to the latter, the trunk of the middle cerebral artery and its branches are usually blocked by an embolus.
| In our country, as in other civilized countries of the world, stroke is the third leading cause of increased mortality after cardiovascular diseases and cancer. Stroke is a pathology that affects the working population, leading to prolonged hospitalization, persistent disability of patients, deterioration in the quality of life of their families and significant economic costs for the state. |
A few days before a stroke, the patient experiences headaches, weakness, blurred vision, dizziness, and transient numbness in the arm and leg. The phenomena increase, and one day in the morning the arm and leg stop working. The patient may not lose consciousness, but notices “fog” in the head. Or there may be a sudden, “stroke-like” development, which in the acute period is practically no different from a hemorrhagic stroke. With the development of right-sided hemiplegia, speech disorder in the form of more or less pronounced aphasia can be persistent. With lesions of the parietal cortex and internal capsule of the brain, the patient develops anosognosia, metemorphopsia, autoagnosia with delusional constructs. The patient has a body schema disorder with distorted perception at the border of the lost visual field, but he does not understand his condition.
Cases of the disease in which there is an extensive focus of softening as a result of switching off both the subcortical and cortical branches of the middle cerebral artery are very severe. Often such patients do not get out of bed, especially if they develop early flexion contracture in the paralyzed leg, which is poorly amenable to treatment. In relatively mild cases, after 1-2 months, movements in the limbs begin to recover, but recovery in the leg is better than in the arm.
With frequent occlusion of individual branches of the middle cerebral artery, incomplete syndromes arise: motor aphasia with contralateral paresis of the arm and facial muscles of the lower half of the face with occlusion of the upper branches, sensory aphasia with occlusion of the lower branches, and others. Mono- and hemiplegia leave an indelible mark on the patient’s motor skills; sometimes a hemiplegic gait (usually in the form of the famous Wernicke-Mann pose with a bent arm and straightened leg) can remain for life. In the paralyzed limb, vasomotor-trophic disorders are noted: coldness, cyanosis, swelling, arthropathy with severe pain in the joints, which leads to their sparing and thereby contributes to the development of contractures and atrophies. This is why restorative measures during the rehabilitation period are so important.
Ischemia in the anterior cerebral artery basin. With the same general symptoms, the peculiarity of the clinical picture is the predominant lesion of the leg in hemiparesis, sometimes in the form of hemiplegia. With a left-sided focus, transient motor aphasia is observed. Mental disorders characteristic of damage to the frontal lobes often appear.
Ischemia in the basin of the posterior cerebral artery. The picture is very diverse depending on the location of the occlusion. Thus, when the entire channel is blocked, there may be hemiparesis, hemianesthesia or hemihyperesthesia, hemiataxia, hemianopsia, and with left-sided localization also sensory aphasia. When only the cortical branch is blocked, hemianopsia is observed, while the lower thalamic branch is blocked - choreoathetosis and painful hyperpathies. The latter are treated with powerful neuroleptics (aminazine).
Ischemia in the basin of the basilar and vertebral arteries. The clinical picture is very diverse: from tetraplegia with bilateral horizontal gaze paresis with thrombotic occlusion of the basilar artery trunk; nystagmus, dizziness, nausea, dysphagia with stenosis of the intracranial vertebral artery - to headaches, dizziness and noise with the common vertebrobasilar insufficiency against the background of cervical osteochondrosis.
Ischemia in the carotid artery basin. Occlusion of the carotid artery (stenosis, thrombosis, embolism) is often asymptomatic, but in the case of neurological disorders they are associated mainly with insufficient blood supply in the middle cerebral and sometimes anterior and posterior cerebral arteries. Usually there is a so-called “flickering” of symptoms. Developing hemiparesis, or even complete hemiplegia with aphasia and the alternating blindness combined with them disappear after a few minutes or hours. This is due to the restoration of blood flow through the circle of Willis, through anastomoses with the external carotid artery. Increased pulsation in the facial arteries and low pressure in the retinal arteries usually indicate stenosis or occlusion of the internal carotid artery on the same side. A thrombus in a great vessel in the neck can be palpated, verified angiographically, and promptly removed by a surgeon.
Lacunar infarction. Develops as a result of occlusion of small penetrating arteries by atherosclerotic plaque or lipohyalinosis, which is more common in arterial hypertension and diabetes mellitus; however, their embolism is also possible. They are mostly asymptomatic; scant single symptoms (dysarthria, clumsiness of the hand, gaze paresis or ataxic hemiparesis) occur against the background of a normal EEG (the diameter of the lesion does not exceed 1 cm).
Transient cerebrovascular accidents. These disorders most often occur in the form of TIA, when the focal deficiency regresses within a day. The specific symptoms of these attacks make it possible to judge the involvement of a particular artery and the localization of the lesion, which is of no small importance for determining treatment tactics. The latter is most often planned taking into account not only and not so much the location as the nature of the lesion. For example, a single attack of speech disorder and hand weakness, relieved after 12 hours, most likely indicates an embolism, and you need to look for the source. Short-term (up to 15 minutes) and frequent (5-10 times a day) single attacks indicate transient disorders of cerebral circulation, local occlusion against the background of atherosclerosis with insufficient development of the collateral system.
Thus, it becomes clear that in case of transient disorders with transient ischemic attacks, the following are especially important:
- insufficiency of collateral blood flow to the ischemic zone;
- state of blood coagulation and anticoagulation systems;
- level of blood pressure, serum cholesterol, the presence of impaired tolerance to carbohydrates, as risk factors for the development of atherosclerotic process (thrombosis, ulceration, embolism, stenosis), leading to vascular occlusion in the brain.
- Diagnosis of ischemic stroke
Despite the fact that a diagnosis can be made based on anamnesis, neurological examination and laboratory data, the following methods are important both in diagnosis and in differential diagnosis and prediction of outcome:
- computed tomography, which allows you to distinguish a heart attack from a hemorrhage, that is, to clarify the nature of the stroke (hemorrhagic or ischemic);
- magnetic resonance angiography, which is not very suitable for emergency situations, but is safe due to its non-invasiveness;
- Dopplerography, especially transcranial, which allows you to assess the state of cerebral blood flow;
- cerebral angiography, which is indispensable if surgery is planned;
- EEG, which identifies areas of cortical and subcortical damage;
- scintigraphy and positron emission tomography, which allow assessing cerebral metabolism and are important in the stage of transient cerebrovascular accidents and at the very beginning of a stroke.
Currently, the improvement of clinical diagnostics and neuroradiological research methods makes it possible to clarify the nature and localization of strokes, as well as to study the accompanying vascular lesions with high frequency and accuracy, which makes treatment more targeted, possible and mandatory.
- Treatment of ischemic stroke
Treatment for ischemic stroke mainly has three goals:
- stroke prevention by reducing risk factors;
- preventing a first or recurrent stroke by removing the underlying lesion - for example, performing a carotid endarterectomy;
- prevention of secondary brain damage by maintaining adequate perfusion in the marginal areas of ischemic zones and reducing edema.
Modern pathogenetic ideas. The development of acute cerebral ischemia triggers pathobiochemical cascade reactions, the outcome of which is the formation of a heart attack.
Analysis of the “ischemic cascade” indicates two possible directions for the treatment of ischemic stroke: the first is improving the perfusion of brain tissue, and the second is neuroprotective or cytoprotective therapy. Early and comprehensive intervention is most promising. The effectiveness of treatment measures depends on the timeliness of their initiation and on the continuity of therapy in all periods of the disease.
System of step-by-step provision of medical care. In Russia, the following system of providing medical care to patients with cerebral stroke has been developed and is functioning: 1. Pre-hospital stage (specialized neurological and linear ambulance teams); 2. Intensive care stage (neurointensive care units, intensive care units, neurosurgical departments); 3. Stage of rehabilitation treatment (neurological departments, rehabilitation departments, centers); 4. Dispensary stage (district neurologist, therapist).
The continuity of treatment measures is determined by the general tactics of patient management and is associated with the solution of treatment and organizational problems. Along with differentiated therapy for strokes, basic therapy aimed at maintaining the vital functions of the body plays an important role. The more severe the stroke, the more necessary, multifaceted and complex basic therapy becomes, which is carried out individually, under the control of laboratory parameters, functions of all organs and systems (see abbreviated diagram of the Department of Neurology and Neurosurgery of the Russian State Medical University, 1997).
Basic therapy. Basic therapy primarily involves proper patient care. For several days the patient should be in a horizontal position with his legs elevated. From the very beginning, it is necessary to prevent hypostatic pneumonia, purulent corneal ulcers, bedsores, and early contractures. After the end of the stroke, within 24-48 hours it is necessary to begin passive movements in the joints, turn the patient in bed, and clear his airways. For persistent vomiting, a nasogastric tube is inserted; for dysphagia, parenteral nutrition is indicated. Control the function of the excretory organs.
| Treatment of strokes involves the combined use of many medicinal, non-medicinal, and surgical agents, prescribed strictly according to indications and under laboratory control, with the participation of cardiologists and, if necessary, resuscitators and neurosurgeons |
Blood pressure control is carried out in order to establish systolic pressure at a level of 10 mm above the “working” numbers, diastolic pressure - no higher than 120 mm Hg. Art. Treatment of concomitant heart pathology is necessary: antiarrhythmic drugs according to indications, anti-infective drugs for septic endocarditis, etc.
Regulation of water-salt metabolism is carried out by infusion therapy under the control of pH measurements, osmolarity of urine and blood, electrolytes and biochemical blood tests.
In the fight against cerebral edema and in order to prevent increased intracranial pressure, dexazone (8 + 4 + 4 + 4 mg IV) is preferable - in the absence of severe forms of diabetes mellitus, internal bleeding, malignant arterial hypertension - or osmotic diuretics (2 times a day reogluman, mannitol 15% - 200 ml IV drip, after 10-15 minutes Lasix 20 mg IV).
Cardiologists and resuscitators should participate in basic therapy.
Anticoagulants. They are prescribed only if it is possible to control blood clotting and in the absence of hemorrhagic diathesis, exacerbation of peptic ulcer disease, severe kidney and liver diseases.
Heparin is administered at a dose of 5,000-10,000 units every 4 hours intravenously, or 1,000 units/hour by drip. The dose is adjusted so that the clotting time or active thromboplastin time is doubled. Coagulation rates are determined daily. In case of heparin overdose, determined laboratory or clinically (petechiae, microhematuria), protamine is administered (5 ml of 1% protamine solution in 20 ml of saline solution). It can be administered, according to the manufacturer's instructions, four hours after the administration of heparin.
After 1-2 days, with the abolition of heparin, they switch to indirect anticoagulants: phenylin, syncumar, warfarin, dicoumarin. Daily monitoring of prothrombin time is necessary. These drugs are prescribed for 3-4 weeks. The effect of indirect anticoagulants is eliminated in urgent cases with plasma (20 ml/kg) or intravenous administration of 50 mg of vitamin K. After the patient is discharged, the prothrombin time can be determined 1-2 times a month.
Antiplatelet agents. The use of antiplatelet agents is due to the fact that platelet aggregation triggers the blood clotting process. They are prescribed from the 3-5th day of a stroke and can be used for years and even for life in courses or permanently. The greatest clinical, although contradictory, experience has been accumulated with aspirin, dipyridanol and ticlid. Aspirin, which selectively suppresses the synthesis of thromboxane A-2, is prescribed mainly at a dose of 1 mg/kg, although there are studies confirming the effectiveness of 30 mg per day, and vice versa, there are studies that indicate the effectiveness of a dose of 325 mg per day. Tiklid is prescribed 250 mg 2 times a day. It is necessary to monitor the condition of the gastrointestinal tract with possible prevention and treatment with antacids, mineral water, herbal medicine, and control of peripheral blood.
Treatment of ischemic stroke in the acute period | ||||||
| * bleeding time * blood clotting * prothrombin * antithrombin * fibrinogen * blood viscosity | 0 | 3 hours | 3-5 days | 7-10 days | 21 day | |
| rtPA!: 0.9 mg/kg i.v., i.v. | End of the acute period | |||||
| Plasma: Day I - 100-150 ml x 1 r.; IV day - x1 rub. | ||||||
| Heparin therapy: 10-15 thousand units/day. through a perfusor or 2.5 thousand units subcutaneously in the abdomen x 4 times. Reduce the dose of heparin by 5 thousand units. Indirect anticoagulants: | phenyline 0.03 g x 2-3 r. or syncumar 8-16 mg/s | |||||
| Hemodilution: rheopolyglucin, rheomacrodex (taking into account systemic hemodynamics, reduce Ht to 30-35%) | ||||||
| Individual antiplatelet therapy (possibly a combination of two drugs) | ||||||
| Trental: 5-10 ml x 2 r. IV jet or x 2 r. IV drip | 0.15-0.2 g x 3 r. per os continue for 2-3 months. + additional REG control | |||||
| Beta blockers: obzidan (anaprilin) 10-20 mg x 4 r. per os | continue for 2-3 months. | |||||
| Calcium antagonists: nimotop 60 mg x 3-4 r. per os | ! 30 mg x 3-4 r. 1.5-2 months | |||||
| Eufillin: 2.4% -7 ml x 2 r. IV drip | x 1 rub. IV drip | |||||
| Stugeron (cinnarizine): 25 mg x 3 r. per os | Continue for 1.5-2 months. | |||||
| Cavinton: 20 mg per 500 ml. physical solution intravenously drip | 10 mg per 500 ml saline. IV drip solution 15 days | 5-10 mg x 3 r. per os for 2-3 months. | ||||
| Tiklid: 250 mg - 1-2 times, long-term + control of peripheral blood | ||||||
| Contrical, gordox i.v. | Aspirin: 1.0 mg/kg per day, long-term | |||||
| Dicinone: 250 mg x 4 r. per day i.v. or x 2-4 times i.m. | If necessary, 250 mg 3 times. continue for 1.5-2 months | |||||
| Neuroprotective therapy: | ||||||
| EEG | Glycine: 1 g x 1-2 r. sublingually | 0.1-0.2 g x 3 r. sublinvally for 1.5-2 months. | ||||
| Control | Nootropil: 12 g/day intravenously for up to 15 days | 5 ml/day. IM for 5 days | 2.4 g x 2 r. per os in table. or in syrup during 2-3 months | |||
| Cerobrezin: 10-20 mg/day IV drip | 5 ml/day. IM for 5 days | 2 days break 3-4 courses | ||||
Individual antiplatelet therapy involves the prescription of vascular drugs with antiplatelet activity: trental, beta blockers, calcium antagonists, stugeron, cavinton, aminophylline. Hordox and Contrical can be administered intravenously in the acute period (see diagram).
Even with the initial manifestations of insufficiency of blood supply to the brain (IBC), it is recommended to prescribe antiplatelet agents containing nicotinic acid (enduracin), polyunsaturated fatty acids (eikonol) or iodine (Splat, spirulina, sea kale).
Vasodilators. Amyl nitrite, papaverine, isoxsuprine can increase cerebral blood flow, but they are not very effective. In addition, vasodilation can lead to a decrease in blood supply specifically in the ischemic zone (“steal”).
Neuroprotective therapy. Neuro- or cytoprotective therapy is necessary to influence the main links of the “ischemic cascade”. From the very first day, Cerebrolysin (10-20 ml), nootropil (12 g per day), glycine (1-2 g sublingually), Semax (6-9 mg intranasally) can be prescribed intravenously. Aplegin 5 ml per day intravenously is effective. After 10-15 days, you can switch from parenteral to oral administration of drugs.
Other means. In recent years, there has been renewed interest in thrombolytics - streptokinase, urokinase and, especially, altepase and nasaruplase, synthesized by genetic engineering methods and having a selective effect on thrombus. However, the results of their studies, as well as those of naloxone (an antagonist of narcotic analgesics), barbiturates, and glutamate receptor blockers, are ambiguous. These drugs do not yet have clinical significance.
Rehabilitation activities. In the recovery phase, when the patient’s condition improves, speech therapy, massage, physiotherapy, reflexology, and therapeutic exercises are important.
Surgery. It is possible only with strict consideration of indications and contraindications and in specialized hospitals and centers. The most common operation is carotid endarterectomy (CE), which is performed for arterial stenosis of more than 70%, as well as for less severe stenosis if there is ulceration of the plaque. The operation can be performed both for prophylactic purposes and urgently during a stroke. Analysis of the literature showed that CE is most often performed in patients who have suffered a TIA or minor stroke as a result of atherosclerotic stenosis of the internal carotid artery.
Surgeries are less often performed for lesions of the extracranial vertebral arteries, subclavian “steal” syndrome, lesions of the aortic arch, cerebellar infarction with compression of the brain stem (decompression of the posterior cranial fossa).
Literature
1. Barkhatov D. Yu., Dzhibladze D. N., Nikitin Yu. M. Functional transcranial Dopplerography in atherosclerotic lesions of the carotid arteries // Journal of Neurology and Psychiatry named after. Korsakova, 1994, 94, 2: 12-16. 2. Vereshchagin N.V., Dzhibladze D.N., Gulevskaya T.S. et al. Carotid endarterectomy in the prevention of ischemic stroke in patients with atherosclerotic stenosis of the carotid arteries // Journal of Neurology and Psychiatry named after. Korsakova, 1994, 94, 2: 103-108. 3. Gusev E. I., Skvortsova V. I., Chekneva N. S. et al. Treatment of acute cerebral stroke (diagnostic and therapeutic algorithms). Educational and methodological literature. M., 1997. 4. Neurology. Ed. M. Samuels. M., 1997. 5. Kistler J.F., Ropper A.H., Martin J.B. Vascular diseases of the brain. Internal Medicine 10: 44-107. 6. Barnett HJM Aspirin in stroke prevention. Stroke 21 (Suppl IV): IV-40, 1990. 7. The Dutch TIA Trial Study Group. A comparison of two doses of aspirin in patients after a transient ischemic attack or minor ischemic stroke // N. Engl. J. Med., 1991. 325: 1261 8. Hass WK et al Control trial of aspirin for the prevention of stroke in high-risk patients // N. Engl. J Med 1989 321:501 9. Petty GW et al. Complications of long-term anticoagulations // Ann. Neurol. 1988. 23: 570 10. Swedish Cooperative Study. High dosage acetylsalicylic acid after cerebral infarction. Stroke 1987.18: 325
Causes and consequences of stroke
The following causes of stroke are known:
- age. People at risk for stroke include older people, especially those who have high blood pressure, lead a sedentary lifestyle, are overweight, or smoke or drink heavily. Currently, stroke is increasingly developing in young people;
- floor. In most age groups, stroke is more common in men than in women. However, it is more severe and more often fatal in women. This is due to the use of contraceptives, hormonal imbalance and emotional imbalance in women;
- family history. In most cases, the closest relatives of patients suffering from stroke have suffered acute cerebrovascular accident;
- smoking. Individuals who smoke more than 20 cigarettes per day have a 2-fold increased risk of stroke;
- nutrition. The predominance of saturated fats, light carbohydrates and excess amounts of table salt in the diet contributes to an increase in blood pressure, which is the main factor in hemorrhagic stroke;
- insufficient physical activity. Lack of regular exercise increases the risk of obesity and increases poor circulation, which contributes to the development of stroke.
- drug use. Drugs, especially methamphetamine and cocaine, are a major factor in the development of stroke in young people. Anabolic steroids, which athletes often take, also increase the likelihood of stroke.
- diseases of the heart and blood vessels. People suffering from diseases of the cardiovascular system, especially those accompanied by cardiac arrhythmias, and peripheral vascular pathology are at increased risk of developing stroke;
- a stroke increases the risk of acute cerebrovascular accident by 10 times;
- Arterial hypertension is the cause of 70% of strokes. Patients with hypertension have a 10 times higher risk of stroke than people with normal blood pressure.
- high cholesterol levels increase the risk of developing atherosclerosis of the cerebral arteries and impaired blood flow through the cerebral vessels;
- Coronary heart disease increases the risk of stroke. Anti-clotting drugs, which are used to treat cardiovascular diseases, dissolve blood clots but also increase the risk of hemorrhagic stroke.
- Atrial fibrillation is a major risk factor for stroke associated with heart rhythm disturbances. 2-4% of patients with atrial fibrillation without warning signs of cerebral bleeding develop a stroke.
The consequences of a stroke are impaired motor, speech, visual, cognitive function, and sensitivity disorders. They are prevented at the Yusupov Hospital by a team of specialists, which includes neurologists, cardiologists, speech therapists, psychotherapists, and rehabilitation specialists.
Seizures after stroke
Some consequences of a stroke can be treated and restored with adequate medical care. These consequences include seizures that occur in women and men after an ischemic or hemorrhagic stroke.
The development of convulsive syndrome is caused by the death of brain neurons and the formation of a focus of necrosis. The body's response to this process is the activation of other neurons to restore blood circulation and stop the pathological process. Necrotic tissue is replaced by a cavity filled with fluid; when a cyst forms, a person does not feel discomfort. However, when neurons are irritated by the cyst, seizures can occur.
After a stroke, seizures can manifest in patients in the form of:
- numbness of one or both limbs at the same time, feeling of a wooden leg or arm;
- contractions of the muscles of the face and neck, resulting in a “mask-like face”, tilting of the head to one side or asymmetry of the face on one side;
- contractions of the facial muscles against the background of numbness of the limbs.
Some patients experience mild tremors after a stroke, while other patients experience short-term cramps throughout the body.
How not to miss a stroke in an old person
We have already said that a stroke in patients over 80 years of age has irreversible consequences. Therefore, as soon as you notice the above signs of illness in your loved ones or acquaintances who have crossed the eighty-year mark, immediately seek help from specialists.
If in young people, during a stroke, only a couple of symptoms appear, then in an old person, a stroke manifests itself in all its diversity, is bright and difficult.
You should be alert to general symptoms: dizziness, headache, poor coordination of movements, numbness on one side of the body.
Hemorrhagic stroke is characterized by the following symptoms:
- sudden and severe headache;
- rapid breathing accompanied by wheezing;
- redness of the skin, especially the face;
- a sharp increase in pressure;
- intermittent heartbeat;
- possible vomiting;
- numbness of the limbs and facial muscles.
In the first minutes of a hemorrhagic attack, immediately after a vessel ruptures, a person may lose consciousness. Depending on how the intracranial hemorrhage is localized, loss of vision and hearing can occur. Vomiting during a stroke can lead to aspiration in an old person, and therefore to respiratory arrest. In the most severe forms, patients experience seizures or even coma.
Signs of ischemic stroke:
- nausea and vomiting due to headache;
- sluggish, impaired movements, inability to lift or even move limbs;
- double vision when looking at objects, a blurry picture before the eyes;
- dizziness and disorientation;
- sensory disturbance;
- numbness of the mouth, inability to speak.
In the ischemic form, symptoms appear gradually. The acute phase is considered to be the first 6 hours after the attack.
If you suspect that an old person has had a stroke, then even before the team of doctors arrives, you can independently determine the primary diagnosis by performing simple tests:
- Ask the patient to smile. If a stroke occurs, one part of the face will remain motionless.
- Have the person try to simultaneously raise or at least stretch their arms forward. In case of a stroke, this can be done with only one hand.
- Try to talk to the victim, pay attention to his articulation. If cerebral circulation is impaired, it is almost impossible to pronounce words.
- Invite a person to stick out his tongue; the tip of the patient will certainly deviate to the side, in the direction of the lesion in the brain tissue.
Even if only one of the tests failed, the patient most likely had a stroke. In this case, there is no time to waste, but it is necessary to provide him with first aid.
Temperature during a stroke in an old person is an important indicator for determining the severity of the attack. The later a person’s temperature rises from the onset of a stroke, the more unfavorable the prognosis for the patient, and the greater the risk of death. High temperature is also a critical indicator that will subsequently prevent the body from recovering. This is due to the fact that hyperthermia worsens the hemorrhage and the hematoma begins to put pressure on the brain.
We recommend
“Recovery of older people after a stroke: tips and practical recommendations” Read more
Temperature after stroke
Temperature during a stroke is an indicator of cerebral hemorrhage, hemorrhagic stroke. With an ischemic stroke, the temperature in most cases is slightly lowered; with a hemorrhagic stroke, the temperature rises.
Timely medical care reduces the risk of developing severe complications. After a stroke, it is difficult to deal with high fever - antipyretics can aggravate the condition of a patient with a hemorrhagic stroke, and in the case of an ischemic stroke cause hemorrhagic transformation.
Temperature after stroke: causes and treatment
Temperature during a stroke is a very important indicator of the patient’s condition. It is most often used to determine the degree of brain damage in a patient. Temperature readings up to 38 degrees are considered to be the maximum permissible.
Stroke studies have shown that the majority of stroke patients had a normal mean temperature upon admission to the clinic. In patients with extensive strokes, the temperature began to rise after a few hours (4-6) to 40 degrees. In patients with moderate strokes, the temperature rose to 40 degrees 12 hours after the stroke. A mild stroke most often occurs without fever or with a slight rise in temperature.
Complications after a stroke
After a stroke, fever often occurs due to the following complications:
- the damage occurred over a large area of the brain;
- swelling of brain tissue has developed;
- during a stroke, the thermoregulation center in the brain was damaged;
- complication after a stroke – pneumonia;
- an allergic reaction to medications developed.
In cases where the cause of the increase in temperature is its central genesis, doctors perform craniocerebral hypothermia. The brain is cooled through the outer covering of the head using special equipment. This method increases the brain's resistance to oxygen starvation, reduces the risk of developing cerebral edema, relieves existing edema, and reduces tissue temperature.
Treatment, prevention, rehabilitation
It is very important to have time to provide assistance to a patient during a stroke in the first six hours from the onset of the attack. At the initial stage, problems associated with impaired respiratory and cardiac function are eliminated.
It is necessary to normalize blood circulation in the brain, stabilize the acid and electrolyte composition of the blood. To do this, the patient must be given special medications: for ischemic stroke, Actalyse is used, the drug actively counteracts the formation of blood clots in the blood vessels and restores normal blood flow. During the treatment of ischemic stroke, medications such as Heparin and Fragmin are prescribed, which prevent the formation of blockages and blood clots in the circulatory system, Cardiomagnyl, a blood thinner, Trental or Sermion as a vasoactive agent, Glycine , "Tiklid", some antioxidants and others.
What preventive measures should each person take to prevent a stroke? It turns out that protecting yourself from this disease is very easy. It is necessary to get rid of bad habits: quit smoking, give up drugs and alcohol, lead a healthy lifestyle, avoid stressful situations.
It should be remembered that curing a stroke quickly and without consequences is an extremely difficult task, but it can be done. Modern medicine uses all kinds of means for this: drug treatment, physiotherapy, occupational therapy, speech therapy and many others.
Signs and symptoms after a stroke
The symptoms of a stroke largely depend on the cause of the disease. The first signs of a stroke are the following symptoms:
- sudden numbness or weakness in an arm or leg on one side of the body;
- confusion;
- Strong headache;
- speech disorder;
- decreased visual acuity;
- dizziness;
- loss of balance or coordination.
The speed at which symptoms of an ischemic stroke appear may indicate its origin: if an acute cerebrovascular accident is caused by an embolism, the disease is sudden. Headache and seizures may develop within seconds of arterial thromboembolism.
In patients with the consequences of a stroke, there are three main types of disorders:
- damage, defect. The following damages after a stroke are distinguished: motor, cognitive, emotional-volitional, speech, visual, sensory, sexual and pelvic disorders;
- impaired ability. Expressed in impairment of walking and self-care;
- impairment of social functioning. It is expressed in the restriction of the implementation of the social role that was the norm for the patient before the illness.
Symptoms after a stroke go away if doctors begin rehabilitation measures in a timely manner. When a patient is admitted to the neurology clinic of the Yusupov Hospital, a team consisting of the following specialists is included in the rehabilitation process:
- neurologists;
- therapists;
- kinesitherapy specialists;
- aphasiologists;
- massage therapists;
- physiotherapists;
- acupuncturists;
- psychologists;
- biofeedback specialists.
Muscle pain due to stroke
Muscle pain after a stroke, which should be treated immediately, occurs in most patients. Muscle soreness can interfere with the body's recovery. Post-stroke pain can be strategic or thalamic. Strategic pain occurs in the area of the brain that controls sensations, particularly pain, and is caused by spasms. Thalamic pain appears after a stroke in one side of the body several months after the circulatory disorder.
The occurrence of pain after a stroke can be associated with various factors. Neurologists and rehabilitation specialists advise patients to follow recommendations that will prevent the onset of this condition. Measures to prevent muscle pain after a stroke:
- do not take hot baths;
- prefer clothes made from natural materials, do not wear light clothes;
- be in a comfortable position and avoid tightly grouping the body;
- do not put pressure on the affected side;
- use special devices for paralyzed and weakened limbs;
- fix the paralyzed arm while sitting so that the pain localized in the shoulder does not get worse;
- When moving, support from another person is desirable.
If you have pain in the legs after a stroke, it is important to trust treatment to qualified neurologists and rehabilitation specialists.
Age of stroke
Stroke is a disease that scientists are still researching to this day; it is a catastrophe that can strike at any age. The greatest likelihood of the disease is among older people, but there is a sad tendency to develop a stroke at a young age under 30, when there is no obvious predisposition to this.
In youth, people do not pay attention to headaches, surges in blood pressure, dizziness and nausea, not assuming that all of these are quite serious symptoms of a pre-stroke condition. In order not to be bedridden, to avoid the negative consequences of a stroke, you need to contact the specialists of the Unimed-S clinic in time, undergo a proper examination, take blood tests, and receive valuable recommendations.
Features of stroke in older people
Age is one of the significant factors in the development of acute vascular pathologies of the brain that impair blood circulation. Diseases of the blood vessels in older people are much more severe than in young people. This is due to physiological changes in the body, and in particular in the central nervous system, such as:
- reduction in brain volume and weight;
- thinning of the leptomeningeal membranes;
- senile neuronal atrophy;
- degenerative changes in white matter;
- decreased functional activity of neurons;
- neuronal death caused by electrolyte imbalance;
- reduction of the blood-brain barrier;
- pathological changes in the cerebral ventricles.
About 80% of stroke cases are diagnosed in people over 70 years of age. And, unfortunately, the prognosis for recovery is very often unfavorable. The consequences of stroke in older people are difficult to predict, since it is difficult for such patients to choose effective therapy.
Causes of stroke in older people
Among the causes of stroke in older people, etiological factors and risk factors are distinguished. The former cause the disease itself, while the latter increase the likelihood of pathology occurring. The main causes of acute disorders of blood flow in the brain include:
- arterial hypertension;
- vasculitis and angiopathy;
- improper use of drugs that affect blood clotting;
- neoplasms in the cells of nerve or connective tissues;
- changes in heart rate;
- atherosclerosis of the carotid arteries;
- hormonal imbalance, which increases the risk of blood clots.
The main risk factors for stroke in older people include:
- gender (statistically, men are more susceptible to extensive bleeding into the brain);
- presence of cardiovascular diseases;
- increased cholesterol levels in the blood;
- history of micro-strokes.
As a rule, a stroke is preceded by certain vascular and cardiac diseases. Some of them are systemic atherosclerosis and atrial fibrillation, which develop at the age of 85 years.
Systemic vascular atherosclerosis
This disease is heterogeneous plaques that form in medium and large arteries, including the brain. Elderly and senile age are the main risk factors for the development of atherosclerosis.
Frequent atrial fibrillation after 85 years
Heart rhythm disturbances that lead to an irregular heartbeat indicate the presence of atrial fibrillation. The sinus node cannot cope with the coordination of the heart rhythm, which is why the upper chambers flicker chaotically. As a result, insufficient blood enters the ventricles. The main symptoms of atrial fibrillation are:
- trembling in the chest;
- cardiopalmus;
- irregular heart rhythm;
- dyspnea;
- pain in the chest;
- dizziness;
- fatigue, drowsiness;
- increased anxiety and restlessness.
Many people live with this disease for decades. It is not a direct threat to life, but when a person reaches old age it leads to a number of complications, including stroke.
Stroke in people over 70 years of age
With age, cerebral circulation deteriorates. These disorders are explained by natural aging changes, due to which the body's compensatory reserves decrease. As a result, the walls of blood vessels become brittle, the inner lining of the arteries is affected by atherosclerotic plaques, and cases of sudden jumps in blood pressure become more frequent.
The consequences of a stroke in elderly patients (over 70 years of age) are very life-threatening and radically change it. The first episode of cerebral vessel rupture leads to coma in more than half of the cases. The recovery process after an acute cerebral circulatory disorder is difficult and lengthy.
Signs of stroke in older people
In most cases, the disease manifests itself almost immediately. Deprived of normal blood supply, brain cells die, which is accompanied by the following symptoms:
- severe headache;
- dizziness;
- fainting, short-term loss of consciousness;
- impaired coordination of movements;
- deterioration of speech and pronunciation (slowness, deterioration of diction, inability to reproduce sounds);
- decreased vision, darkening of the eyes, blurred and unclear images;
- confusion, absent-mindedness;
- disorientation in space.
Signs of stroke in older people have some peculiarities. A vascular accident in the brain occurs regardless of the time of day, but more often develops in the early morning or evening. In older patients, the condition often worsens gradually over several days. This is due to the fact that cerebral hemorrhage occurs quite slowly.
How long do they live after a stroke: statistics in detail
The life expectancy of a person after a stroke is highly individual. In 20% of cases, a person’s death occurs instantly.
Studies have shown that in the first 30 days the mortality rate is 30-40%; after the first year after a stroke, approximately 50% of patients die.
The repeated process of cerebral circulatory disturbance increases the possibility of death. Often, if a patient has a first stroke, he can live up to 10 years, but with a second attack on the brain, life expectancy is no more than 3 years.
The reason for such a high mortality rate after a second stroke is that after the first attack, lesions remain in the brain.
Dependence on age and gender
With hemorrhage before 40 years of age, the death rate is 15%, after 50 years of age – 45% of cases.
Women have a higher mortality rate than men – 39% versus 29%.
It is several times more difficult for newborns and people aged 65 years and above to survive a stroke. This is due to age-related factors in blood vessels and their walls, which cannot recover quickly. In newborns, the cells have not yet formed. Such wall problems lead to:
- inflammation of the cranial nerves;
- damage to the vascular system;
- hemorrhage.
Lesion size
This is the main aspect that affects how long a person can live after a stroke. Tissues susceptible to necrosis take a long time to recover.
The larger the affected area, the worse the prognosis.
How consequences affect the outcome
If after a stroke the patient begins to develop concomitant pathologies (paralysis, numbness or impaired psychological functions), then life expectancy decreases several times.
In addition, these consequences create the preconditions for the occurrence of bedsores. Bedsores form irreparable processes in the blood circulation of the whole body. Mental disorders require round-the-clock care for the patient, since he is not able to soberly assess the situation and take medications on time.
Life expectancy without movement
A person who is immobilized after an attack does not have the necessary desire for long-term recovery. Because of this psychological feature, a person does not strive to adhere to all norms and procedures, which is why muscle endurance decreases, fibers lose tone, and blood flow in the limbs is disrupted.
This ultimately leads to blood clots and tissue necrosis, which poison the blood.
Psychological recovery of the patient
After suffering a stroke, all patients require mandatory psychological rehabilitation. The specialist’s actions should be aimed at developing in the patient an adequate attitude towards his health, activating the desire to recover faster after an attack, and returning to normal social life.
The psychological recovery program for each person is developed individually. In this case, the doctor must take into account the degree of depression, the presence of psychological health complications due to hemorrhage or ischemia, the patient’s personal character traits, and his living conditions.
The psychologist works not only with the victim, but also with his loved ones. Relatives must clearly understand how a person feels after an attack and how to help him. A favorable emotional atmosphere, positive attitude and understanding from relatives help the patient recover faster.
Support from loved ones is valuable after an attack
How long do people live after a stroke, the rules of recovery, the importance of the psychological situation and many other nuances were described by Sergei Vikentievich Kuznetsov. The book “Life after a stroke” contains a lot of valuable information for the person himself and his loved ones.
Taking medications
Life expectancy after a stroke largely depends not only on medical care, but also on the literacy of further rehabilitation. After being discharged home, you should not let the disease take its course. A person must strictly follow the recommendations of doctors. This primarily concerns taking medications. The most commonly prescribed drugs are those designed to improve blood circulation in the brain area. nootropic drugs increase the production of phospholipids and the synthesis of nucleic acids, improve glucose absorption, and reduce excessive activity of nerve cells.
The rehabilitation period includes the use of medications
In addition to nootropics, patients are prescribed antispasmodics, antidepressants, and sedatives. More than 30% of people after an attack have an unstable emotional state, suffer from depression and sleep disorders. This is due to the fact that it can be quite difficult to return to normal life on your own, which is associated with many complications after a stroke.
Important! In the family where the person is after suffering an attack, a positive emotional environment should reign.
How to recover and prevent another stroke for an old person
For older people after a stroke, even in a hospital setting, they offer classes on special simulators and select individual exercises that need to be continued at home. The basis of the rehabilitation period, along with taking medications and physiotherapeutic procedures, is a properly selected diet:
- minimum amount of sugar and salt in the diet;
- reducing the consumption of animal fats (pork, lamb, butter, some dairy products);
- The basis of the diet is lean vegetable soups, vegetable oils, cereals, fruits and vegetables.
It is recommended to steam dishes and eat boiled or baked foods. To avoid difficulty chewing, it is better to eat fairly well-chopped food.
In the post-stroke period, many patients have a deteriorating emotional state, feel morally depressed, and have their usual sleep patterns disrupted. What sedatives does a doctor usually prescribe for an old person after a stroke? As a rule, these are sleeping pills and antidepressants: Doxepin, Mirtazapine, Trazodone. Nicergoline is used as an additional medicine, which not only reduces the symptoms of insomnia and mental disorders, but also helps reduce the tone of the cerebral arteries and improves blood flow. It is worth warning that long-term use of these drugs can be addictive. Beware of this and listen to medical advice.
In recent years, PNF therapy (proprioceptive neuromuscular facilitation) has been actively recommended for older people who have suffered a stroke, a technique that allows them to regain the ability to move. Simple physical exercises improve motor functions and prevent the development of complications - paralysis and muscle dystrophy.
Other methods are also effective in treating stroke in older people:
- soft tissue manual therapy - working out all muscles allows you to restore their tone;
- Vojta therapy - through targeted pressure on certain areas of the body, the activity of motor muscles and reflexes is triggered. In some cases, completely paralyzed patients after a course of procedures were able to roll over and crawl on their own;
- The Castillo Morales method is a set of exercises that allows you to restore the breathing and swallowing functions, as well as the speech of the victim. Usually carried out in conjunction with psychological therapy;
- kinesio taping - special elastic patches glued to the patient’s skin not only improve microcirculation and lymph outflow, but provide additional support and strengthening to the joints;
- The Mulligan concept is a type of manual therapy method that has proven itself in the treatment of stroke in an old person. Special manipulations by the doctor alleviate the excessive pain of the actions, and the patient, overcoming the pain, can improve the exercises day by day;
- bobat therapy (neurodynamic rehabilitation) is a practice that helps to correct movement patterns and overcome lack of movement.
All these techniques are usually used to treat stroke in an old person in a rehabilitation center under the guidance of experienced doctors. Additionally, patients are prescribed physiotherapeutic procedures, magnetic brain stimulation to restore speech, and transcranial stimulation to improve vascular function.
You can also achieve good results after acupuncture, which helps normalize muscle activity and restore motor functions, improve tissue condition, and form reflexes.
Treatment of a stroke in an old person and the subsequent rehabilitation period is a rather lengthy set of measures that falls on the shoulders of the patient’s relatives and friends. The choice of good doctors, strict adherence to all recommendations, the desire and efforts of the patient himself, the patience and responsibility of relatives help many who have suffered an attack to return to a comfortable standard of living.
Precursors of stroke
Symptoms before an attack appear within a few days. However, many do not pay attention to them, because the signs of an impending stroke disappear on their own.
How to recognize the proximity of a “blow”? The most important harbingers:
- headaches that appear suddenly and go away quickly;
- weakness unexpected for a person;
- causeless nausea;
- short-term dizziness;
- frequent mood changes.
You also need to pay attention to symptoms such as:
- visual and hearing impairments;
- slow pulse;
- numbness of the limb;
- flushes of blood to the face;
- disturbance of speech function or coordination of movements;
- severe sweating.
If you have these symptoms, you should immediately consult a doctor, as it is still possible to prevent a stroke.
Within 3 hours from the moment of formation of a brain lesion, acute manifestations of a close “impact” occur:
- difficulty swallowing;
- unbearable headache that leads to fainting;
- severe dizziness;
- vomit;
- convulsions;
- breathing problems;
- tachycardia.
At this stage, the victim requires urgent hospitalization. With timely provision of first aid, the likelihood of severe complications will be reduced.
Treatment of stroke in old age
The most effective therapy for elderly patients is thrombolytic therapy. However, Western clinics often refrain from this method, as they believe that thrombolysis can cause subarachnoid hemorrhage. It is also very difficult to observe the effect of treatment during this intervention. The best treatment results were achieved by endovascular methods and intra-arterial thrombolysis. These treatments significantly reduce the negative effects. The use of antiplatelet drugs gives good results. Thus, taking aspirin in the first hours of a stroke significantly reduces the likelihood of subsequent development of paroxysms. Antihypertensive therapy is carried out both as a primary measure and during secondary prevention. The sooner measures are taken to restore post-stroke and physiological functions, the easier it is for an elderly patient to endure negative consequences and complications.