Brain glioma is the most common type of tumor that grows from glial tissue, which makes up the supporting cells of the nervous system. Gliomas account for about 60% of all tumors localized in the brain. The name of the types of gliomas - astrocytomas, ependymomas and others - comes from the name of the cells that form the tumor.
Services for the diagnosis and treatment of brain glioma are offered by the leading multidisciplinary medical center in Moscow - Yusupov Hospital. Positive treatment results are achieved thanks to the high professionalism of the oncology center’s doctors and advanced technologies used to combat brain tumors.
Classification
- Astrocytomas are the most common type of glioma, localized in the white matter of the brain. Depending on the type, astrocytic glioma of the brain can be fibrillary (protoplasmic, gemistocytic), anaplastic, glioblastoma (giant cell, gliosarcoma), pilocytic astrocytoma, pleomorphic xanthoastrocytoma, and subependymal giant cell astrocytoma.
- Ependymomas - can occur in 5-7% of cases of brain tumors, are characterized by typical localization in the ventricular system of the brain.
- Oligodendrogliomas account for 8 to 10% of all brain tumors and develop from oligodendrocytes.
- Chiasmal glioma - spreads along the optic nerve into the orbital cavity, can grow into the hypothalamus, and affect the third ventricle of the brain. This tumor causes endocrine imbalance, metabolic disorders, decreased vision, and is characterized by intracranial hypertension, depending on the location and size of the tumor.
- Mixed gliomas – oligoastrocytomas, anaplastic oligoastrocytomas.
- Neuromas make up 8 to 10% of tumors.
- Choroid plexus tumor is a rare type of glioma, occurring in 1-2% of cases.
- Neuroepithelial tumor of unknown origin - this group includes astroblastoma and polar spongioblastoma.
- Diffuse glioma of the brain stem is a tumor with a high degree of malignancy, cancer of the central nervous system. People of any age are affected, but the tumor is rare in adolescents and children. The survival prognosis for this type of tumor is poor. Diffuse glioma develops in the area of the brain in which all the important nerve connections are located, providing communication between the analyzing nerve centers of the brain and the impulses of the musculoskeletal system of the extremities. The tumor very quickly causes paralysis.
- Neuronal and mixed neuronal-glial tumor - occurs in extremely rare cases (up to 0.5%). This group includes gangliocytoma, ganglioglioma, neurocytoma, neuroblastoma, neuroepithelioma).
- Gliomatosis cerebri.
Malignant and benign gliomas
Neoplasms can be benign or malignant. The exact type of tumor is determined by a neurologist or neurosurgeon based on the diagnostic data.
Experts distinguish three main types:
- astrocytomas;
- ependymocytes;
- oligodendrogliocytes.
Depending on the degree of malignancy, tumors come in several types. Juvenile and giant cell astrocytomas are considered benign. They are classified as the first degree and are considered the most harmless. Glioma of the second stage is borderline. It is growing slowly and has a favorable prognosis. But without timely treatment, it easily transforms into a tumor of the third and fourth degrees of malignancy.
Degrees
There is a WHO classification, according to which gliomas are divided into four grades:
- Grade I – slow-growing benign glioma, which is associated with a long life expectancy;
- Grade II – slowly growing “borderline” brain glioma, which tends to progress to grades III and IV;
- III degree – malignant glioma;
- IV degree – fast-growing glioma of the brain: the life expectancy of patients with this diagnosis is significantly reduced.
A little about terms and erroneous conclusions
Patients or their relatives who do not have a medical education sometimes have doubts about the need to remove a tumor node using a radiosurgical unit. This is due to the fact that the medical report does not (and cannot write) “inoperable brain cancer,” but refers to a tumor, neoplasm, area of neoplastic growth, etc. The validity of irradiation of a benign tumor raises especially many questions.
In this case, people are misled by the peculiarities of medical terminology. It must be borne in mind that in the brain tissue there are no epithelial cells that can degenerate and give rise to a true cancerous tumor - carcinoma. That is, brain cancer as such does not exist. But this circumstance does not mean that the detected outbreak is harmless. On the contrary, highly malignant brain tumors are distinguished by extremely aggressive “behavior”, although they are not cancerous.
Moreover, in some cases, benign nodes can cause no less serious problems. For example, if they disrupt blood circulation, they compress the centers of nervous and neurohumoral regulation.
Symptoms
The symptoms of brain glioma depend on the location of the tumor, its size, and it consists of general cerebral and focal symptoms.
Most often, brain glioma manifests itself as persistent and constant headaches, in which patients experience nausea and vomiting, after which there is no relief, as well as convulsions.
In addition, depending on which part of the brain is affected by glioma, patients have speech impairment, weakened muscles, and may experience paresis and paralysis of the arms or legs, face and other parts of the body. Visual or tactile function, coordination of gait and movements may be impaired.
The psyche may change, and the development of behavioral disorders is often noted. In addition, memory and thinking are impaired in patients with brain gliomas. Due to impaired circulation of cerebrospinal fluid, intracranial hypertension and hydrocephalus develop.
Positron emission tomography (PET) for glioblastoma
Positron emission tomography is a useful adjunct in the detection of glioblastoma multiforme, especially after surgery to remove it. In this case, when performing CT and MRI, the distinction between residual or recurrent tumor and postoperative edema or scar is often difficult. The use of 18-fluorodeoxyglucose (FDG) PET is effective for tumors with high metabolic activity that actively take up glucose, whereas such FDG accumulation is not observed for postoperative edema or scar tissue. In cases where the tumor has been resected, the detection of increased FDG uptake in the surgical area is a reliable indicator of disease recurrence. However, after radiotherapy, increased activity can be observed in the surgical site without tumor recurrence. False-positive results are found after radiation therapy, when active granulation tissue can metabolize FDG, which can reduce the sensitivity of the method. An epileptogenic focus located adjacent to the surgical site may also show increased metabolism on PET, especially if epileptic activity is high. All of these options require assessment by an experienced neuroradiologist. If the initial evaluation of the images does not provide a clear answer, a second opinion on a PET scan may be helpful.
Diagnostics
Diagnosis of brain glioma is based on the results of a thorough neurological examination and other special diagnostic tests.
First of all, the doctor at the Yusupov Hospital Oncology Center assesses the condition of reflexes and skin sensitivity, and motor function of the limbs. If the patient complains of deterioration in visual function, he is prescribed a consultation with an ophthalmologist.
The neuromuscular system is assessed using instrumental diagnostic methods - electromyography and electroneurography. In addition, a lumbar puncture is performed to identify atypical cells in the cerebrospinal fluid. This study is also used for ventriculography and pneumomyelography.
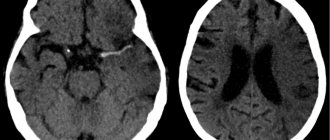
Modern imaging methods that provide layer-by-layer images of brain tissue are of great importance in the diagnosis of brain tumors. These include computed tomography (CT), magnetic resonance imaging (MRI). These studies are considered quite safe and very informative; they help determine the location, size, shape and structure of the tumor.
To determine the displacement of the midline structures of the brain, an ultrasound examination of the brain (M-echo) is performed.
Additionally, cerebral contrast angiography (x-ray examination of cerebral vessels), electroencephalography, scintigraphy and PET may be prescribed.
Make an appointment
Reasons for the ineffectiveness of chemotherapy and radiation treatment using outdated methods
Due to the special organization and functions of the central nervous system, the effectiveness of irradiation of a brain tumor using traditional radiotherapy installations was extremely low, as was the benefit from taking previous generation chemotherapy drugs. This happened because:
- radiotherapists could not use high enough doses of ionizing radiation, since it destroyed not only the tumor, but also healthy brain tissue located in the path of the radiation flow;
- Chemotherapists had practically no drugs at their disposal that had the ability to penetrate the blood-brain barrier, act selectively and not cause significant harm.
With the advent of new technologies, equipment and drugs in the arsenal of neuro-oncologists, the situation has changed dramatically.
Treatment
Like any malignant tumor, brain glioma is treated with three main methods that are used in modern oncology - surgery, radiation therapy (including radiosurgery) and chemotherapy.
The gold standard treatment for brain glioma is surgery. If the tumor is operable, surgery is performed to remove the tumor.
Radiation therapy is performed before and after surgery. For inoperable tumors (if the glioma is localized in a hard-to-reach place), this method is used as a separate method. Today, traditional radiation therapy has been replaced by stereotactic radiosurgery.
Chemotherapy treatment of glioma can be used both preoperatively and postoperatively.
Surgery
The operation to remove malignant glioma is open, involving craniotomy, during which the skull is opened. The main goal of surgery is to remove as much of the tumor as possible while leaving healthy brain tissue intact, thereby preventing neurological damage. A certain localization of gliomas allows the effect of surgical treatment to be achieved up to 98%.
No operation to remove a tumor guarantees a 100% result, since there is always a possibility that cancer cells remain in the brain tissue. However, surgical intervention eliminates compression of surrounding brain tissue and the symptoms of glioma, as well as restores cerebrospinal fluid circulation if intracranial hypertension is present.
The effectiveness of surgical treatment of brain glioma largely depends on the skill and experience of the operating specialists. Treatment of brain tumors at the Oncology Center of the Yusupov Hospital is carried out using high-precision tomographs and neuronavigators, thereby minimizing the likelihood of a relapse of the disease.
Radiation therapy
Radiation therapy may be given before surgery to shrink the tumor before excision, or after surgery to kill any remaining tumor cells.
In addition, this method can be used as an independent method when the tumor is localized in a hard-to-reach place, which prevents its surgical removal. In this case, radiation therapy does not completely destroy the tumor, but can significantly stop its growth.
Traditional radiation therapy is accompanied by a number of undesirable effects: patients experience nausea, decreased appetite, and increased fatigue. At the site of radiation exposure there is a high probability of hair loss and the development of radiation dermatitis. As a rule, side effects of radiation therapy appear 10-14 days after irradiation.
In addition, late complications of radiation exposure are known: patients experience memory impairment to varying degrees, and radiation necrosis may develop (scar tissue forms around the dead tumor tissue).
Radiosurgery
Due to the fact that surgical treatment of brain tumors does not guarantee a complete cure, a relapse of the disease may occur after surgery. Therefore, it is advisable to use additional treatment methods - radiation therapy and chemotherapy. As a rule, relapses are localized at the borders of healthy tissue with the area where the tumor was removed. In such cases, it is recommended to use radiosurgery: cyber knife, gamma knife, Novalis.
Radiosurgery is an innovative method of radiation therapy, the essence of which is to irradiate a glioma with a beam of radiation from different angles, which ensures that radiation reaches the tumor and minimal irradiation of soft tissues.
During the procedure, the position of the patient's head and the location of the tumor are constantly monitored using computed tomography or magnetic resonance imaging, so that the radiation beam is directed exclusively to the malignant neoplasm.
This method is non-invasive, as no incisions are required to perform it. Thanks to this, there is no risk of intraoperative complications and side effects associated with traditional radiation therapy.
In addition, radiosurgery is an absolutely painless method that does not require anesthesia or preparatory measures, and there is no recovery period. The only limitation to radiosurgery is the size of the tumor.
It is important to understand that the effect of radiation therapy occurs gradually, unlike surgery. However, radiosurgery is often the only alternative treatment for inoperable brain gliomas.
Description, causes and classification of pathology
The disease is characterized by the development of a tumor process that originates from “auxiliary” brain cells surrounding the main neurons - glial fibers. Neuroglia transmit nerve impulses from neurons, protect, participate in metabolic processes, and normalize the functionality of neurons. Glioma is a fairly common tumor pathology, as it is detected in more than half of patients in whom brain tumors are diagnosed. Develops as a primary disease. According to external signs, it can be differentiated by color from light pink to dark red node, which does not have clear boundaries. Very rarely, ingrowth of its processes into adjacent brain tissue or bone structure is observed.
The shape of the formation resembles a roundness or a cylinder narrowed at the ends. At the initial stage of development, its diameter is two to three millimeters; at an advanced stage it can reach the size of a large apple. Characteristic is the growth of the tumor over time and the absence of aggressive metastases, while the contours of the tumor are so blurred that their features cannot be completely determined even with multiple magnification. As the abnormal cells grow into adjacent tissues, the surrounding neurons and glia slowly degenerate. There is often a discrepancy between the number and degree of neurological disorders and the small size of glioma.
If we classify the types of disease, we can distinguish three groups of tumors formed from different types of glial cells:
- Astrocytoma. It is formed from astrocytes and accounts for almost half of all cases of this disorder.
- Oligodendroglioma. Covers about ten percent of all cases.
- Ependymoma. It grows from ependymocytes, the incidence rate is the same as the previous type.
There are cases when mixed types of formations are diagnosed, involving the vascular structure, as well as tumors of unknown nature. There are 4 groups based on the degree of malignancy:
- Slowly developing benign neoplasm.
- Borderline stage, growing at a slow pace and having only one criterion for malignancy - degeneration of adjacent cellular structures. This stage can develop into subsequent malignant forms.
- A dangerous form that includes multiple signs of the cancer process.
- The final stage, characterized by the formation of necrotic foci of destroyed and dying tissue.
Treatment of glioma at Yusupov Hospital
Oncologists at the Yusupov Hospital have enormous experience and effective methods of treating cancer. An individual treatment program is drawn up for each patient, based on the results of a thorough diagnostic examination. The Oncology Center of the Yusupov Hospital is equipped with innovative equipment for high-quality diagnosis and treatment of gliomas and other brain tumors.
An appointment with an oncologist can be made by calling the Yusupov Hospital or online on the website using the feedback form. The coordinating doctor will answer all your questions and tell you about the cost of medical services and the conditions for hospitalization of the patient.
Make an appointment