Brain meningioma (ICD 10 code – D32.0) is a neoplasm that originates from the arachnoid (arachnoid) membrane of the brain. Brain meningioma has a clear outline morphologically and looks like a horseshoe-shaped or spherical node, most often fused with the dura mater of the brain.
At the Yusupov Hospital, qualified specialists use the most advanced technologies and time-tested effective methods to treat meningioma: radiation therapy, stereotactic radiosurgery, high-quality removal of brain meningioma. Recovery after surgery is carried out in the rehabilitation department of the Yusupov Hospital under the careful supervision of competent rehabilitation doctors and attentive medical staff.
Meningioma: what is it?
As a rule, meningioma is benign in nature, however, like any other tumor localized inside the skull, benign meningioma of the brain is considered relatively malignant, accompanied by symptoms associated with compression of the brain matter. Malignant brain tumor (meningioma) is a less common disease characterized by aggressive growth and a high recurrence rate after surgical treatment.
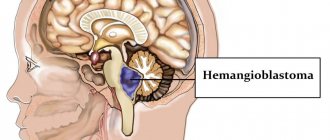
Most often, brain meningioma is localized in the area of the foramen magnum, cerebral hemispheres, pyramid of the temporal bone, wings of the sphenoid bone, tentorial notch, parasagittal sinus and cerebellopontine angle.
In most cases, meningioma is located in a capsule. The tumor is not characterized by the formation of cysts; it can be small, just a few millimeters, or reach large sizes - over 15 centimeters in diameter. If a meningioma grows towards the brain, a node forms, which over time begins to compress the medulla. If a tumor grows towards the bones of the skull, over time it grows between the cells of the bone and causes thickening and deformation of the bone. The tumor can grow simultaneously towards the bone and brain, then nodes and deformation of the skull bones are formed.
Make an appointment
Brain oligodendroglioma - what is it?
Oligodendroglioma has varying degrees of malignancy and can develop at any age, however, it is more common in adults. Men get sick more often than women, approximately 25-30%. Oligodendrogliomas account for about 3% of all tumors in the brain. Neoplasms of this type are characterized by slow expansive-infiltrative growth. If the tumor is localized in the white matter of the hemispheres, then its volume can reach significant sizes. In most cases, characteristic signs appear late. It often takes 3-5 years from the formation of the tumor until the first symptoms begin to appear.
Note. It may take years to make a correct diagnosis, since early clinical symptoms are unspecific and it is often difficult to understand the true cause of unfavorable symptoms.
Features of location and histology
Most often, oligodendroglioma forms along the walls of the ventricles of the brain. Pathogenic cells grow in them and also spread to the cerebral cortex. Most rarely, oligodendroglioma forms in the brain stem, cerebellum and nerves innervating the visual analyzers.
The tumor itself has a pale pink tint, with clearly defined boundaries. This type of neoplasia is characterized by the presence of a cyst-forming process, so there may be cysts (separate cavities filled with exudate) inside the formation. Cytohistological features of brain oligodendroglioma are the presence of a large number of myelin fibers in the tumor. There are individual large cells with well-structured hyaloplasm and small cells with poorly differentiated contents, but clearly visible and relatively large nuclei.
Note. A distinctive feature of oligodendroglioma from other brain tumors is the presence of petrificates (calcifications) in the tissue.
Reasons for development
The direct causes of the development of meningiomas have not been reliably studied to date. However, there are a number of factors that can provoke their occurrence:
- Most often, brain meningioma is diagnosed in mature patients, after 40 years;
- It is known that women are more susceptible to developing brain meningioma than men. This is due to the fact that tumor growth is greatly influenced by female sex hormones;
- the occurrence of various tumors in the brain is often associated with high doses of ionizing radiation;
- the influence of such negative factors as chemicals and toxic substances, trauma, exposure to a mobile phone and others;
- A significant role in the development of meningioma belongs to genetic diseases, one of which is neurofibromatosis type 2, which causes multiple malignant meningiomas.
Reasons for the appearance of the tumor
A single cause for the development of cancer has not yet been identified, although active searches are being conducted in this direction. For now, the multifactor theory prevails. It states that several factors can simultaneously take part in the occurrence of a tumor. Most often this is:
- genetic predisposition (if close relatives had cancer).
- belonging to the age category (usually over forty-five years, with the exception of medulloblastoma).
- exposure to harmful production factors, especially chemicals.
- exposure to radiation.
- race (oncological diseases are more common in people belonging to the Caucasian race, with the exception of meningioma, which is typical for Negroids).
Symptoms and signs
Meningioma of the brain (ICD 10 - D32.0) is characterized by relatively slow growth, so it can develop asymptomatically for a long time.
One of the first symptoms is a headache - dull, bursting or aching. It is distinguished by its diffuse nature and localization in the area of the back of the head, forehead or temples.
The occurrence of other symptoms is associated with the localization of the tumor (compression of certain brain structures). Such symptoms are called focal.
Brain meningioma may be suspected if the following symptoms are present:
- paresis of the limbs (severe weakness, decreased sensitivity, the appearance of pathological reflexes);
- loss of visual fields and other visual disorders (decreased visual acuity, double vision). A characteristic symptom is ptosis - drooping of the upper eyelid;
- deterioration of hearing function;
- reduction or complete loss of smell, olfactory hallucinations;
- epileptiform seizures;
- psychoemotional disorders, behavioral disorders - these symptoms most often manifest themselves as meningioma of the frontal lobe of the brain;
- thinking disorders;
- impaired coordination and gait;
- increased intraocular pressure;
- nausea and vomiting that does not bring relief.
If the outflow of cerebrospinal fluid is disrupted, hydrocephalus and cerebral edema occur, as a result of which patients develop persistent headaches, dizziness, and mental disorders.
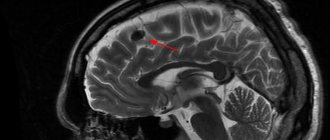
Diagnostics
The most informative and accurate methods for diagnosing meningioma are computed tomography (CT) and magnetic resonance imaging (MRI). As a rule, these studies are carried out with contrast. CT and MRI can determine the size of the tumor, its location, the extent of damage to surrounding tissues and possible complications.
Magnetic resonance spectroscopy (MRS) is used to determine the chemical profile and nature of the neoplasm. Positron emission tomography (PET) allows identifying foci of recurrent meningioma.
An auxiliary method that allows you to determine the nature of the blood supply to the tumor is angiography. This study is often used in the process of preoperative preparation.
Make an appointment
Kinds
There are 11 types of benign meningiomas:
- meningothelial meningiomas – 60%;
- transitional meningiomas – 25%;
- fibrous meningiomas – 12%;
- rare types of meningiomas – 3%.
A brain tumor can be located in different areas of the brain:
- convexital tumor – 40%;
- parasagittal – 30%;
- basal location of the tumor – 30%.
Meningioma of the brain of the frontal lobe
Meningioma of the frontal region forms very often, in most cases it does not bother the patient for a long time. If the meningioma is located in the right frontal lobe, symptoms will appear on the opposite side of the body.
The reasons for the development of meningioma of the frontal region are various: traumatic brain injury, inflammatory disease of the meninges, genetic predisposition, food high in nitrates, neurofibromatosis and other reasons. Radiation exposure is considered a proven cause of tumor development; all other causes are considered risk factors.
Meningioma of the frontal region can cause blurred vision, headache, paresis of the facial nerves, arm muscles, lethargy and other symptoms.
Anaplastic meningioma
Anaplastic meningioma is a grade 3 brain tumor; tumor recurrence occurs in all patients within three years after treatment.
Parasagittal meningioma
Parasagittal meningioma is located in the occipital, parietal or frontal part along the longitudinal midline. Often this tumor is accompanied by a pathological increase in the content of bone matter in the bone tissue. Parasagittal meningiomas, growing in the frontal part of the head, cause:
- increased intracranial pressure;
- development of congestive optic discs in the fundus;
- severe nausea and vomiting, headache;
- epileptic seizures.
Parasagittal meningioma of the parietal region of the head is characterized by sensory disturbances and epileptic seizures. Meningioma of the occipital region is characterized by increased intracranial pressure and hallucinations.
Atypical meningioma
Atypical brain meningioma is a grade 2 tumor; tumor recurrence occurs in 30% of patients within 10 years after treatment.
Meningioma falx
A tumor growing from the greater falciform process of the brain is called falx meningioma. Over time, the tumor grows into the sagittal venous sinus, resulting in impaired venous circulation and intracranial hypertension. The growth of the tumor causes the following negative symptoms: epileptic seizures, impaired sensitivity and motor activity of the legs, pelvic disorders.
Publications in the media
Brain tumors are a heterogeneous group of neoplasms for which a common feature is location or secondary penetration into the cranial cavity. Histogenesis varies and is reflected in the WHO histological classification (see below). There are 9 main types of tumors of the central nervous system • A: neuroepithelial tumors • B: tumors of the membranes • C: tumors of the cranial and spinal nerves • D: tumors of the hematopoietic series • E: germ cell tumors • F: cysts and tumor-like formations • G: tumors of the region sella turcica • H: local spread of tumors from adjacent anatomical regions • I: Metastatic tumors.
Epidemiology. Given the heterogeneity of the concept of “brain tumor,” precise generalized statistical data are not available. It is known that central nervous system tumors in children occupy the second place among all malignant neoplasms (after leukemia) and the first place in the group of solid tumors.
Classification. The main working classification used to develop treatment tactics and determine prognosis is the WHO Classification for tumors of the central nervous system • Tumors of neuroepithelial tissue •• Astrocytic tumors: astrocytoma (fibrillary, protoplasmic, gemistocytic [mast cell], or large cell), anaplastic (malignant) astrocytoma, glioblastoma (giant cell glioblastoma and gliosarcoma), pilocytic astrocytoma, pleomorphic xanthoastrocytoma, subependymal giant cell astrocytoma (tuberous sclerosis) •• Oligodendroglial tumors (oligodendroglioma, anaplastic [malignant] oligodendroglioma) •• Ependymal tumors: ependymoma (cellular, with papillary, clear cell), anaplastic (malignant ) ependymoma, myxopapillary ependymoma, subependymoma •• Mixed gliomas: oligoastrocytoma, anaplastic (malignant) oligoastrocytoma, etc. •• Choroid plexus tumors: papilloma and choroid plexus cancer •• Neuroepithelial tumors of unknown origin: astroblastoma, polar spongioblastoma, glioma brain omatosis •• Neuronal and mixed neuronal glial tumors: gangliocytoma, dysplastic gangliocytoma of the cerebellum (Lhermitte Duclos), desmoplastic ganglioglioma in children (infantile), dysembryoplastic neuroepithelial tumor, ganglioglioma, anaplastic (malignant) ganglioglioma, central neurocytoma, paraganglioma of the filum terminale, olfactory neuroblast oma (esthesioneuroblastoma), variant : olfactory neuroepithelioma •• Parenchymal tumors of the pineal gland: pineocytoma, pineoblastoma, mixed/transitional tumors of the pineal gland •• Embryonic tumors: medulloepithelioma, neuroblastoma (option: ganglioneuroblastoma), ependymoblastoma, primitive neuroectodermal tumors (medulloblastoma [option: desmoplastic honey Ulloblastoma], medullomyoblastoma, melanin-containing medulloblastoma) • Tumors of the cranial and spinal nerves •• Schwannoma (neurilemoma, neuroma); options: cellular, plexiform, melanin-containing •• Neurofibroma (neurofibroma): limited (solitary), plexiform (mesh) •• Malignant tumor of the peripheral nerve trunk (neurogenic sarcoma, anaplastic neurofibroma, “malignant schwannoma”); variants: epithelioid, malignant tumor of the peripheral nerve trunk with divergence of mesenchymal and/or epithelial differentiation, melanin-containing • Tumors of the meninges •• Tumors of meningothelial cells: meningioma (meningothelial, fibrous [fibroblastic], transitional [mixed], psammomatous, angiomatous, microcystic, secretory, clear cell, chordoid, rich in lymphoplasmacytic cells, metaplastic), atypical meningioma, papillary meningioma, anaplastic (malignant) meningioma •• Mesenchymal non-meningothelial tumors: benign (osteochondral tumors, lipoma, fibrous histiocytoma, etc.) and malignant (heme angiopericytoma, chondrosarcoma [ option: mesenchymal chondrosarcoma] malignant fibrous histiocytoma, rhabdomyosarcoma, meningeal sarcomatosis, etc.) tumors •• Primary melanocytic lesions: diffuse melanosis, melanocytoma, malignant melanoma (option: meningeal melanomatosis) •• Tumors of unknown histogenesis: hemangioblastoma ( capillary hemangioblastoma) • Lymphomas and tumors of hematopoietic tissue •• Malignant lymphomas •• Plasmacytoma •• Granulocellular sarcoma •• Others • Tumors of germ cells (germ cell) •• Germinoma •• Embryonic carcinoma •• Yolk sac tumor (endodermal sinus tumor) •• Choriocarcinoma •• Teratoma: immature, mature, teratoma with malignancy •• Mixed germ cell tumors • Cysts and tumor-like lesions •• Rathke's pouch cyst •• Epidermoid cyst •• Dermoid cyst •• Colloid cyst of the third ventricle •• Enterogenous cyst •• Neuroglial cyst •• Granular cell tumor ( choristoma, pituicytoma) •• Neuronal hamartoma of the hypothalamus •• Nasal glial heterotopia •• Plasmacytic granuloma • Tumors of the sella turcica •• Pituitary adenoma •• Pituitary cancer •• Craniopharyngioma: adamantinoma-like, papillary • Tumors growing into the cranial cavity •• Paraganglioma (chemodectoma) •• Chordoma •• Chondroma •• Chondrosarcoma •• Cancer • Metastatic tumors • Unclassified tumors
Clinical picture. The most common symptoms of brain tumors are progressive neurological deficit (68%), headaches (50%), and seizures (26%). The clinical picture mainly depends on the location of the tumor and, to a lesser extent, on its histological characteristics • Supratentorial hemispheric tumors •• Signs of increased ICP due to mass effect and edema (headaches, congestive optic discs, disturbances of consciousness) •• Epileptiform seizures • • Focal neurological deficit (depending on location) •• Personality changes (most typical for frontal lobe tumors) • Midline supratentorial tumors •• Hydrocephalic syndrome (headache, nausea/vomiting, disturbances of consciousness, Parinaud's syndrome, congestive optic discs) •• Diencephalic disorders (obesity/emaciation, thermoregulation disorders, diabetes insipidus) •• Visual and endocrine disorders in tumors of the chiasmatic-sellar region • Subtentorial tumors •• Hydrocephalic syndrome (headache, nausea/vomiting, disturbances of consciousness, congestive optic discs) •• Cerebellar disorders •• Diplopia, severe nystagmus, dizziness •• Isolated vomiting as a sign of an effect on the medulla oblongata • Tumors of the base of the skull •• Often asymptomatic for a long time and only in the later stages cause neuropathy of the cranial nerves, conduction disorders (hemiparesis, hemihypesthesia) and hydrocephalus.
Diagnostics. Using CT and/or MRI at the preoperative stage, it is possible to confirm the diagnosis of a brain tumor, its exact location and extent, as well as the presumptive histological structure. For tumors of the posterior cranial fossa and skull base, MRI is more preferable due to the absence of artifacts from the bones of the base (the so-called beam-hardering artifacts). Angiography (both direct and MR and CT angiography) is performed in rare cases to clarify the characteristics of the blood supply to the tumor.
Treatment . The treatment strategy depends on the exact histological diagnosis, the following options are possible: • observation • surgical resection • resection in combination with radiation and/or chemotherapy • biopsy (usually stereotactic) in combination with radiation and/or chemotherapy • biopsy and observation • radiation and/or chemotherapy without tissue verification based on CT/MRI results and tumor marker studies.
The prognosis depends mainly on the histological structure of the tumor. Without exception, all patients operated on for brain tumors require regular MRI/CT control studies due to the risk of relapse or continued tumor growth (even in cases of radically removed benign tumors).
ICD-10 • C71 Malignant neoplasm of the brain • D33 Benign neoplasm of the brain and other parts of the central nervous system
Treatment
Meningioma very often causes the development of edema of surrounding tissues, which affects the appearance of various negative symptoms. Steroid drugs are prescribed to relieve swelling. Treatment for meningioma depends on the type and size of the tumor, its location, the patient's health and age.
According to medical statistics, in 90% of cases, brain meningiomas are benign tumors, which are characterized by slow development and the absence of concomitant damage to vital organs.
Malignant tumors are characterized by rapid growth and the presence of metastases in any other organs of the human body.
Tumor removal
Removal of meningioma is not always carried out. Most often, a benign tumor is monitored. Surgery is required if the meningioma is malignant and increases in size.
The main treatment method for growing benign and malignant tumors is surgery to remove brain meningioma. It is very important to perform competent removal of the tumor. The consequences of incorrect surgical intervention, which damaged the surrounding brain tissue or venous sinuses, can be very dire. Such an operation can cause a significant decrease in the patient’s quality of life, so neurosurgeons often leave part of the cancerous tissue, constantly monitoring its growth.
Malignant meningiomas tend to recur, requiring repeated surgery.
Make an appointment
Consequences of the operation
Depending on the location of the tumor and its size, complications may develop after the operation: deterioration or loss of vision, partial or complete memory loss, paresis of the limbs, impaired concentration, changes in character, personality, cerebral edema, bleeding.
Radiation therapy
Treatment of brain meningioma without surgery involves the use of radiation therapy methods, which are used when it is not possible to effectively remove the tumor surgically. Pathological cells are destroyed under the influence of high doses of X-ray radiation. The use of standard radiation therapy is inappropriate for the treatment of patients diagnosed with large cerebral meningioma. However, treatment without surgery in such cases is ineffective.
When the tumor is localized in a place that is difficult for a neurosurgeon to reach, or when there are areas close to it, damage to which can lead to disruption of vital functions, specialists at the Yusupov Hospital give preference to stereotactic methods. This type of therapy can be used to treat large tumors. Stereotactic radiosurgery is based on targeted irradiation of a tumor formation with beams located at different angles.
Often, the stereotactic method is combined with surgical treatment - if there are contraindications for removing tumors in the usual way.
Chemotherapy is not used to treat benign brain meningiomas.
Classification of oligodendrogliomas
There are three types of oligodendroglioma, depending on their aggressiveness and behavior.
Oligodendroglioma grade 2
This is a typical oligodendroglioma of the brain. It is characterized by slow growth, low aggressiveness and mitotic activity of cells. How long people live after surgery to remove a tumor is an individual question. In this case, the prognosis is usually favorable than when diagnosing other types of tumors.
Note. Stage 2 brain oligodendroglioma is diagnosed more often than other tumors of this type.
Anaplastic oligodendroglioma grade 3
Anaplastic oligodendroglioma is characterized by high aggressiveness. Neoplasia is characterized by rapid cell growth and its spread to neighboring tissues. It is a fairly rare type of neoplasm. They account for about one percent of all malignant neoplasms in the brain.
Most often, anaplastic oligodendroglioma forms in the frontal lobe of the brain; somewhat less frequently, the tumor forms in the temporal region. Clinical signs are similar to other neoplasms of this genus, but for anaplastic oligodendroglioma the main distinguishing feature is the formation of convulsive or nervous seizures, which is typical both for the primary tumor and for relapses that malignize into anaplastic glioma, a more dangerous type of cancer.
The note. Anaplastic oligodendroglioma is more common in adults.
The histological feature of anaplastic oligodendroglioma is that pathogenic cells are characterized by a high level of mitotic activity. In this case, cellular atypia is noted. In rare cases, necrosis develops; small blood vessels can grow strongly in the tumor.
Anaplastic oligodendroglioma is characterized by the presence of pathological reactive astrocytes. This feature can complicate diagnosis, because even experienced clinicians sometimes have certain difficulties in differentiating oligodendroglioma and glioblastoma with oligodendroglial elements.
Treatment of anaplastic oligodendroglioma is only radical, followed by radiation and chemotherapy. It is important to remove the entire oligodendroglioma, or if this is not possible, then most of it.
Oligoastrocytoma of the brain
Brain oligoastrocytoma is a mixed type tumor. It is classified as the third degree of malignancy. A characteristic feature of brain oligoastrocytoma is that it can degenerate into glioblastoma, a dangerous type of cancer. Oligoastrocytoma is characterized by rapid growth, damage to nearby brain tissue and metastases. This poses a real threat to life, so the survival rate in this case is low (stages 3 and 4 of carcinogenesis/grade).
Note. There is no first-grade oligodendroglioma.
Relapses
If a benign, clearly circumscribed meningioma that has not grown into the surrounding tissue is detected in a patient, surgical intervention most often ensures a complete recovery.
However, it must be remembered that after removal of even benign meningiomas, relapses can occur. Recurrences of atypical meningiomas are recorded in almost 40% of cases, of malignant ones - in 80%.
The development of relapses within five years after surgery also depends on the location of the tumor.
Relapses are least likely to occur with meningioma localized in the cranial vault, more often in the area of the sella turcica and the body of the sphenoid bone. The most common tumors that recur are those affecting the sphenoid bone and cavernous sinus.
Life prognosis after surgery
Patient survival depends on the effectiveness of treatment, stage, presence of metastases and relapses. The location of the tumor is of no small importance. The sooner a pathological neoplasm is identified and surgical treatment is performed, the better the prognosis.
With the classic type of tumor of the 2nd degree of malignancy in patients under 40 years of age after surgery and complex treatment, the prognosis is favorable: the average period without relapse is 5 years, and the ten-year survival rate remains at 35%. About 30% of patients will survive more than 5 years after the initial diagnosis. The prognosis worsens in proportion to the worsening degree of malignancy.