The pituitary gland is an endocrine gland located in the sella turcica (a formation in the human skull). Despite its miniature size, it controls many functions in the body. It is the pituitary gland that produces hormones that are responsible for the functioning of the entire endocrine system. Nature has reliably protected this gland from external influences, but internal factors can still cause pathological changes. One such problem is pituitary adenoma. It can be recognized by hair loss, infertility, changes in appearance, sexual dysfunction and many other signs.
Types of pituitary adenoma
There are various criteria for classifying benign pituitary tumors.
To size:
- microadenoma – tumor size up to 10 mm;
- mesoadenoma - a tumor measuring from 10 mm to 20 mm, located within the sella turcica;
- macroadenoma - a tumor measuring from 10 mm to 30 mm, or extending beyond the boundaries of the sella turcica;
- giant adenoma – a tumor larger than 30 mm.
In a simplified classification, meso- and giant adenomas are classified as medium and giant macroadenomas, respectively.
By nature of distribution:
- endosellar (intrasellar) – the tumor does not extend beyond the boundaries of the sella turcica;
- endosuprasellar - the adenoma grows upward beyond the sella turcica towards the optic chiasm;
- endolaterosellar - spread of the neoplasm into the cavernous sinuses by germination of the lateral wall of the sella turcica;
- endoinfrasellar – pituitary adenoma grows downwards from the sella turcica.
A tumor growing in different directions is called endo-supra-infra-laterosellar.
By origin:
- primary tumors;
- secondary, developed as a result of hypofunction of peripheral endocrine glands;
- adenomas caused by disruption of the hypothalamus, as well as the production of releasing hormones in ectopic formations located in non-endocrine organs.
Based on hormonal activity, pituitary adenomas are divided into active (about 60% of adenomas) and inactive (about 40%). Hormonally active tumors, based on the type of hormones they produce, are divided into:
- somatotropinomas;
- corticotropinomas;
- thyrotropinomas;
- prolactinomas.
Gonadotropinomas are also isolated, which most often do not affect hormonal levels, since they produce biologically inactive hormones. However, sometimes these tumors produce active forms of follicle-stimulating hormone and luteinizing hormone.
There are mixed tumors that produce more than one type of hormones.
The danger of education
Since microadenoma of the pituitary gland of the brain increases the production of various hormones, this is fraught with endocrine disorders and metabolic problems. Prolonged presence of a tumor in the head leads to the leaching of minerals from the bones, including calcium. Osteoporosis, increased fragility and other pathologies develop.
Due to malfunctions in the thyroid gland and increased production of prolactin, women experience infertility. When asked whether a pituitary adenoma can resolve on its own, doctors most often give a negative answer.
A tumor of any type can grow, and this is the main reason why pituitary microadenoma is dangerous.
Constant growth leads to compression of the optic nerves and headaches. If the hypothalamus is involved in the process, the patient experiences disturbances of consciousness, and migraine of the frontal or temporal region very often develops. Even a small-sized pituitary microadenoma can develop into an adenoma with a malignant course. If detected in a timely manner, restraining medications are prescribed. Other features of different shapes:
- endosellar pathology is characterized by accelerated growth, which leads to significant disruptions in brain function;
- cystic pathology often degenerates, has hard edges that strongly affect the work of other nearby glands and tissues;
- with any microadenoma of the pituitary gland, women are faced with the fact that in 98% of cases they cannot become pregnant;
- even if conception has occurred, the pregnancy almost always ends in miscarriage due to disruption of the smooth muscles of the body.
If a woman manages to carry a fetus to term, immediately after childbirth the increased prolactin level begins to decrease.
Causes of pathology
The reasons for the development of pituitary adenoma are factors that directly affect the brain and the gland itself (trauma, neuroinfections), as well as those that have an indirect effect due to the pathology of other glands and organs. The latter include disorders of the regulatory function of the hypothalamus, thyroid gland, gonads, as well as the appearance in organs that are not endocrine glands of areas that produce hormones (for example, such accumulations of cells are found in small cell lung cancer).
In hereditary forms of the disease, mutations in suppressor genes that suppress the process of tumor cell changes play a role in the occurrence of tumors. The causes of the mutation are unknownSource: Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59.
What it is
The pituitary gland is also called the pituitary gland, which is located on the lower surface of the brain. The mass of the gland is only 1 g. Not only the functioning of the internal organs, but also the appearance of a person depends on its work.
It is she who ensures the development of universal human external characteristics. Therefore, deviations in its work will be very noticeable.
Symptoms of pituitary cancer
A pituitary tumor is a common brain disease that affects the endocrine system and has specific symptoms.
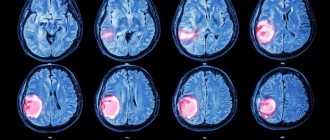
To examine the pituitary gland, an MRI is performed, which determines the homogeneity of the tissue, that is, the ability to equally reflect rays.
By homogeneity we mean:
- absence of pathological shadows;
- maintaining normal sizes ;
- smooth borders with smooth curves;
- no signs of infiltration;
- position of the organ relative to other tissues.
If there is a discrepancy with even one point, we can talk about the diagnosis of diffuse heterogeneity of the pituitary gland.
Symptoms of pituitary adenoma
Clinical manifestations of the disease can be divided into two groups. With microadenomas or small endosellar tumors, endocrine symptoms come to the fore, varying depending on the hormones secreted.
With large hormonally inactive adenomas spreading beyond the sella turcica, neuro-ophthalmological symptoms prevail, which are different for tumors growing in different directions.
Endocrine symptoms
Somatotropinoma
A tumor that produces somatotropin, or growth hormone. Its manifestations depend on the period of tumor onset. Before the growth of bone tissue is complete (in adolescence and young adulthood), it manifests itself as symptoms of gigantism; in adults, acromegaly.
Gigantism is a proportional increase in bone length and overall height. Women can reach a height of 190 cm, men - over 2 meters.
Acromegaly is characterized by pathological growth of bones, soft tissues, cartilage, and corresponding changes in appearance - the nose, lips, chin, brow ridges, hands, feet increase disproportionately to the rest of the body. Patients experience hyperhidrosis (excessive sweating), hirsutism (excessive hair growth), severe sebum production, and the appearance of papillomas, warts, and nevi on the skin.
In addition, the patient’s internal organs become enlarged, and metabolic and endocrine processes are disrupted. From the cardiovascular system, increased blood pressure, cardiomyopathy, and cerebrovascular accidents are observed. From the nervous system - polyneuropathy, manifested by pain, paresthesia, decreased sensitivity of the peripheral parts of the extremities. The development of obesity, secondary diabetes mellitus, and thyroid pathologies is possible. Source: Main types of complications with pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92.
Corticotropinoma
A pituitary adenoma that produces ACTH is an adenocorticotropic hormone, an excess of which develops Cushing's disease. Its symptoms:
- Cushingoid obesity - an increase in the volume of adipose tissue on the face, back, hips and buttocks, and abdomen;
- swelling and congestion of the face;
- striae - stretch marks of purple-violet color on the skin of the abdomen and thighs;
- skin atrophy, especially on the back of the hands, pustular diseases, fungal infections;
- osteoporosis accompanied by multiple compression fractures;
- arterial hypertension, cardiovascular failure;
- secondary diabetes mellitus.
Thyrotropinoma
A neoplasm that produces thyroid-stimulating hormone. Thyrotropinoma can be primary or secondary.
Primary thyrotropinoma has characteristic signs of thyrotoxicosis (excess thyroid secretion). Its symptoms:
- cardiopalmus;
- tremor - trembling throughout the body, shaking fingers;
- hyperhidrosis;
- nervousness;
- bad dream.
Secondary thyrotropinoma develops as a result of a long course of uncompensated hypothyroidism. It is characterized by:
- weakness, lethargy;
- body swelling and weight gain;
- lethargy, absent-mindedness, memory impairment;
- slow metabolism.
Prolactinoma
One of the most common gland tumors. It arises from cells that synthesize the hormone prolactin. The symptoms of this pituitary adenoma are different in women and men. Source: Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L., Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80.
Among women:
- decreased sexual desire up to frigidity;
- menstrual irregularities;
- discharge from the nipples outside the period of breastfeeding;
- infertility.
For men:
- gynecomastia – enlargement of the mammary glands;
- hypoplasia of secondary sexual characteristics;
- decreased libido, erectile dysfunction;
- infertility.
Gonadotropinomas
Most often hormonally inactive, they can rarely produce active forms of follicle-stimulating or luteinizing hormones, causing ovarian hyperstimulation syndrome in women.
Neuro-ophthalmological signs
With endosuprasellar adenoma, partial loss of visual fields is observed while maintaining visual acuity. An increase in tumor size leads to gradual atrophy of the optic nerves and blindness.
A tumor growing to the sides causes impaired oculomotor function (ophthalmoplegia) and double vision (diplopia), and decreased visual acuity.
When an adenoma grows into the bottom of the sella turcica, patients note nasal congestion, simulating the clinical picture of sinusitis or nasal tumors.
If the tumor grows towards the hypothalamus, patients complain of sleep disturbances, uncontrolled appetite, unstable thermoregulation (fever, chills), emotional disturbances: unstable mood, tearfulness, irritability.
With a large adenoma and its multidirectional growth, the symptoms will overlap each other and be masked. The following neurological manifestations are possible:
- headache, dizziness;
- nausea, vomiting;
- speech and facial expression disorders;
- dysphagia is a swallowing disorder.
Diagnosis of the disease
Patients with suspected pituitary adenoma complain to various doctors: a neurologist, ophthalmologist or endocrinologist.
At the initial appointment, the doctor will conduct a general examination, collect an anamnesis of life and illness, prescribe laboratory and instrumental tests: general blood and urine tests, blood biochemistry, ECG. A doctor of appropriate specialization will conduct an ophthalmoscopy, test visual acuity, neurological examination, and evaluate the existing symptoms.
In addition, the following studies are indicated for patients with pituitary adenoma:
- radiography of the skull;
- CT, MRI of the brain;
- Ultrasound of the thyroid gland, heart, liver, spleen;
- analysis of hormone levels in blood and saliva.
If surgical intervention is indicated, the patient must consult a neurosurgeon.
Healing procedures
At the first symptoms of pituitary adenoma, treatment is prescribed with an ergot-based drug, bromocriptine.
In the fight against other types of small adenomas, radiation therapy in the form of gamma or proton therapy is more often used, and sometimes radioactive substances are injected directly into the tumor.
For larger adenomas or certain complications (hemorrhages, cysts, visual impairment), surgery .
In the case of macroadenomas craniotomy ; for smaller sizes, transnasal surgery .
Treatment of the disease
According to clinical guidelines, there are three main approaches to the treatment of pituitary adenoma:
- conservative (medicines);
- radiation therapy;
- neurosurgical.
The drug method is indicated for small prolactin-producing adenomas. Treatment is carried out with prolactin antagonist drugs.
Radiation therapy is carried out in various ways: gamma, proton, external beam radiation therapy, stereotactic radiosurgery.
For somatotropinomas and corticotropinomas, neurosurgical removal is used. Before surgery, hormonal therapy is often prescribed to reduce the effect of hormone hypersecretion, which sometimes leads to a reduction in the size of the tumor. Drug and radiation therapy are also prescribed after surgery according to indications.
Neurosurgical intervention is recommended for macroadenomas that have severe symptoms and a risk of complications - visual impairment, up to complete blindness, hemorrhage, brain cysts. Source: Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50.
Forecast
The prognosis for life with damage to the pituitary gland is more than favorable. The sooner you notice the symptoms of tumor growth, the higher the likelihood of a complete recovery. The prognosis also depends on the treatment method. Of course, if the tumor has progressed intensively and led to partial or complete loss of vision, then it will not be possible to normalize it.
If you follow all the doctor’s recommendations, you can quickly restore hormonal levels with minimal risk of relapse.
Prognosis and rehabilitation
With timely diagnosis and proper treatment, pituitary adenoma has a generally favorable prognosis without undesirable consequences. Remission after removal of an adenoma occurs in 70-80% of cases, this figure is higher for microcorticotropins and lower for somatotropins and prolactin. The relapse rate is about 12%. Postoperative mortality is low - approximately 4%, decreasing to almost 0 for endosellar and endosuprasellar tumors. The risk of mortality is higher with a large adenoma, its penetration into the ventricular system, or tumor growth of blood vessels.
Rehabilitation, as a rule, does not take much time, since most pituitary adenomas are removed transnasally (through the nose) using endoscopic instruments. In the early postoperative period, the patient is prescribed painkillers, hemostatic agents, and antibiotic therapy. If there are no complications, after a few days the patient is discharged home and is under the supervision of a doctor (ENT, ophthalmologist, endocrinologist) in the clinic. No special rehabilitation measures are required.
Prevention
There is no specific prevention of pituitary adenoma, since the exact causes of tumor development are unknown. If suspicious symptoms appear, you should immediately consult a doctor. Timely diagnosis and treatment will help achieve the most favorable results and maintain the patient’s quality of life.
Sources:
- The main types of complications from pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92
- Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59
- Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L.,
- Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80
- Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50
Useful video
Watch the video about the prevention of diseases of the pituitary gland and adrenal glands:
Similar articles
- MRI of the pituitary gland: how to do it without contrast and with it, what...
For a detailed examination, an MRI of the pituitary gland is prescribed. It is performed with and without contrast. Almost no preparation is needed. What does an MRI show? What is the pituitary gland normal when a tumor is suspected? Read more - Enlarged pituitary gland: main causes, symptoms...
There are many factors that can cause the pituitary gland to become enlarged. The main reasons include hormonal fluctuations, as well as sinusitis and rhinitis. Symptoms depend on the size; they may not be present at all. Signs of changes in vertical size are visible on x-rays. The consequences without treatment are severe, including blindness and development into an adenoma. Read more
- Rathke's cyst of the pituitary gland: how the formation manifests itself...
Sometimes a Rathke cyst of the pituitary gland does not make itself felt; in other cases, the formation of a pocket leads to high blood pressure and hormonal imbalances. Treatment is prescribed only in case of abnormalities or large size of the Rathke cyst. Read more
- Hemorrhages in the pituitary gland: main symptoms, MRI with...
Often, hemorrhage into the pituitary gland occurs with adenoma and microadenoma. Unfortunately, the symptoms are similar to a heart attack or stroke, and it is not always possible to diagnose it in a timely manner. For an accurate determination, CT and MRI are used. Read more
- Hormones of the pituitary lobes: anterior, middle, posterior, their...
Hormones of the pituitary gland influence almost all vital functions of the body. The structural features of the organ include three lobes - anterior, middle and posterior. What are their functions? What is the histological and physiological significance? Read more