Metastasis is the migration of carcinogenic cells from the primary tumor to other organs, which is typical for most cancer tumors. This leads to the formation of secondary lesions in other tissues. Different types of cancer are characterized by different intensity of the metastatic process, which depends on the degree of malignancy and characteristics of the primary tumor. The more intense the spread, the more aggressive the cancer. For example, with skin melanoma, metastases to the brain occur frequently, unlike basal cell carcinoma. The metastatic process begins, as a rule, at the third stage of carcinogenesis, and at the fourth stage it already manifests itself quite strongly. There are two ways for cancer cells to migrate: through the blood and lymph. The appearance of metastatic tumors will be identical to the appearance of the cells of the primary tumor. When neoplasias are detected in the brain, it is important to ensure that these are secondary tumors. For this purpose, a complete examination of the body is carried out. In the presence of metastases in the brain, the prognosis worsens, life expectancy is estimated at months, in some cases weeks.
Metastasis formation
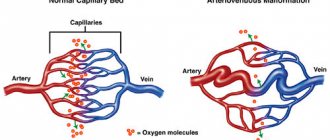
Metastases form after the development of a primary malignant neoplasm in other organs. The latter are formed as a result of mutagenesis or errors in the genetic material of somatic cells. At the initial stages, there is no metastatic process, but as it progresses, the tissues of the primary tumor grow into nearby organs. In the future, the disease worsens, cancer cells begin to break away from the primary focus and migrate through the blood or lymphatic channels (the integrity of the blood vessels is damaged). A metastatic cell attaches itself to an organ, germinates, and gives rise to a new lesion—a secondary tumor.
Important. In different individuals, the nature, timing and intensity of the formation of secondary metastatic foci are different, which is explained by the level of antitumor immunity.
Features of metastasis
The intensity of the metastatic process, the degree of malignancy, the formation of relapses, the treatment of brain metastases and the aggressiveness of cancer are influenced by the following circumstances:
- Stage of carcinogenesis. The life prognosis directly depends on the stage at which the cancer was discovered and surgically removed. The most successful will be removal of cancer at the first stage, however, this cannot guarantee a complete cure, so the patient must be constantly monitored.
- The location of the primary tumor largely determines the nature of the metastatic behavior of cancer and damage to other organs.
- The histological structure and form of cancer also influence the reasons for the spread of metastases. The most dangerous are poorly differentiated forms. Different types of carcinogenesis are characterized by different features of cancer cell migration. If the tumor is dense and slowly growing, for example, cylindroma, then metastases to the brain are rare and, as a rule, only in the terminal stages. In other cases, even with good antitumor immunity, metastases form in the brain, for example, with the development of melanoma.
- Features of anticancer therapy. If it is possible to completely remove the primary tumor in the initial stages, with the administration of radiotherapy and chemotherapy, then in this case the treatment gives the most acceptable result.
- The older the patient, the more difficult the cancer is to treat.
Causes of the disease
Once detached from a cancerous tumor, cells are able to travel considerable distances through the blood and lymph. They even affect distant organs and invade healthy cells. After the cell has established itself in a new place for it, the process of uncontrolled division begins.
In addition to moving through the blood and lymph, the spread of cancer cells in the peritoneal cavity occurs transcoelomically. This happens, apparently, because the conditions are favorable for them. A significant part of metastases are localized in areas where there is a weak rhythmic contraction of the walls of organs or where excessive absorption of intra-abdominal fluid occurs.
Often, the spread of cells is lower during surgery and laparoscopy than during classical surgery. Surgical manipulation involves preventing the spread of the tumor process throughout the body through the use of unique treatment solutions. The most effective method of purification is HIPEC, which involves intracavitary chemotherapy in combination with hyperthermia.
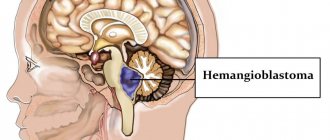
Metastases to the brain
Lead to the formation of secondary tumors in various parts of the brain. This almost always causes death. In general, any type of cancer can lead to this, but there are tumors that metastasize more often than other types of cancer:
- Metastases to the brain in skin cancer (melanoma) are more common than in other types. Approximately 50-73% of patients face this problem. In 10-45% of cases (at the time of diagnosis), melanoma is at stage 4, when there are already metastatic lesions. At the same time, every third patient exhibits neurological manifestations. In this case, a condition similar to a stroke often develops, because a hemorrhage forms in the pathological neoplasm. Treatment of brain metastases in melanoma is complicated by the fact that they are poorly sensitive to radiotherapy.
- Metastases in lung cancer form in 35-60% of cases. In this case, how long people live with brain metastases is determined by many factors (age, type of cancer, intensity of carcinogenesis, presence of metastatic lesions in other organs, and so on). According to statistics, such metastases in lung cancer are the most dangerous in terms of mortality. Most often they are characteristic of the fourth stage of pathogenesis. Only in 5% of cases will the patient live 2-3 years. As a rule, at this time there are already multiple neoplasms in the lymph nodes and other organs. The patient receives palliative treatment.
- In breast cancer in women, metastases to the brain are recorded in 20-30% of cases. At later stages, metastases are diagnosed in the brain and many other organs. Treatment is carried out with radiochemotherapy and hormone therapy. The quality of life deteriorates significantly, stroke, mental disorders, vertebral fractures due to brittle bones, cough due to lung damage, and so on are possible.
- Brain metastases in kidney cancer are characteristic of stage 4. In this case, there are secondary lesions in other organs (second kidney, lungs, other organs and multiple lymph nodes). The prognosis is unfavorable: only 8% of patients will live for about two years. Kidney cancer has a high risk of recurrence.
- Metastases from bladder cancer can be at the fourth stage. The prognosis is negative due to the presence of secondary tumors in other organs; most patients will not live more than a year. Removing the cancer is almost impossible; supportive treatment is prescribed.
- Brain metastases in intestinal and esophageal cancer are observed at stage 4. If they are present in other organs, the prognosis is negative - only 6% of patients will live more than a year.
In addition to these types of cancer, metastatic brain lesions can also form in other malignant neoplasms, for example, in the terminal stages of laryngeal or thyroid cancer, when the tumor grows into large main arteries.
Classifications
There is no single classification. This is due to the fact that the primary cancer sites that lead to the appearance of the disease are different in their characteristics. One of the most common gradations of abdominal carcinomatosis is the one based on the number of metastases and their location. This classification distinguishes 3 degrees of the disease:
- P1 – local damage to the abdominal cavity;
- P2 – several foci of the disease were identified, which were separated by healthy areas of the abdominal cavity;
- P3 – there are many lesions in the abdominal cavity.
The method for determining the abdominal cavity carcinomatosis index is also applicable, during which the sum of points (from 0 to 3) is calculated for measuring the foci of maximum damage in each of the most likely areas of damage to the peritoneal cavity.
Symptoms and signs
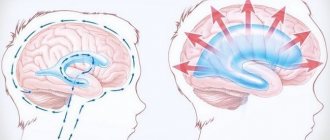
As cancer progresses, it enters later stages (3 and 4). In this case, metastases form in the brain, so characteristic clinical signs begin to appear. Manifestations will depend on the area of the brain affected. In many cases, the signs are mirrored, i.e. if the tumor is in the right hemisphere, then the clinic will appear on the left side and vice versa.
Main features:
- dizziness, headache due to increased pressure inside the skull, while negative symptoms are not relieved by medications;
- dyspeptic symptoms, nausea and vomiting (vomiting does not bring relief), which is not associated with poisoning;
- various disorders of brain activity: confusion, memory impairment, speech impairment, epileptic seizures, hallucinations, etc.;
- vision, hearing, and smell suffer;
- the mental and emotional background changes, the person becomes rude, aggressive, overly irritable;
- the formation of epileptiform seizures with brain damage is more typical for the elderly;
- motor activity is impaired, coordination and fine motor skills suffer, it is difficult for the patient to maintain balance, gait is impaired, the ability to write, and so on.
Symptomatic manifestations
Peritoneal pathology in the first stages of its development may not reveal itself, especially when there is no excess liquid mass in the peritoneal cavity.
In this case, the liquid mass can accumulate without the participation of metastases. Symptomatic manifestations of the disease in most cases are nonspecific, however, as a rule, they are noted:
- Discomfort in the abdomen;
- Severe weakness;
- Unexplained weight loss;
- Weight loss with a stable diet regimen;
- Loss of appetite;
- Malfunction of the gastrointestinal tract.
As the disease progresses, malignant cells lead to:
- Poisoning of the body;
- Compression of the stomach by a tumor;
- State of nausea, vomiting;
- Stool disorders;
- Raising body temperature above normal.
The resulting ascites negatively affects the breathing process, which leads to heart failure, persistent edema, and protein deficiency due to frequent evacuation of liquid mass.
Diagnostics
Since the formation of secondary tumors in the brain causes the death of the patient, it is important to identify the presence of a pathological formation as early as possible. If cancer is present, the patient must be diagnosed continuously to monitor the situation and timely identify secondary tumors in the brain. If the tumor in the head is small, it usually already has a pronounced clinical picture, however, it can be diagnosed at the earliest stages using computed tomography (CT) or magnetic resonance imaging (MRI). A biopsy is important to establish the metastatic process and clarify all the nuances of pathogenesis. The presence of metastases can be suspected even with a biochemical blood test.
What happens during radiation therapy?
Before starting radiation therapy, the patient is consulted by a radiation oncologist. During the consultation, the doctor evaluates the medical history and conducts an examination. In addition, consultations are carried out with other specialists who are part of the group of treating personnel.
Once the most suitable treatment method has been selected, the radiotherapy planning phase begins. At this stage, a radiation oncologist who specializes in radiation therapy for malignant tumors conducts treatment simulation. This uses standard radiography or CT, and in some cases MRI. The results of the examination are important for choosing the type and direction of the beam of rays.
It is important to remain still during simulated radiotherapy, although no radiation treatment is given during this period. A fixation mask is used to hold the patient's head in a certain position. As a rule, radiation therapy begins 1-2 days after drawing up a treatment plan.
During each radiation therapy session, the patient lies motionless on the treatment table while the radiologist or technician administers the treatment according to parameters prescribed by the oncologist. A radiotherapy session takes only a few minutes and is completely painless.
During stereotactic radiosurgery, a rigid head frame is used to immobilize the patient. In addition, during the procedure, regular scans (CT or MRI) are performed, which allows you to accurately monitor the position of the tumor and adjust the radiation dose if necessary.
Treatment planning and the first radiotherapy sessions take 1 or 2 hours. After this, each session lasts only a few minutes, and the patient's total stay in the radiology department does not exceed 30-45 minutes. As a rule, radiotherapy is carried out 1-2 times a day, 5 days a week, for 5-7 weeks.
Up
Treatment
What to do in case of metastases in the brain is decided by a council of doctors based on the diagnosis and medical history of the patient. Treatment of metastases in the head is very difficult, which is due to the inaccessibility of the location of secondary lesions in the brain, the presence of multiple tumors in other organs, the patient’s condition in the later stages, age and a number of other factors. Today, in the presence of secondary tumors in the head, stereotactic radiosurgical techniques are used, which stop or slow down the growth of pathological tissue. The best result is achieved when tumors are removed surgically, but at these stages treatment is always difficult. The method of treatment will depend on the location of the tumor, the intensity of damage to other organs and the general condition of the patient.
Main types of treatment
- Surgical treatment is possible only in cases where there is access to tumors in the brain. As a rule, in the terminal stages many other organs are already affected, so surgical treatment is carried out mainly for palliative purposes, to eliminate negative signs and alleviate the patient’s condition. In some cases, it is possible to remove a few tumors or metastases are removed en bloc (when they are located nearby). If there are many lesions in the brain, then surgical treatment is not advisable.
- Treatment with radiotherapy is more preferable in this case. For deep, hard-to-reach locations of secondary tumors in the brain, this type of treatment is the main one. For a few tumors, stereotactic proton therapy (irradiation of an organ from several sides) will be an effective method.
- Chemotherapy and drug treatment for brain metastases are not effective. Drugs are prescribed to relieve negative symptoms and reduce side effects. Thus, drug therapy is palliative.
Best practices
Clinical practice shows that the greatest positive effect is achieved by a combination of 3 treatment methods:
- Cytoreduction is an intervention during which a maximum of cancerous tumors are removed;
- Local hyperthermia;
- Introduction of chemicals into the cavity.
If intraperitoneal hyperthermic chemotherapy (IHC or HIPEC) is used during surgery, it is possible to maintain a significant concentration of the drug in the area of the tumor for a long time and thereby ensure a high medicinal effect. The prospects for such treatment are encouraging.
Intraoperative photodynamic therapy (PDT), with its effect on the tumor with a photosensitizer, is inferior to HIPEC in terms of positive results. This is explained by the fact that the laser does not penetrate all areas of the peritoneum. However, for tumors that are large in volume or tumors that are few in number, this method has proven itself to be excellent.