Mnestic activity is the ability of the brain to record, remember any information, and reproduce it at the right time. The human brain has a well-developed ability to reproduce facts and events accurately.
But some people experience mental disorders. Why this happens and how to correct them will be discussed in the article.
Mnestic activity of man. Peculiarities
Mnestic activity is the work of the cerebral cortex aimed at the perception, systematization and sequential reproduction of information. Only humans have the ability to remember information that is not related to the direct perception of the world through the senses. However, it is feelings that are associated with attention.
The human brain constantly perceives and analyzes the incoming stream of signals. But as conscious beings, we can selectively fix our attention on the necessary areas of knowledge and remember abstract statements that do not have visual properties.
Forgetfulness does not always indicate mental disorders
As efficient as the human brain is at processing information, it can also make choices: information that is not requested regularly and therefore seems redundant in the long term disappears again from memory. Another characteristic of mnestic mechanisms is that people remember positive things better and longer than negative experiences.
Only what the brain perceives very impressively - especially when it is associated with strong emotions - or what it needs and is repeated over and over again, is retained for years. The fact that individual information is lost through selection or suppressed by others does not necessarily indicate memory impairment. However, certain manifestations of memory impairment and memory loss are diseases that should be treated if necessary.
Elementary and specific mnestic processes
In neuroscience, it is customary to distinguish between elementary and specific mnestic processes. Elementary ones (sensitization, conditioned reflex) are present even in primitive animals. Specific ones are inherent in more advanced, multilayer types of memory.
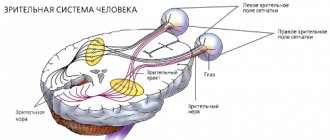
Modal-specific mnestic processes are those that are associated with the functioning of various sensory systems. Based on this, the corresponding types of memory are distinguished: visual, auditory, tactile, olfactory, motor. A modality-specific type of memory often becomes necessary in professional activities (auditory memory of people involved in music).
Processes of mnestic activity. Stages
The memorization process sequentially goes through several stages.
- Recognition of the material. It takes careful reading or listening to the material to leave some kind of trace in the brain.
- Then this trace must be fixed through volitional efforts.
- Systematization, when new knowledge is superimposed on existing knowledge in different brain structures and assimilated. At the same time, those blocks that do not correspond to previously learned material and marked as important, that knowledge is erased. This is necessary to ensure that internal “failures” do not occur in the playback system.
- Playback. The material that has been successfully integrated into the overall picture of the world built by the brain is securely stored in long-term memory.
It takes quite a lot of time to process new information. Few people have phenomenal mnestic abilities to quickly grasp and remember something forever. The brain also spends an incredible amount of energy.
The peculiarity of mnestic activity is that the perception mechanism is always at work. But for new neural connections to form, the body must have enough protein and neurotransmitters: dopamine, serotonin. In addition, you need at least 8 hours of sleep so that the brain is rested and can also successfully concentrate on systematizing what it has learned.
What are the types of memory?
Photo by Michael Wysmierski: Pexels
Experts distinguish:
- ultra-short,
- short-term
- long-term memory.
Ultra-short-term memory refers to a period of just a few seconds - for example, when a telephone number just heard can be echoed without error. It is a kind of buffer for ongoing sensory perceptions, which is why it is also called sensory memory or immediate memory.
Short-term memory is the memory in which the brain processes its perceptions and separates them into important and unimportant information. Shelf life is a few minutes. Sometimes short-term memory is also called working memory.
Information is stored in long-term memory for days, weeks or even years. Only a small portion of the information recorded takes place in long-term memory, but the attachment to it is often even deeper - for example, many people can still remember their first day of school in old age.
Mnemonics and mnemonics. What's happened?
Classification according to the nature of mental activity
Individual characteristics of mnestic processes are characterized by what material is best absorbed: figurative, verbal, or both equally:
- Figurative memory. This is the ability to perceive and retain in memory certain visual images (ideas, pictures from life) and subsequently reproduce them; the type of memory is determined by a set of modality-specific sensations. This memory is plastic, can be long-term and appear unexpectedly. It is believed that its structure is made up of complex connections of neuronal units from different parts of the brain.
- Emotional memory. This type of memory is the result of fixations and new manifestations of emotional experiences; simply put, it is a memory for feelings. An impression that contains an emotional coloring is remembered instantly and without volitional effort, thus replenishing the structures of the human subconscious. This is a very stable mnestic type, the material of which can be reproduced completely involuntarily. Its biological basis presumably contains connections that combine subcortical neuronal links with links in different parts of the cerebral cortex.
- Semantic memory. This mnestic process correlates with the imprinting of verbal signs symbolizing what is happening in reality and internal experiences. Schematically, it represents series-connected linear links. If one of the links suffers, then this is fraught with a break in the entire chain, failure of the correct alternation of stored realities and erasing of certain fragments from memory.
Traditionally, the mnestic sphere is divided into 3 classic temporary types of memory:
- Iconic.
- Short-term (operative).
- Long-term (declarative).
The social significance and high prevalence of epilepsy contributed to the establishment of epileptology as an independent discipline. The chronic, progressive course of epilepsy is aggravated by the formation of mnestic-intellectual disorders, the negative impact of which on the social adaptation of patients is not inferior to the negative consequences of paroxysmal syndrome [7, 8].
Epilepsy is considered a highly disabling disease that causes stigmatization of patients in society. It is stigma that many consider an obstacle to improving the quality of life, which has a significant impact on personality, mood and behavior [3, 15, 16, 20].
The cognitive ability of patients with epilepsy is influenced by many factors, including the etiology of the disease, the type and frequency of seizures, the age of the patients at the time of their onset, as well as hereditary and psychosocial influences.
The final effect of antiepileptic therapy [21], since the peculiarity of treatment is the need for many years, sometimes lifelong use of antiepileptic drugs, which in 7-25% of cases lead to side effects and complications.
Recently, much attention has been paid to studying the influence of functional interhemispheric asymmetry on the nature of the ongoing process in patients with neurological and mental disorders - psychoses [4, 6, 18], various forms of deviant behavior [17, 22, 24-27] and with epilepsy itself [ 5, 9, 13]. Most authors come to the conclusion that lateralization is impaired in all of the listed types of pathology. To the above, we can add that interhemispheric asymmetry often determines the characteristics of the course of the disease and the effectiveness of therapy. Suffice it to say that among patients with schizophrenia and epilepsy, left-handed people are 2-3 times more likely than in the healthy population, and they mostly have severe forms of the disease [5, 23]. In addition, there is evidence that the processes of compensation and adaptation, as well as the course of the disease in right-handers and left-handers with damage to the ipsi- and contralateral hemispheres proceed differently [1, 19]. The effectiveness of therapy in epilepsy patients with right, left and mixed individual profiles of functional asymmetry also differs [13].
In this regard, the relevance of this study was determined by the high medical and social significance of the development of mnestic-intellectual disorders and the insufficient knowledge of the problem taking into account functional asymmetry.
The purpose of the study was to establish the pattern of formation of cognitive impairment in patients with epilepsy, taking into account the influence of the basic characteristics of the epileptic process and functional asymmetry.
Material and methods
We examined 132 patients (70 women and 62 men, aged 16 to 50 years; average age 27.8±8.9 years) who were treated in a specialized epileptology hospital at the Moscow Research Institute of Psychiatry. The main group consisted of 112 patients with cognitive disorders, the control group - 20 patients with epilepsy without cognitive disorders. The second control group included 20 healthy people, comparable in demographic indicators and level of education to the main group.
The work used clinical-psychopathological, psychometric, neurointroscopic, neurophysiological and statistical methods. When determining the form of the disease and the structure of the leading paroxysmal syndrome, the modern classification of epilepsy (New Delhi, 1981) and epileptic seizures (Kyoto, 1981) was used. To assess the profile of functional asymmetry, a set of techniques was used aimed at identifying preferences in the motor and sensory spheres [14]. Leading importance was attached to the motor sphere.
The level and structure of intelligence were assessed using the neurocognitive tests WAIS (Wechsler Adult Intelligence Scale) and the MMSE scale (Mini-Mental Test Examination). The NHS3 scale (National Hospital Seizure Severity Scale) was used to quantify neurological level disorders; Personality-psychopathology disorders were assessed using the Clinical Self-Esteem Scale (SCL-90) and the Munich Personality Test (MPT).
In accordance with the results of the clinical-psychopathological examination and cognitive tests, 3 subgroups of patients were identified in the main group according to the degree of intellectual impairment: subgroups of cognitive defect, borderline level and average level of intelligence.
In accordance with the ICD-10 criteria, these disorders corresponded to the headings: F-02.8 “Dementia”, F-06.7 “Mild cognitive impairment”. According to the division of dementia by severity [10], the subgroup of cognitive defect corresponded to moderate dementia, and the borderline subgroup corresponded to mild dementia. Let us dwell on these categories of disorders in more detail.
Dementia of moderate severity.
A cognitive defect consistent with dementia was observed in 17 (15.1%) patients. This subgroup includes patients with a general intelligence level below 69 points on the WAIS scale, with a pronounced mnestic-intellectual defect. Clinically, the cognitive defect was manifested by a significant decrease in memory (direct, indirect) and concentration, difficulties in generalization, switching, abstraction, and prediction. The pace of thought processes, counting operations and orienting-search reactions are also sharply slowed down, and for some patients they are inaccessible. Associative products are thorough, detailed, judgments are primitive, with a tendency to form super-valuable experiences. Criticism of their condition and behavior was sharply reduced; most patients in the group could not live without outside help. All of the above as a whole significantly complicated the perception of new material and comprehension, or made it impossible.
Mild dementia.
A borderline level of intellectual decline was detected in 37 (33.0%) patients. This subgroup includes patients with an intelligence level from 70 to 89 points on the WAIS scale, with a fairly pronounced mnestic-intellectual decline. What distinguished them from the patients of the previous subgroup was the possibility of independent living and self-care without restrictions. Clinically, the subgroup is represented by patients with decreased memory and attention functions, a slower pace of thought processes, but to a lesser extent than in the subgroup of cognitive defects. A decrease in the level of generalization and abstraction is characteristic. Thorough thinking, with difficulty switching. Most patients can develop simple new skills.
Mild cognitive impairment
was observed in 58 (51.78%) patients, with a general intelligence level from 90 to 109 points on the WAIS scale. The subgroup was characterized by a slight decrease in the cognitive sphere or its individual functions, which in most cases was detected only when using cognitive tests. Against the background of a slight slowdown in the pace of thinking and memory within normal limits, instability of attention was noted. Generalizations took place at the categorical level. The associative products are adequate, somewhat detailed, and emotionally charged. In the clinic, cerebrasthenic symptoms and emotional disturbances in the form of mood swings and dysphoric reactions came to the fore.
results
The cognitive sphere of patients with epilepsy is reduced with a high degree of reliability in comparison with the control group (Table 1).
The mnestic-intellectual functions of patients with moderate dementia are almost 2 times lower than in the control group of patients without cognitive disorders (63.0±6.7 and 112.7±4.6 points, respectively, t=–18.7; p=0.0000), and were formed to a greater extent due to verbal indicators: awareness, social orientation, counting, definitive thinking and memory.
The intellectual sphere of patients with mild dementia was significantly reduced, but to a lesser extent than in the group with moderate dementia (82.9±4.6 points, t=–16.2; p=0.0). The general level of intelligence of the borderline group, like the group of cognitive defects, was formed due to verbal functions: awareness, social orientation, abilities to understand idioms and generalization, and definitive thinking.
In patients with mild cognitive impairment, the intellectual domain was slightly reduced compared to controls (99.7±5.7 and 112.7±4.6 points, respectively). It was uniformly formed due to all verbal and non-verbal indicators, in contrast to the subgroups of cognitive defect and borderline level, where only verbal functions were manifested. Thus, patients with mild cognitive impairment were distinguished by the harmonious development of the intellectual sphere, despite its decline.
The data from Wechsler's cognitive technique were confirmed by the results of the MMSE test.
Analysis of the characteristics of the epileptic process influencing the appearance of cognitive disorder revealed the following factors to be of greatest importance.
1. Patients with moderate dementia were distinguished by the presence of diffuse slow-wave activity on the EEG with bilateral synchronous flashes, indicating dysfunction of the mid-brain structures, while the amplitude accent in the left temporal region led to a significant decrease in cognitive functions (p<0.05).
Patients with mild dementia were characterized by the presence of less pronounced diffuse slow-wave activity and the absence of bilateral synchronization, which, according to the results of cognitive tests, had a positive effect on their intellectual level. At the same time, the presence of focal epileptiform activity in the left frontotemporal region led to a statistically significant decrease in cognitive functions (p<0.01). Similar focal epileptiform activity, but with a focus in the right temporal region, correlated with mild cognitive impairment (p < 0.005).
2. The age of onset of seizures had a great influence on the cognitive sphere. In moderate dementia, the minimum values according to the Wechsler test were observed in patients with the onset of seizures before the age of 5 years (p <0.03). In mild dementia and mild cognitive impairment, the minimum Wechsler test score was observed in patients with the onset of seizures between the ages of 11 and 15 years (p=0.009 and p=0.0003, respectively).
3. The duration of the disease had an ambiguous effect on the cognitive sphere. In groups with cognitive impairment, as the age of onset of seizures increased (from 3.8 years for moderate dementia to 13.8 years for mild cognitive impairment), the duration of the disease decreased (from 21.9 to 13.3 years). At the same time, in the control group of patients without cognitive disorders at the latest age of onset of seizures (16.6 years), the duration of the disease corresponded to the group with dementia (Fig. 1).
Figure 1. Average values of the age of onset of seizures and duration of epilepsy in the study and control groups (years). This may be due to the characteristics of the premorbid level of intelligence and the degree of brain maturity at the time of the onset of the disease. It has been established that in patients with premorbidly high intelligence, a decrease in cognitive functions is detected to a lesser extent, later and is better compensated [2, 11].
Thus, when assessing the impact of the duration of the disease on the cognitive sphere, it is necessary to consider it in relation to the age of onset of seizures.
Among other factors of the epileptic process, the following had a significant impact on the cognitive sphere: high frequency of seizures (more than 1 per week), seizures with secondary generalization, and symptomatic form of epilepsy.
In accordance with the objectives of the study, the cognitive sphere of patients with epilepsy was studied taking into account functional asymmetry, in particular its motor component.
In the main group of patients with cognitive disorder, 14% of patients with left-sided motor asymmetry were identified. The first control group (patients with epilepsy without cognitive impairment) was entirely right-handed. The second control group (healthy) included 5% left-handed people.
Patients with epilepsy with left-sided motor asymmetry were distinguished by a heterogeneous structure in the genesis of handedness with compensatory and hereditary causes.
In 37.5% of patients with left-sided motor asymmetry, the following factors were identified in the anamnesis: pathology of childbirth with fetal extraction, complicated otolaryngological diseases, traumatic brain injury and infectious diseases of the brain with the formation of right-sided paresis. A nuclear magnetic resonance imaging scan of the brain in the left hemisphere showed organic changes of a cystic-atrophic nature in all of them. Due to these factors, patients were classified into the group with compensatory or pathological left-handedness.
The majority of patients (62.5%) were in the group of genetically fixed left-handedness due to hereditary conditions. Among the analyzed group of patients with epilepsy with left-sided manual preference, not a single case of sociocultural or environmental left-handedness was identified, which was a consequence of social upbringing, living conditions or imitation of relatives.
Patients with left-sided motor asymmetry had the greatest depth of cognitive impairment compared to right-handed patients. The proportion of dementia disorders among left-handed people reached 70%, among right-handed people - 45% (Fig. 2).
Figure 2. Distribution of cognitive disorders by severity, taking into account functional asymmetry.
The intellectual sphere of patients with epilepsy with a dominant left hand was characterized by a significant decrease due to a sharp deficit in nonverbal indicators (Table 2),
and also due to males (Table 3)
The level of intelligence of left-handed men was statistically significantly different from right-handed men (77.2 and 91.3 points, respectively, p = 0.006); among women, the differences did not reach a statistically significant level.
In the structure of the intelligence of patients with left-sided motor asymmetry, a deficit was found in both verbal (counting, p = 0.007; memory, p = 0.02; definitive thinking, p = 0.04) and non-verbal indicators (synthetic abilities, p = 0.01 ; hand-eye coordination, p=0.02; attention, p=0.02).
Analysis of factors in the formation of a cognitive defect, taking into account motor asymmetry, established the following patterns.
1. The early age of onset of seizures (before 5 years) and the duration of the disease (more than 20 years) in right-handed patients determined a significant decrease in cognitive functions, which was not confirmed in left-handed patients.
2. Focal epileptiform activity of the brain in the left temporal region led to a decrease in cognitive functions in right-handed patients and an increase in them in left-handed patients. A decrease in cognitive functions in patients with a dominant left hand was determined by the presence of diffuse slow-wave activity with the inclusion of bilateral synchronous discharges with an amplitude accent in the frontal region.
3. Taking barbiturates and clonazepam, as well as the factor of polytherapy with anticonvulsants, led to a significant decrease in cognitive functions in right-handed patients, in contrast to left-handed patients.
4. The prescription of antipsychotics led to a decrease in mnestic-intellectual functions in right-handed people, which was not confirmed in left-handed people.
Meanwhile, in women, the factor of left-handedness correlated with the duration of remission (p=0.0001, t=4.02). The average duration of remission in women with the dominant left hand was 3.93±5.15 years, with the right hand - 0.66±1.24 years. This allows us to consider left-sided motor asymmetry in women as a predictor of a prognostically favorable outcome of therapy in relation to paroxysmal syndrome.
Discussion
The study showed that a number of factors take part in the formation of mnestic-intellectual decline (defect). In this case, the defect can form both as a result of brain damage and epileptic activity itself, and as a result of the negative effect of antiepileptic therapy. Among the leading risk factors are the younger age of patients at the time of the onset of the disease, the high frequency of seizures (more than 1 per week) and their secondary generalization; Long-term neuroleptic therapy, especially clonazepam and barbituric drugs, significantly aggravates the development of cognitive defect. Studying the profile of lateral organization taking into account gender makes significant adjustments to the understanding of the formation and course of cognitive decline in epilepsy. The revealed influence of left-sided motor asymmetry on the formation of a pronounced intellectual defect is apparently due to a decrease in the right hemisphere functions of the brain, which manifests itself to a greater extent in men. It is likely that the left-sided profile of brain asymmetry is an unfavorable prognostic factor in relation to the cognitive sphere. At the same time, in women it contributes to the formation of remission of paroxysmal syndrome. It is obvious that work on studying the relationship between the asymmetry profile and various manifestations of epilepsy, including intelligence, should be continued.
Types of memory. Short-term and long-term memory
Mnestic activity is a special brain activity that allows you to learn to keep large amounts of information in your head for a long time; operate with concepts.
https://www.youtube.com/watch?v=ytdevru
Memory is divided by modality into motor, emotional, figurative, verbal-logical. There is also a division into voluntary and involuntary.
Based on storage duration, memory is divided into instantaneous, short-term and long-term, or indefinite. Information that enters short-term memory, with constant fixation of attention on this material and repeated repetition, passes into long-term memory.
Intellectual-mnestic activity
Memorization is closely related to intellectual activity. And by training the intellect, we thereby develop memory.
Mnestic activity is the ability to learn new things and adapt to a changing reality. If you work in one job for many years and fulfill standard requirements, your intelligence decreases. A person must constantly study something, be interested in new trends in science, and have a developing hobby.
Children under 5 years of age develop very quickly. Their consciousness does not differentiate the incoming flow of information into “bad” and “good”, “profitable” and “unprofitable”. They perceive absolutely everything.
For the development of mnestic activity in children, it is important to communicate with them in a playful way. It is the game that develops intelligence, not memorization.
Steps to Prevent Memory Problems
It is impossible to completely protect yourself, but some methods show good results:
- Brain training and mental stimulation (eg reading, solving puzzles, learning languages).
Photo by George Milton from Pexels
- Exercise and fitness (at least 30 minutes three times a week)
- A little stress.
- Get enough sleep (six to eight hours a day).
- Healthy eating (fruits, vegetables, whole grains, omega-3 fatty acids).
- Water (about 2 liters per day).
- Moderate alcohol consumption.
Meeting with friends and acquaintances makes people healthier. Therefore, a person with a lively social environment is less likely to get sick. It is important to keep in touch with your family and see friends often. New encounters also challenge and stimulate the brain. You need to meet new people and do something good for others to stay healthy.
Studies have shown that the likelihood of developing dementia increases by 50 percent even with a slight deficiency of vitamin D. Therefore, if possible, it is necessary to get outside for at least 20 minutes every day. Sunlight stimulates your own production of vitamin D.
Mechanisms of regulation and imprinting
The recording of new information goes through three stages in time: initially, based on the work of the visual, auditory and tactile analyzers, an engram is formed, that is, a special trace in the iconic memory. At the next stage, the available data is sent to the higher authorities of the brain. In certain cortical structures and parts of the limbic system, the incoming material is analyzed and sorted.
It is known that the hippocampus acts as a kind of filter, classifying all this and discarding what is unnecessary, and the task of the temporal region is to establish relationships with areas where engrams are stored from other parts of the brain. At the last stage, all this is translated into a clear circuit of long-term memory.
Diagnosis and treatment concept
Oligophrenia and its degree are determined using standard psychological tests, through which the intellectual quotient (IQ) is derived:
- idiocy – IQ < 20;
- imbecility - IQ 20-49;
- debility – IQ 50-69.
Diagnosis of psychoorganic, Korsakoff, dementia and concomitant syndromes depends on the underlying disease that caused the deviations.
Standard tools for examining a patient are MRI, ultrasound of the brain, as well as blood tests and observation by a psychiatrist.
Relationship between attention, intelligence and memory
The processes of mnestic activity are determined by the ability to voluntarily maintain attention on one object. Attention is a program that ensures that information that needs processing is retained in the field of consciousness. Weak control of attention is the key to the fact that it is difficult for a person to remember facts; even with good intelligence, he will not be able to achieve success in his profession.
Also with low intelligence. Even good attention, the ability to focus for a long time on one object will not help develop good memory if the intellect is poorly developed.
Factors influencing intelligence
The basis for the development of human mental abilities is made up of three main factors:
- Heredity. Genes are considered one of the main factors. It has been experimentally proven that in highly intelligent families, children grow up more developed than their peers. Indicators of memory, thinking, speech literacy and ability to concentrate are usually higher in such children.
- Environment. It is this that forms a person’s system of values, aspirations and goals. The ability to correctly choose your life task helps the intellect to develop to the proper extent.
- Race, gender and age. A number of studies confirm that some races exhibit signs of low intelligence to a much greater extent than others. So, for example, Europeans are, on average, smarter than people from Africa, and men are smarter than women. Age also affects intelligence - the peak development of mental abilities occurs around the age of 25. Later, with age, intelligence gradually fades away.
Reasons for violations
When a person during a study cannot remember 4 objects or words out of 10, researchers can note disturbances in mnestic activity. The causes of memory failures can be physiological or psychological.
Let's try to understand the cause-and-effect relationships that lead to a deterioration in the ability to perceive, analyze and remember information^
- Exhaustion of the nervous system due to stress or neurosis.
- Severe damage to the frontal lobes of the brain due to injury or stroke.
- Consequences of infectious diseases (meningitis, arachnoiditis) affecting the structure of the brain.
- Affective-emotional instability.
- Congenital brain abnormalities. Such as schizophrenia, childhood autism or dyslexia.
- Inability to regulate attention, lack of focused effort.
https://www.youtube.com/watch?v=ytpressru
Functional memory disorders, which are based on prolonged neurosis or attention disorders, are treated with the help of a psychologist. But more serious disorders require long-term treatment. Moreover, late treatment often leads to the fact that it becomes impossible to eliminate the disorders.
There are various reasons why mnestic processes suffer greatly. In psychology, this is a significant topic for research, since memory disorders underlie many mental illnesses. For example, patients with manic-depressive syndrome often have impaired memory function.
Modality-specific regulation of memory is dependent on the work of the primary fields and functional areas of the cerebral cortex. If their functioning is impaired, memory processes are also impaired. The most severe disorders of mnestic processes are those that are caused by organic changes in the brain.
Modal-nonspecific disorders are formed due to pathologies of subcortical brain structures: the neural network of the brainstem, limbic system, hippocampus. If the activity of the hippocampus is suddenly disrupted, “Korsakoff syndrome” may occur, in which the victim, having retained long-term memory, loses the ability to remember recent events.
What are the types of mnestic disorders?
- Selective disorders
The patient does not remember either verbal or spatial information.
- Quantitative memory impairments such as:
Here we are talking about anterograde amnesia, when not only are individual connections missing, but there are also obvious gaps in memory for a certain period of time; retrograde amnesia, when there is a loss of memories before a certain event; hypermnesia - a very rare memory disorder where selection processes in the brain operate to a limited extent for those affected.
- Qualitative memory impairments
The last group consists of déjà vu experiences that are fakes. For example, it may be that incorrect memories are stored in stressful situations.
Memory research methods
Canis therapy, carried out in boarding houses and social homes for adult patients with depression and mild dementia, is based on the method of group psychotherapy. Group psychotherapy is a direction born from the demands of life itself: nurses at one of the private hospitals in the USA noticed that conversations with patients conducted in a group of patients have a much greater impact on their well-being, interaction with each other, and improvement of mood than those conducted individually.
And in 1905, the American doctor Pratt began to use psychotherapeutic groups as a convenient and cost-effective way to inform patients, without initially finding out their psychotherapeutic capabilities. Subsequently, he noticed that in a psychotherapeutic group, the effectiveness of assistance consists of the influence of one person on another, of the emerging relationships of understanding and group solidarity, as well as of the reduction of pessimism and feelings of isolation.
The most important factor of effectiveness in group psychotherapy is that the group becomes a “model of the world” in which each participant begins to manifest himself in his own way, which means he has the opportunity to notice, analyze and experience how and in what way he manifests himself in relationships with other people, how they react to it (through “feedback”), what thoughts and feelings arise in situations of interaction with different people.
Group psychotherapy is carried out in the form of 1.5-2 hour sessions in a group of people who sit in a circle and discuss topics either arising from the experience of the participants or suggested by the psychotherapist. A variety of additional methods are also used, organically connected both with the personality and education of the group leader, and with the group request.
Methods that promote the development of non-verbal methods of interaction (for example, psycho-gymnastics), strengthening and clarifying feelings, and role-playing games can be used. As a rule, the very appearance of a dog in such a group causes a flow of positively colored memories, but if you stimulate patients with questions about what kind of animals they had, then the communication becomes even more active.
At the beginning of work, you need to introduce the group to dogs, at the rate of 2-3 dogs for 10-15 people, tell patients about the animals in as much detail as possible. Talk about where the dogs live, how they are trained, and why the counselor chose this or that breed. After this, you can start brainstorming the merits of different breeds and types of dog training.
How to improve the patient's condition?
When selecting a treatment regimen for a patient, it is important to first establish the cause of the development of cognitive disorder. Therefore, after assessing the mental status, a comprehensive examination of the patient is carried out
Treatment tactics for disorders are determined based on the severity of the disease and the cause of the brain dysfunction. In the treatment of mild to moderate dementia caused by Alzheimer's disease or vascular pathologies, acetylcholinesterase inhibitors or Memantine are used. However, the effectiveness of these drugs has not yet been proven. They are prescribed mainly to prevent further progression of the pathological process and the development of dementia.
In case of diagnosing vascular pathologies that provoke a failure of brain activity, the following are used:
- phosphodiesterase inhibitors promote vasodilation, which leads to normalization of blood circulation;
- α2-adrenergic receptor blockers suppress the actions of the sympathetic nervous system, which lead to the narrowing of blood vessels.
In addition to these medications, in the presence of neurological disorders, various therapeutic tactics are used to correct the patient’s behavior. It takes a lot of time to complete this task, since such treatment involves a consistent transformation of the human psyche.
Dyslexia due to memory impairment in children
Disorders of mnestic processes quite often respond to drug therapy, as well as other methods of treatment. Options for their use depend on the specific diagnosis; in particularly severe cases, at least relief of symptoms is possible. The basic therapeutic regimen is built on the following principles:
- relief of an acute condition (for psychosis, trauma);
- consumption of vitamins;
- treatment with psychotropic drugs (tranquilizers, antipsychotics);
- correction of cerebral circulation (nootropics: “phenibut”, “phenotropil”, “mexidol” and others).
In addition to the main treatment, the following are prescribed:
- balanced diet;
- medicinal herbs (valerian, ginger, motherwort);
- cognitive development of memory (various hobbies, memorizing poetry, mastering new languages, educational games);
- individual work with a psychotherapist.
In childhood, the correction of mnestic processes is primarily exercises based on intermodal synthesis, that is, on the transfer of information from the level of one modality to the level of another:
- Transfer from tactile to visual modality. You need to take three-dimensional objects of various shapes and then draw them on paper in a random order. Next, ask the child to close his eyes and feel the objects, and then ask him to open his eyes and choose the correct object from the ones drawn.
- Translation from tactile modality to auditory and speech. The child also closes his eyes and feels a three-dimensional object, then, with audio recordings turned on, you need to ask him to select the sound corresponding to this object.
- Translation from visual to tactile modality. The child is asked, with his eyes closed, to find by touch the figures shown to him before.
- Translation from auditory to visual modality. It is necessary to turn on an audio recording for the child with a certain speech sound, or the sound of some mechanism or vehicle, and then invite him to find the corresponding image on paper or draw it himself. Regardless of which mnestic type is being corrected, a certain sequence must be followed. First, mnestic recognition processes are formed. Then - reproduction, and finally - selectivity.
It is very important to begin the timely development of gnostic and mnestic processes (that is, cognition and memory) in early childhood. To avoid problems in the future.
So, mnestic processes are complex and subtle activities. Which occurs in the human brain at the neurophysiological, biological and mental levels. These processes, which make up the mobile structure of our memory, can be subject to disorders of a different spectrum depending on the nature of the damage to the nervous system. If the cause of the disorders is not deep organic lesions of the brain, then with the modern approach they can be fully corrected.
Impaired memory of words and objects, difficulties with speech in early childhood may be associated with dyslexia. This is a special disorder of mnestic activity associated with a congenital anomaly in the region of the language center of the brain.
With this syndrome, the child experiences difficulty perceiving speech and dividing the flow of sounds into its component parts. Naturally, the development of memory and thinking in such children is slowed down. Studies of mnestic activity in children show that working with them, communicating, and pointing out errors of perception contribute to recovery from the syndrome.
It happens that the cause of difficulties in mastering writing is associated with visual-perceptual disorders.
Clinical picture
Manifestations of intellectual disability are a variety of clinical and psychophysiological conditions, depending on a number of factors. Such disorders manifest themselves in the form of weak curiosity and slow learning. Such children have practically no receptivity to the new. In this case, primary disorders are observed from the first days of a child’s life:
- there is no reaction to external stimuli;
- shows interest in the world around him late;
- the behavior of such a baby is dominated by lethargy and drowsiness, but this does not exclude loudness and anxiety;
- the baby does not know how to distinguish between his own and strangers;
- does not show keen interest when communicating with adults;
- does not show interest in toys hung above the crib, and does not respond to toys in the hands of an adult.
In children of the first year of life with various forms of intellectual impairment, the grasping reflex is absent for a long time. Only by the age of two or three do they experience some shift in mastering manipulation skills, but intellectual deficiency manifests itself in behavior and play activities.
For a long time, children cannot take care of themselves independently, do not show a keen interest in anything and do not show curiosity. Interest that rarely arises quickly disappears. During games, such a child is limited to basic manipulation, has little contact with surrounding peers, and moves little.
In older preschool age, he is characterized by a lack of interest in intellectual pursuits. In games with peers, such children are not independent and do not show initiative, while copying the children around them.
Important Droppers for brain vessels and strengthening the nervous system
In communication with peers they never have the status of a leader. These children are much more willing to play with younger children, and tend to be overly active and bring disorganization into the game.
Intellectual disorders come to the fore at school age: they are especially noticeable in educational areas of activity and behavior. The perception of new information is slow, and educational material is absorbed in a narrow volume. Students with intellectual disabilities cannot identify the main or general thing in a picture or text and do not understand the connections between parts. They do not perceive the logic of events, and when retelling a plot or describing a picture, the reproduction is meaningless.
Most children in this category have local impairments, which are expressed by difficulties in perceiving concepts such as “right-left”, “above-under”, and mastering school skills. Some children with similar pathologies do not distinguish between the right and left sides even by the age of nine, and are often unable to find their class. Many of them have difficulty determining the time on the clock, days of the week, months and seasons.
Very often, such children suffer from phonetic-phonemic speech underdevelopment and are unable to correctly reproduce the lexical-grammatical structure of a sentence. They are characterized by a poor vocabulary, so they have difficulty expressing their decisions and actions. Questions are usually answered impulsively, without thinking about the answer. The development of children with intellectual disabilities is characterized by impaired attention function, frequent distractibility and rapid exhaustion.
Correction
Problems with memory have a negative impact on your studies and career. What can you do to improve your memory? There are several methods for correcting mnestic activity:
- If a person works with information, he needs to constantly get enough sleep.
- Take breaks during the learning process. The brain needs to rest and “reboot.”
- Organize material to make it easier to comprehend and remember. Build tables, pictures, diagrams.
- Use associations when learning.
- Remember more often the poems you taught at school.
To improve memory ability, it is recommended to take brain vitamins. These are Omega-3, glycine, all B vitamins.
https://www.youtube.com/watch?v=cosamomglavnom
If there are serious disturbances in the functioning of the cerebral cortex due to injury, more serious chemicals and treatment under medical supervision are required.
Disorders indicating illness
One of the most common memory disorders in old age is dementia, especially in the form of Alzheimer's disease and dementia. These diseases are usually progressive, that is, they become stronger over time and increasingly limit a person’s mental activity. In addition to memory impairment, problems with language expression and orientation to one's surroundings are common.
Giphy