Depression in children and adolescents
Depression in children is a mental disorder that manifests itself as follows: bad mood (tearfulness, moodiness), obsessive actions (slowness of movements), negative thinking, decreased appetite. In childhood, depression rarely corresponds to classical descriptions of depression, so it is not always possible to identify this disease at the initial stage.
Depression in children manifests itself in different ways, depending on the age of the child and the causes of the disease. For example, children under three years of age may suffer from depression due to damage to the central nervous system. The disease develops as a result of damage to brain cells during severe illnesses affecting the nervous system and family history. Also, the cause of a child’s depressive state may be a break with the mother: physical separation, emotional alienation, difficult family environment.
The cause of childhood depression in preschool children is often the attitude of parents: the use of physical and emotional violence, excess care and control/lack of involvement in the child’s life and indifference. Social relationships can also be a source of stress for a child.
For school-age children, the academic load increases, social relationships become more complicated, and some children have difficulties in achieving their goals.
It is important to note that depression is a multifactorial disease that is influenced by biological, genetic and psychosocial causes. There is a classification of depression according to the duration and severity of the disease:
• depressive reaction;
• depressive syndrome;
• depressive disorder.
Symptoms of depression in children
Children cannot evaluate their emotions and be aware of them, so it is necessary to pay attention to the child’s somatic symptoms, such as headache, malaise, and indigestion. However, laboratory tests remain unchanged.
In a depressed state, a child’s emotions are characterized by increased anxiety, fears of the dark, and loneliness. Small children cry, scream, panic if their mother leaves or they communicate with strangers or are in a new environment. Children may have difficulty adapting to kindergarten; they may develop various phobias and panic attacks (attacks of rapid heartbeat, suffocation, fear of death).
In primary schoolchildren, depression manifests itself in behavioral changes: isolation and indifference, loss of interest in communication and games. The child may complain of boredom, and a decrease in interest in life is a clear sign of depression. Emotional regression may be noticeable in children: constantly crying, gloomy, embittered.
How to diagnose depression in children?
To make a diagnosis, it is necessary to exclude somatic pathology, determine the nature of the disease and accurately determine the cause of the disease.
Diagnosis includes a comprehensive examination using the clinical interview method. Depression in children under 4 years of age is identified by the method of exclusion and determination of risk factors (pre- and postnatal damage to the central nervous system, heredity). Children over 3-4 years old undergo special psychodiagnostic techniques. The psychologist determines the emotional sphere and characteristics of the child’s social interactions.
Treatment of depression in children
The treatment of depression is based on an integrated approach, which includes: drug therapy, cognitive behavioral therapy, family psychotherapy.
Doctors at the Children's Medical Center carry out:
- psychological diagnostics on issues of development, behavior and education of children;
- correctional and developmental classes (individual and group);
- family psychological trainings;
- classes in the neurosensory room.
Make an appointment with a psychotherapist in Moscow by phone: +7 (495) 727-11-66.
Make an appointment
Treatment of childhood depression
Diagnosis of childhood depression occurs through a clinical interview with a psychiatrist or psychotherapist who specializes in child development. A psychiatrist may prescribe medication to help relieve some symptoms and normalize the child's mood. The psychotherapist will work with the patient and his parents using cognitive-behavioral or dynamic psychotherapy techniques. Unlike adults, it is quite difficult to explain to a child of primary school and preschool age that his condition is a disease that requires certain actions and treatment. Treatment for childhood depression usually occurs through music, art, games and sports. By participating in games, a child can express himself, and through art, he can perceive the psychotherapeutic work of a specialist.
Often, parents are unable to help their child cope with depression because they themselves are the cause of his condition. The psychotherapist works with parents and provides them with the tools to properly interact with the child. During the sessions, they learn about methods of psychological support in such situations and learn to apply them in practice. If parents meet halfway, cooperate with a psychotherapist and follow all recommendations, most symptoms of childhood depression can be relieved within a month. The younger the child, the faster the treatment process occurs.
- Depression
Normal or depressed state
Your child may feel sad, depressed, and cry for a while. This is a natural and extremely necessary way for our psyche to give vent to emotions.
You should not immediately run to a psychoanalyst if your child had a fight with friends or lay in bed all day. Watch!
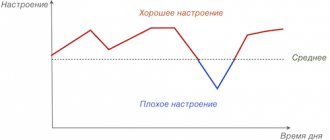
You need to worry when symptoms of depression appear more and more often. And the child is in a normal state of mind less and less often. The line between normal and not normal is very thin.
Depressive triad
In psychotherapy, there is a symptom complex called the depressive triad - three main manifestations of depression:
- Bad mood.
- Deterioration in the quality and speed of thinking.
- Lack of motor activity (lethargy, apathy).
These three symptoms are indicators of the child's condition. If you observe kinks in one or more of them, contact a specialist.
Diagnostics
If you suspect depression, you should visit a psychotherapist or psychiatrist for an accurate diagnosis. Diagnosis is based not only on symptoms visible to the average person.
When diagnosing, the doctor collects information that he takes directly from the child, his parents and teachers. The patient undergoes a brief psychological test. The Beck scale, Hamilton scales and Montgomery-Asberg tests are used.
Self-diagnosis is not effective. Diagnosing a child with depression is difficult even for specialists. The reasons are that the symptoms are very variable, unstable, and masked by somatic manifestations. Children's isolation and sadness are often falsely perceived as depression. And vice versa - depression is perceived as isolation and sadness. One or three symptoms are not a sign of disease.
If a child is irritable or sad, this does not mean depression. Manifestations also depend on the characterological characteristics of the individual and age.
Pathogenesis
There are biological prerequisites for the formation of the disease that can be tested in a medical setting. We are talking about a deficiency of neurotransmitters in brain synapses (norepinephrine, dopamine), and an increase in cortisol levels. Disorders of melatonin secretion are characteristic. Patients exhibit morphological changes in the amygdala and frontal cortex.
Most children with depression experience a lack of maternal love. Many experienced social and economic changes and acute stress before the onset of the disease. The disease is more often diagnosed in children who, before the disease, were already quite introverted, anxious, vulnerable and neurotic.
Complications
Without medical help, childhood depression progresses into adult forms of the disorder. Symptoms worsen, new manifestations arise. Disorders increasingly affect the somatic state. During adolescence, attention should be paid to suicidal behavior. Many depressed teens demonstrate intentions to harm or kill themselves. This manifests itself in alarming moments:
- in the conversation there is a noticeable lack of hope for the future and self-confidence;
- no interest in previously favorite activities;
- indifferent attitude towards oneself or towards parents;
- gross deviations in behavior;
- preparations for suicide - writing farewell notes, wills;
- auto-aggression - self-mutilation or involvement in life-threatening activities;
- passion for the topic of death;
- straightforward statements or threatening statements about intentions to commit suicide.
The only attack of depression suffered is a huge likelihood of recurrence of the disease.
Who is at risk?
The reasons for the development of depression in adolescents are different and are determined individually in each specific situation. What makes a person vulnerable are emotional, social, and also physical factors: violence and abuse, social status among peers, family well-being, performance at school or university. Some teenagers are at higher risk of depression.
This problem affects children with chronic illnesses or other neuropsychiatric disorders, such as autism spectrum disorders. Adolescents who became parents or entered into early marriage, as well as ethnic minorities, are at risk.
What else can you do
Parents always feel like they are not doing enough for their children. Especially when it comes to treating not the simplest mental disorder. Childhood depression - what else you can do for your child:
Organize your favorite activities.
During therapy, it is important to create the most comfortable home environment for the child. Due to his current difficult condition, it is worth giving up travel, noisy holidays, and lifestyle changes.
On the contrary, remember what brought joy to the child in the past. For example, singing karaoke, playing board games, cooking food together, caring for a pet. Return to these activities.
Create a space of trust.
Children make contact more easily not during a so-called confidential conversation, but in the process of some kind of joint activity. Do something with your child and talk unobtrusively. Do not ask with pressure, but simply give the opportunity to express your emotions, plans, fears. Make it a habit to communicate this way during joint activities.
Do not punish for revelations.
Inconvenient truths are hard to hear. But if you have reached a certain level of frank communication, therapy brings results, and the child decides to tell you about the not so pleasant moments in his life, do not betray his trust. Refuse the impulse to judge, subtract, punish. By these actions you will only close with a concrete wall the small door of trust that has opened in front of you.
Gradually involve your child in social interaction.
If a noisy company does not yet arouse his enthusiasm, start small. Communication with even one friend will help gradually return the child to full social interaction with others.
Bring physical activity back into your child's life.
Hiking, cycling, sports games, rollerblading or skating - any physical activity is suitable. Physical activity will not only distract you from sad thoughts, but also help relieve muscle tension.
Control your obsession with gadgets.
Being stuck on the phone itself has a negative impact on children, and during periods of depression it can become a factor slowing down recovery. It is better to leave online games and social networks for later - when the child feels better.
Watch your diet.
It has been proven that an abundance of carbohydrate foods has a negative effect on mood. Fuel your child's energy balance with healthy foods: healthy fats, quality proteins, fresh fruits and vegetables. Don't forget about healthy treats.
Give your child enough time to sleep.
If he's sleeping, don't wake him up. If he can’t sleep, turn on calm music, give him a glass of warm milk, and sit next to him. Adequate sleep is the key to rapid restoration of both physical and mental strength of the child. If you have persistent insomnia, consult your doctor about taking mild sleeping pills.
Classification
To classify depression, it is worth familiarizing yourself with the ICD-10 headings:
- F93.0 “anxiety disorder due to separation” - anxiety in relation to the person to whom the child is attached and from whom he was separated;
- F93.1 “phobic disorder” - fears that do not correspond to a certain age phase, pathological level of anxiety;
- F93.2 “social anxiety disorder” - problems in social interaction, a high level of shyness and tightness when communicating with strangers, but the absence of such indicators when interacting with family members;
- mixed variants of pathology - the presence of symptoms of all three categories.
Anxiety disorder of the first type is expressed in the child's concern about possible accidents associated with the person from whom the separation occurred. Reluctance to attend school due to fear of separation is typical. There is a fear of loneliness, nightmares about separation.
In social anxiety disorder, disruption of social interactions comes to the fore. The presence of distress and discomfort is noted in situations where the child involuntarily participates in social activities. He begins to cry, his speech is confused, and there is no spontaneous speech. Symptoms do not go away for at least 4 weeks. In this case, the disease does not progress as a gross disturbance of emotions or behavior, and there are no characteristic symptoms of PTSD or other diseases.
I'm a teenager and right now I'm contemplating committing suicide.
Be sure to talk to someone! If negative feelings become so unbearable that you can't find any solution other than self-harm, you need immediate help! We understand that the decision to apply for it may not be easy for you, but it is truly very important! You need to turn to someone you trust, such as a friend, family member, teacher. If you have no one to discuss your problem with, share with our specialists who are ready to listen - call the hotline:
- 8 800 2000 122 - hotline for psychological assistance to children, adolescents and their parents, 24 hours a day.
- 8 emergency psychological assistance center of the Ministry of Emergency Situations.
- 8 children's helpline of the Moscow Department of Education, 24 hours a day.
- 051 from the city center or +7 495 051 (MTS, MegaFon, Beeline, Tele2) - emergency psychological help telephone number of the Moscow service for psychological assistance to the population.
- 8 hotline for teenagers and their parents in St. Petersburg.
Don’t forget also about emergency medical services (103) and emergency services (112).
Whatever your situation, remember that there is another solution, even if you don't see it right now. Having thoughts about harming yourself or others does not make you a bad person. The disease can make you think and feel things that were previously unusual. If your feelings are uncontrollable, try to wait another 24 hours before taking action, and during this time, do not isolate yourself and be sure to talk to someone. Tags:
- Depression
- Children
- Teenagers
- Psyche
To leave a comment you must be an authorized user