Can the temperature rise with a concussion?
What does her promotion mean? What to do to get rid of the fever? All these issues are discussed in this article. A fall from a height, a blow to the head, a collision with a wall, an accident - all this can provoke a traumatic brain injury and concussion. The main symptoms of this condition are dizziness and nausea. But can there be fever during a concussion, or is this abnormal?
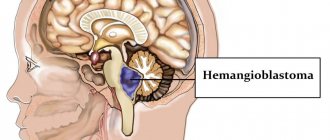
What is a concussion
It is important to distinguish between two conditions - concussion and brain contusion. Both are types of traumatic brain injury (TBI). A concussion is a minor injury, while a bruise is a more serious condition involving tissue damage. Often, as a result of a traumatic brain injury, a person receives both a concussion and a bruise.
With TBI, a concussion is observed in 70% of patients, a mild brain contusion is observed in 15%. It is difficult to draw clear boundaries between a concussion and a mild injury based on symptoms. As a result, ordinary people, and doctors to simplify things, call everything a concussion.
Further in the article, we will also not distinguish between these states, so as not to complicate an already difficult topic. However, let us say right away that elevated body temperature is characteristic of brain contusion. Therefore, when we say “fever (fever, low-grade fever) due to a concussion,” we will mean a bruise or more serious consequences of a head injury.
Diagnostics
After the examination, the doctor may prescribe additional tests, namely: x-rays, MRI, neurosonography, computed tomography or electroencephalography.
X-rays help reveal the integrity of the skull bones.
Neurosonography is prescribed for children under 2 years of age. Using this procedure, the doctor will be able to identify this or that brain pathology.
Electroencephalography will allow you to study the bioelectrical activity of the brain and assess the severity of the injury.
Computed tomography is an effective method for detecting brain damage.
Why does the temperature rise during a concussion?
A common cause of fever during traumatic brain injury is the presence of an inflammatory process in the body that began even before the injury. If a person had a cold the day before, then after an injury the temperature during a concussion can rise to 38.5 or higher. But this is just a coincidence: the concussion itself does not cause the fever. In this case, the injury became only a catalyst for another inflammatory process.
But the concussion itself also causes fever. Although the human brain appears to be well protected, it is vulnerable to various mechanical damage. Gray matter is located in cerebral fluid, which protects it from impacts on the skull. With a strong impact, the brain approaches the bone tissue and hits it. As a result, brain structures are displaced, which leads to the appearance of microcracks in blood vessels, ruptures in capillaries and disruption of neural connections.
The human neural network is a collection of nerve cells (neurons) of the brain and spinal cord, and the peripheral nervous system. A neural network consists of neurons that are chemically or functionally connected to each other. One neuron is connected to many others using neural connections.
With a traumatic brain injury or concussion, the patient's temperature may rise. Neurologists say that its fluctuations in the range of 37-37.5 degrees are absolutely normal. During injury, the brain's thermoregulation center, the hypothalamus, can shift. And for neural connections to return to normal and the functioning of the thermoregulation center to improve, it takes at least a week. After this period of time, the indicator becomes normal - 36.6 degrees.
As for a significant increase in temperature - above 38 degrees, it can occur when the patient’s condition is serious. Fever is a sign of the development of infection in an open wound or hematoma, which has become an environment for the development of pathogenic bacteria. If you do not provide timely assistance to the victim and do not hospitalize him, then there is a risk of developing meningitis and a rapid rise in temperature to fatal levels of 41-42 degrees.
So, we found out whether there can be a high temperature with a concussion and bruise of the brain. It is worth understanding that its increase in such an injury does not always occur. It all depends on the general health of the victim, the individual characteristics of the body and the nature of the injury.
Mild traumatic brain injury is considered to be cases of direct or indirect mechanical damage to the brain with a Glasgow Coma Scale (GCS) score of 13-15 30 minutes after injury
Mild traumatic brain injuries in the vast majority of cases occur without consequences, or with transient disturbances that persist for several days/weeks.
Brain concussion
Concussion is defined as a complex pathophysiological process caused by traumatic biomechanical forces. Traumatic changes in the brain have a number of common clinical, pathophysiological and biomechanical characteristics.
Brain concussion
- can be caused by a direct blow to the head, face, neck and other parts of the body with kinetic energy transferred to the head.
- as a rule, leads to the acute development of short-term neurological disorders that resolve spontaneously.
- A concussion may be accompanied by pathohistological changes in the brain tissue, however, the development of symptoms is primarily based on functional disorders. Standard neuroimaging procedures do not reveal any traumatic changes.
- leads to the sequential appearance of clinical syndromes, among which there may not be loss of consciousness. Characteristic is a consistent decline in the severity of the disorders. However, it is important to remember that some of them can persist for a long time.
In addition to a concussion, a mild traumatic brain injury includes a mild brain contusion.
Symptoms of mild traumatic brain injury
Neurological
- Headache
- Nausea
- Vomit
- Double vision and “fog” in the eyes
- "Flashes" or "stars" in the eyes
- Balance disorders
- Dizziness
- Photo and sound sensitivity
- Noise in ears
Behavioral or emotional
- Lethargy
- General weakness or drowsiness
- Irritability
- Depression
- Anxiety
- Increased sleep duration, more than usual
- Difficulty falling asleep
Cognitive
- Feeling slow
- Feeling “numb”, “as if in a fog”
- Difficulty concentrating
Deterioration of the condition of a patient with a mild traumatic brain injury (appearance/intensification of headache, appearance/worsening of neurological symptoms, appearance of confusion and depression of consciousness) may indicate the development of an intracranial hematoma and requires urgent neuroimaging
For most patients, short-term symptomatic treatment is sufficient:
- for headaches, analgesics and NSAIDs (paracetamol, ibuprofen, naproxen) are used,
- for nausea and vomiting - anti-sickness medications and sedative antihistamines - for mild severity - Dramamine, Atarax, for severe - antiserotonergic drugs - ondansetron, granisetron (Avomit, Kitril).
Many famous people have practiced boxing and have likely suffered repeated traumatic brain injuries.
From this list, I am most impressed by Ernest Hemingway and Vladimir Vladimirovich Nabokov.
It was boxing that “discovered” Charlie Chaplin to the world; he worked as a sparring partner in the lightweight division, was noticed by the director of the Chicago Circus and invited him to perform the act “Boxing in the Arena.”
Exceptions: after 3 months, persistent sequelae in the form of cognitive, mental or neurological impairment remain in 10-15% of individuals who have suffered mild traumatic brain injury (Iverson, 2005). This condition is called "post-concussion syndrome."
Post-concussion syndrome includes at least three of the following groups of syndromes that developed within no more than 4 weeks after injury:
- Headache, dizziness, malaise, general weakness, increased sensitivity to loud sounds;
- Irritability, depression, anxiety, emotional lability;
- Memory and attention disorders, thinking disorders, which are perceived subjectively by the patient and are not recorded by neuropsychological tests
- Insomnia
- Decreased tolerance to alcohol
- Increased preoccupation with the symptoms described above with a hypochondriacal attitude and a painful sense of self
In patients with focal brain lesions, including traumatic ones, as well as in alcohol abusers, repeated, even mild, traumatic brain injuries significantly increase the risk of post-traumatic seizures and epilepsy.
The development of “boxer dementia” is rarely observed in individuals with repeated mild traumatic brain injuries. People with ApoE ε4 (a subtype of lipoprotein, a protein-lipid complex) are predisposed to this complication.
A small proportion of patients develop second-impact syndrome (SIS), a diffuse swelling of the brain after repeated trauma. More often it occurs in athletes against the background of symptoms of a previous concussion. In 1998, 17 cases were described, in 12 of them the description was incomplete. The 2013 paper did not identify conditions that could be clearly considered risk factors for SIS.
- perform craniography if it is possible to perform a computed tomography (CT) scan of the brain - skull fractures without brain contusion - casuistry. If a fracture is detected, a CT scan of the brain is necessary to exclude a bruise and hematoma; if not, the study does not exclude dangerous manifestations of injury in the patient.
- In practice, doctors often have difficulty assessing the bones of the facial skeleton based on radiographs, which also requires repeat CT scanning.
- If you have a tomograph, there is no need to waste time on echoencephaloscopy.
- If access to CT or MRI is limited, it is necessary to reasonably select those who really need the study.
Below, for your reference, are the different sets of indications:
Canadian set of indications*
- GCS score < 15 points;
- Suspicion of an open or depressed skull fracture;
- Clinical signs of a fracture of the base of the skull (hemotympanum, “raccoon eyes,” liquorrhea from the ears and nose, bruising in the parotid region “Battle’s sign”;
- Two or more episodes of vomiting;
- Age ≥65 years;
- Duration of anterograde amnesia ≥30′ from the moment of injury;
- Hazardous mechanism of injury (motorcycle injury, fall more than 3 feet (about 1 meter), or more than five steps;
*The scale is not suitable for cases with the possibility of developing disorders of consciousness due to causes not related to trauma, with a GCS score <13 points, patient age <16 years, if the patient is taking oral anticoagulants (warfarin, Pradaxa, Xarelto, etc.) or suffers from diseases with an increased tendency to bleeding.
New Orleans set of readings
- Headache;
- Vomit;
- Drug or alcohol intoxication;
- Persistent antegrade amnesia (impaired short-term memory)
- Traumatic injuries above the collarbone;
- Convulsive seizures;
- Age ≥60 years;
The risk of detecting brain pathology is higher in patients with a Glasgow Coma Scale score of 13-14 points 30 minutes after injury than 15 points. The following groups are identified according to the severity of risk:
Low risk - 15 GCS points after injury, without loss of consciousness, amnesia, nausea, vomiting, headache - risk of developing intracranial hematoma requiring neurosurgical treatment 0.1:100
Average risk - 15 points on the GCS in combination with loss of consciousness, amnesia, nausea, vomiting, headache - the risk of identifying an intracerebral hematoma requiring neurosurgical intervention is 1-3:100, a CT scan of the brain is necessary.
High risk - GCS score of 14-15, signs of a skull fracture, neurological deficit. The risk of detecting a hematoma requiring neurosurgical intervention is 6-10:100.
The group of high-risk patients, regardless of the clinical manifestations of the injury, includes persons with a history of taking anticoagulants before injury, and persons > 60 years of age.
In cases where a CT scan of the brain was not performed, it is recommended:
- for two weeks from the moment of injury, refrain from taking alcohol and painkillers, driving a car or other vehicles;
- inform your loved ones about the traumatic brain injury you have suffered and warn that if behavioral disturbances and increased drowsiness appear, you must call an ambulance,
- seek help yourself if your headache worsens, double vision, nausea and vomiting, weakness of the limbs and other neurological disorders occur.
“Qu'ils mangent de la brioche”, French - verbatim. “Let them eat brioche” - “If they have no bread, let them eat cake!”, Queen of France, Marie Antoinette, 1769
- conduct a CT scan of the brain after receiving a negative result from an MRI of the brain (the institution where the care is provided has an MRI, but no CT scan)
Due to the heterogeneity of conditions caused by biomechanical damage to the brain, which are characterized by impaired memory and orientation, sometimes with loss of consciousness (2013 definition of a concussion), the issue of neuroimaging of traumatic brain injury is complex. The diagnosis is based on the clinical characteristics of the patient; in most cases, conventional CT and MRI studies do not reveal changes in the brain substance in individuals with mild traumatic brain injury.
If a magnetic resonance imaging scanner is available, the method is sufficiently sensitive to detect focal traumatic changes in the brain and intracranial hemorrhages.
MRI, compared with CT of the brain, has greater sensitivity in detecting focal brain lesions. However, neither study provides results that correlate with the degree and nature of neuropsychological impairment.
Both research methods do not accurately detect signs of diffuse axonal damage.
In practice, it is important to identify conditions requiring neurosurgical intervention: hematomas, skull fractures.
The use of data on the nature and prevalence of brain contusions in forming a prognosis and rehabilitation treatment plan has not been developed.
— perform repeated neuroimaging studies (CT and MRI) without medical indications
Unreasonable anxiety from the attending physician is not an indication. Repeated examinations are indicated for patients with progression of disorders of consciousness and focal neurological symptoms, with the development of convulsive seizures. Performing a CT scan exposes the patient to ionizing radiation, which increases the risk of tumor diseases.
The harm from MRI of the brain to health has not been proven, but to the wallet of the patient and the medical institution it is undeniable.
— use rheoencephalography when examining a patient, both after injury and in the long-term period
The study does not provide valuable information, its results will differ with repeated studies, is not needed for the treatment of patients, and acts as an additional source of anxiety.
- perform electroencephalography in patients who have suffered a TBI and have not had epileptic seizures or their equivalents
After TBI, nonspecific changes are more often observed: single sharp waves, groups of sharp waves, less often, peak-wave complexes, uneven alpha rhythm; greater sensitivity to functional tests. The risk of epileptic seizures in people without focal brain damage is low, and the risk of developing epilepsy in people who have suffered early post-traumatic seizures within the first week after injury is also low.
— perform duplex scanning of the brachiocephalic arteries in all patients who have suffered a TBI
dissection of cerebral arteries is a rather rare complication of traumatic brain injury, usually accompanied by clinical signs of cerebrovascular insufficiency, headache and neck pain. Strokes caused by dissection of the precerebral arteries are benign.
Other symptoms of a concussion
Concussions manifest differently in children, adolescents and adults. The characteristic symptoms, in addition to temperature, in an adult are:
- sudden darkening of the eyes;
- loss of consciousness;
- nausea and vomiting;
- twitching of the eyeballs;
- noise in ears;
- dizziness;
- heart rhythm disturbances;
- increased drowsiness;
- feeling of numbness in the face;
- decreased sensitivity of fingers;
- increased anxiety, excitability, irritability;
- inability to focus the gaze at one point;
- absentmindedness;
- restless and sensitive sleep, insomnia.
A mild concussion has less severe symptoms than a severe one. But in both situations, a doctor’s consultation and possibly hospitalization are required.
You can read about the characteristics of concussions in children in a separate article on the website temperaturka.com.
How long does the temperature last after a concussion?
The increase in temperature and its duration as a result of traumatic brain injury depend on the severity. It can be light, medium, heavy.
- With a mild degree of concussion, the temperature remains normal, sometimes rising by a few tenths of a degree (maximum temperature - 37). The norm of 36.6 is restored within a few days.
- With moderate severity, the thermometer can rise to 37.5-38 degrees. This suggests that neural connections are broken and need to be restored. In this case, the temperature after a concussion can last up to one to two weeks.
- In severe conditions, a process of hemorrhage occurs and there is a risk of the temperature rising to a higher level, up to 40-42 degrees. A person suffers from severe headaches, nausea, vomiting, and memory disorders. This continues for several days, and then the degree gradually declines, subject to adequate treatment. But full recovery will take several weeks or even months.
Is it necessary to reduce the temperature during a concussion?
If the temperature does not exceed 37.5 degrees, then there is no need to bring it down. Provide the patient with bed rest and complete rest. If, during a concussion, the temperature rises above 37.5 degrees, and there are concomitant inflammatory diseases (ARVI, colds, etc.) in the background, then they need to be treated. But in the case of fever during a concussion in adults and children, it is strictly forbidden to take any measures on your own. You need to call a doctor at home or arrive at the hospital with an ambulance, after which it is the doctor who, after all the tests, will decide on hospitalization or home treatment, and also prescribe a course of therapy.
Treatment of concussion with fever
There is a general set of therapeutic measures that are used regardless of the presence of fever. If the condition is mild, the patient is sent home. You need to put it in a dark, regularly ventilated room, and also:
- protect from watching TV, computer and reading books;
- allow you to get out of bed only when necessary;
- do not give junk food - spicy, fried, pickled, sweet;
- avoid irritants such as loud music;
- relieve stress.
A complex of medications is used to treat concussion:
- diuretics to avoid tissue swelling and for better circulation of fluids;
- medicines containing potassium to maintain normal functioning of the heart muscle;
- sedatives to relieve anxiety and tension;
- nootropic drugs strengthen blood vessels and restore neural connections;
- non-steroidal medications relieve headaches and prevent general malaise;
- antiemetic tablets eliminate nausea, improve the functioning of the stomach and intestines;
- anti-inflammatory medications are used in case of a significant increase in temperature;
- vitamins and minerals accelerate the processes of regeneration and rehabilitation.
In the event of a sudden increase in temperature due to a concussion, you should inform your doctor about this change, who will adjust the treatment regimen.
Read also
Pinched nerve
This morning you arrived at your country house.
While taking out a heavy and large bag of tools from the trunk of your car, you suddenly felt a very strong, shooting pain in your lower back on the right side. Raise… Read more
Amyotrophic lateral sclerosis (ALS)
– “One of the most terrible human diseases... 3 letters...” – “Cancer” – “Not suitable...” Yes, dear ones, there is something worse than cancer. And this disease is called amyotrophic lateral sclerosis or...
More details
Neuropathy
In the human body, the work of internal organs and systems is regulated by the brain, namely by nerve impulses emanating from it. These impulses travel along nerve fibers. Damage to them can damage this...
More details
Myositis
Myositis is a group of diseases characterized by an inflammatory process in skeletal muscles. Depending on the cause of the disease, there are several forms of myositis: Autoimmune…
More details
Aphasia
Aphasias are speech defects that appear with minor brain damage, most often affecting the left hemisphere in right-handed people, and consisting of various forms of speech changes. Location and size...
More details
Consequences of temperature disturbances in head trauma
After an injury, if it is complicated by an increase in temperature, the following symptoms persist indefinitely:
- increased fatigue;
- irritability;
- weakening of attention and memory;
- sudden change of mood;
- apathy;
- slight dizziness;
- nausea, vomiting.
So, a concussion is sometimes accompanied by fever and fever. There are two reasons for this - natural (disruption of neural connections due to injury) and pathological (infection during severe traumatic brain injury, inflammation due to another disease). In both cases, the patient must be under the close supervision of a doctor and follow his recommendations. If you consult a doctor and strictly adhere to the prescribed treatment regimen, the risk of complications will be minimized. If you ignore the advice, then there is a possibility of complications even if the concussion was mild and occurred without fever.
It takes time to recover
A person who has suffered a head injury needs time to recover. Do not return to exercise until your doctor allows it.
Those who begin vigorous physical activity too early have a high chance of suffering a second concussion due to poor coordination and balance. New head injury may cause permanent damage
brain
Try to stop reading (especially on mobile devices!), watching TV, and working on the computer for at least a week.