List of known diseases starting with the letter “G”: Ganglioneuritis, Ganglioneuroblastoma, Ganglionitis of the pterygopalatine node, Soft tissue hematoma, Hematomyelia, Hemiballism, Hemorrhagic stroke, Ganglioneuroma, Hemangioblastoma, Hemifacial spasm, Generalized epilepsy, Germinoma of the brain, Hydrocephalus, Hyperventilation syndrome, Hyperkinesis, Hyper somnia , Hypertensive cerebral crisis, Hypertensive encephalopathy, Hypnic headache, Brain glioma
The process of inflammation of the pterygopalatine ganglion is called pterygopalatine ganglionitis. This disease occurs when an infection enters the human body. It manifests itself with very unpleasant symptoms.
General information about the disease
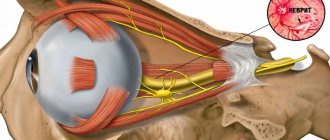
The pterygopalatine node is located directly in the pterygopalatine fossa, which is located in the area under the temple. Its node consists of three roots:
sensitive - formed by branches from the trigeminal nerve or maxillary nerve (II branch);- sympathetic - internal branch of the carotid plexus;
- parasympathetic - greater petrosal nerve.
The branches that arise from the pterygopalatine ganglion innervate the:
- eye area;
- lacrimal gland, orbital branches;
- nasal mucosa;
- ethmoid sinus;
- soft and hard palate;
- maxillary sinus.
Ganglionitis of the pterygopalatine ganglion is also known as Slader's syndrome. The disease is named after its discoverer. Slader described this type of pathology in 1908. The author identified all the possible symptoms of this disease, and also listed various methods of treating this disease.
Pathology is a very common type of disease of the nasal region. If the inflammatory process spreads to the nerve roots that are part of the pterygopalatine node, then the disease takes the form of ganglioneuritis (the clinical picture of ganglioneuritis is determined by the level and nature of the lesion). If the cervical ganglia are affected during the disease, pain and the following autonomic disorders may be detected:
- increased sweating;
- changes in color, temperature, sensitivity of the skin of the face and neck;
- soreness of the exit points of the trigeminal nerve;
- vascular spasms.
If the cervicothoracic ganglia are affected, this is manifested by a change in the localization of pain, temperature, increased sensitivity, and pain in the heart area.
With lumbar and pelvic ganglionitis, burning, paroxysmal pain appears in the lower torso, abdomen, inner thighs, and lower back. The pain often intensifies at night with the manifestation of severe asthenic syndrome, which manifests itself in the form of:
- increased fatigue and exhaustion with extreme mood instability;
- weakening of self-control;
- impatience, restlessness;
- sleep disorders;
- loss of ability for prolonged mental and physical stress;
- intolerance to loud sounds;
- photophobia;
- intolerance to strong odors.
Patients also experience irritable weakness, expressed by increased excitability and quickly followed by exhaustion, affective lability with a predominance of low mood with features of moodiness and displeasure, as well as tearfulness.
Book "Eye Diseases"
Chapter 20
The close anatomical relationship of the dental system and the organ of vision, common innervation with a number of border areas is manifested by symptoms and syndromes characteristic of a particular pathology.
<< CONTENTS
Crouzon's disease (craniofacial dysostosis)
Of the eye symptoms, bilateral, often significant exophthalmos is noted, which is associated with underdevelopment of the upper jaw and underdevelopment of the orbit. Sometimes exophthalmos is very strong. There is also divergent strabismus caused by expansion of the nasal root, hypertelorism. In the fundus there are congestive nipples followed by secondary atrophy, as a result of narrowing of the optic canal or increased intracranial pressure due to synostosis of most cranial sutures. Mongoloid type of palpebral fissures, astigmatism, and nystagmus are observed. There may be congenital subluxations of the lens, hydrophthalmos, and cataracts. The most persistent symptoms are exophthalmos and strabismus. Other symptoms include a tower-type skull deformation, a large convex forehead, a nose like a parrot's beak, aplasia of the upper jaw with its retraction back, prognosis of the lower jaw, epileptic seizures, and impaired sense of smell. Crouzon's dysostosis can be combined with an open bite, with syndactyly; two-phalanx fingers, polydactyly, cranial nerve palsies, hypofunction of the pituitary gland with adipose-genital dystrophy have also been described. The disease is regarded as a family-hereditary anomaly of the skull, both the cerebral and facial parts, such as oxycephaly with dominant transmission and high penetrance. Crouzon dysplasia is considered a form of first branchial arch syndrome.
The syndrome of the first branchial arch includes all forms of clefts of the upper lip and palate, especially cases of their combination with anomalies of the auricle in its anterior third, as well as some forms of transverse and longitudinal clefts of the face.
Treatment is surgical.
Meyer-Schwickerath-Grüterich-Weyers syndrome
This is oculodental motor dysplasia, i.e. a combination of changes in the eyes, face, teeth, fingers and toes. From the side of the eyes, epicanthus, narrow palpebral fissures, ptosis, bilateral microphthalmia, hypoplasia of the anterior layer of the iris, congenital glaucoma. On the dental side, enamel dysplasia, brown staining of teeth, micro- and oligodantia, abnormalities in the shape of teeth, and sometimes a cleft palate. Among the anomalies of the limbs, one should note the elongation of the skin fold between the fingers, the square appearance of the middle phalanx of the little finger, hypoplasia or complete absence of the middle phalanges in one, two, and sometimes all five fingers, dystrophy of the nails of the fingers and toes or even their absence. There may also be microcephaly, nasal changes, hypotrichosis, and skin pigment deficiency.
Treatment is surgical.
Mandibular-facial dysostosis (Franceschetti)
Mandibular-facial dysostosis (Franceschetti) is a syndrome that is familial and hereditary in nature, characterized by a variety of maxillofacial anomalies in various combinations. From the side of the eyes about the palpebral fissures, i.e. bilateral downward descent of the outer canthus. There are colobomas of the eyelids. Epibulbar dermoids, paresis of the extraocular muscles, rarely microphthalmos, congenital cataracts, colobomas of the vascular tract and optic nerve are observed. From the maxillofacial system, hypoplasia of the facial bones is observed. The cheek bones are small and underdeveloped and this leads to significant facial asymmetry. The zygomatic processes of the temporal bones may be absent, the body and branches of the jaw bones may be underdeveloped. Hypoplasia of the lower jaw, prognathism, and macrostomia are observed. Dental anomalies are characterized by underdevelopment of the teeth, primarily the molars, the teeth are widely spaced, there is often a malocclusion, and less commonly a cleft palate. Aplasia of the ears, false ears, fistulas between the corner of the mouth and the ear, hyperplasia of the frontal sinuses, underdevelopment of the maxillary sinuses, splitting of the facial bones and skeletal deformation are common. Hair grows low on the forehead, cheeks, sometimes partial alopecia. There may be enlargement of the tongue, absence of the parotid gland, internal hydrocephalus, damage to the heart, trachea and bronchi, cryptorchidism, mental retardation. Along with typical forms of the syndrome, there are also atypical ones, in which only part of the symptoms are present.
Treatment is surgical.
Nasociliary nerve syndrome
This syndrome is based on neuralgia of the nasociliary nerve. The nasociliary nerve is the largest branch of the first branch of the trigeminal nerve. The ethmoidal nerves (anterior and posterior) depart from it. The posterior ethmoidal nerve, as a sensory nerve, goes to the posterior ethmoidal cells, and the anterior one passes into the cranial cavity at the lamina cribrosa and through the anterior openings of this plate into the ethmoidal labyrinth and nasal bone. Here the nerve supplies the mucous membrane of the nasal cavity, then passes over the nostrils into the space between the cartilage and the nasal bone and supplies what is called n. nasalis externus skin of the nostrils, wing and tip of the nose. The other terminal branch, the supratrochlearis nerve (n. supratrochlearis), in the area of the upper inner corner of the orbit innervates the skin of the eyelids, forehead and root of the nose adjacent to this angle. It anastomoses with the frontal nerve. Through this anastomosis, sympathetic fibers from the plexus of the internal carotid artery penetrate into the frontal nerve, which supply the skin of the forehead area, within which the frontal nerve branches. The nasociliary nerve sends a branch to the ciliary ganglion, from which short ciliary nerves go to the eyeball. Long ciliary nerves depart from the trunk of the nasociliary nerve, which, without entering the ciliary ganglion, go to the eyeball. They, together with the short ciliary nerves, form plexuses in the region of the ciliary body and around the cornea outward from Schlemm’s canal. The branches of this plexus penetrate the cornea as sensory and trophic nerves. When the nasociliary nerve is irritated in the area of its branches, changes in sensitivity (pain), secretion disorders (lacrimation, increased secretion of the nasal mucosa) and trophic disorders (rashes on the skin and cornea) occur. The syndrome may not always be complete; it often occurs in “erased” forms. The disease is associated with hypertrophy of the middle turbinate, curvature of the nasal septum, and its spines. nasopharyngeal adenoids, polyps, sinusitis, mucocele and facial injuries. In the pathogenesis of the syndrome, common diseases syphilis, tuberculosis, diabetes, influenza, focal infection (dental diseases), as well as brain diseases of various etiologies are also important. Attacks of acute pain in the eye, around the eye, the corresponding half of the head and face, blepharospasm, lacrimation, copious discharge from the nose, on the affected side, occur suddenly. Patients also complain of a burning sensation and pain in the nasal mucosa above the nostrils, and in the area of the upper inner corner of the orbit. Herpes-type blisters may appear on the skin of the nose. On the part of the eyes there may be superficial, ulcerative or neurotrophic keratitis, iritis or iridocyclitis. The severity of eye symptoms and the intensity of pain often do not correspond. An attack can occur under the influence of irritation of the side wall of the nasal cavity or pressure on the wing of the nose at the exit site of the nasociliary nerve. An attack of pain can last 10-60 minutes, and sometimes patients cannot sleep for weeks and spend their nights sitting. An attack can also occur while eating.
The erased form includes facial neuralgia, which is expressed in periodically occurring orbital and periorbital pain that can last weeks, months and even years. Treatment consists of eliminating the underlying cause. Subjective symptoms are temporarily eliminated by lubricating the mucous membrane in the anterior part of the nose with a 5% solution of cocaine with adrenaline. Antibiotics, tranquilizers, sulfonamides, painkillers, sleeping pills, ganglion blockers, nasal electrophoresis with novocaine, atropine, platyphylline are used. Cases are described in which recovery occurred from antisyphilitic treatment and from sanitation of the oral cavity. The syndrome should be differentiated with damage to the pterygopalatine ganglion and other facial neuralgia.
Pterygopalatine ganglion syndrome (Slüder syndrome)
The pterygopalatine ganglion is the formation of the parasympathetic part of the autonomic nervous system. It contains multipolar cells and has three roots: the first - sensitive, the second - parasympathetic (greater petrosal nerve, carrying secretory fibers to the lacrimal gland, to the glands of the nasal cavity and palate), sympathetic (deep petrosal nerve, branch of the plexus caroticus internus, containing postganglionic sympathetic nerve fibers from the cervical ganglia). The branches of the pterygopalatine ganglion innervate the lacrimal gland, the mucous membrane of the hard and soft palate, a large area of the nasal mucosa, the posterior cells of the ethmoid bone and the sinuses of the maxillary and sphenoid bones. The anatomical structure of the pterygopalatine node explains the symptoms of the disease. The patient experiences sharp shooting pains at the base of the nose, around and behind the eyes, in the eye, in the upper and lower jaws, and in the teeth. The pain radiates to the temple, ear, parotid region, especially to the mastoid process. The pain may spread to the neck area. shoulder blades, shoulder and forearm, hands and fingertips. At the same time, there may be pain in the area of the hard palate and adnexal cavities. But it is most intense in the area of the orbit, root of the nose and mastoid process. The duration of pain ranges from several hours and days to several weeks. At the time of the attack, the patient also complains of a burning sensation and tickling in the nose, attacks of sneezing, runny nose, lacrimation, drooling, dizziness, and nausea. There may be asthma-like attacks and taste disturbances. Objectively, the eyes show severe photophobia, blepharospasm, swelling of the upper eyelid, conjunctival hyperemia, mydriasis or miosis, and sometimes a short-term increase in IOP. There may be slight exophthalmos. The disease can last for a long time, months or even years. In the interictal period, a dull deep pain may remain in the area of the upper jaw, root of the nose, or orbit, swelling of the affected half of the face, and increased sweating may remain. Therefore, some believe that this is not only neuralgia, but also ganglioneuritis. Neuralgia of the pterygopalatine ganglion is associated with perifocal infection (in the paranasal sinuses and oral cavity), with infection in various parts of the head (purulent otitis, cerebral arachnoiditis), with injuries and foreign bodies in the nose, with hypertrophy of the nasal concha or deviated nasal septum, with peritonsillar abscesses, allergies. General intoxications, viral and rheumatoid infections can also cause irritation of the pterygopalatine ganglion. The cause may also be jaw tumors. Unlike nasociliary nerve syndrome, when the pterygopalatine ganglion is affected, there are no anatomical changes in the anterior segment of the eyeball, since the branches of the pterygopalatine ganglion do not supply the eyeball, but innervate the nasal cavity and the floor of the orbit. Increased sensitivity of the nasal mucosa is concentrated in the posterior part of the nasal cavity, and not in the anterior, as with disease of the nasociliary nerve. When the pterygopalatine node is irritated, there are no areas of increased pain sensitivity and no rashes occur. It is necessary to differentiate with other facial neuralgia.
Treatment. During an attack, novocaine blockade of the pterygopalatine ganglion area is recommended. Treatment should be comprehensive and, first of all, aimed at eliminating the main cause of the disease. Painkillers, decongestants, corticosteroids, antibacterial drugs, ganglion blockers, anticholinergic drugs (Belloid, Bellaspon), physiotherapeutic procedures, massage of the sore half of the face, endonasal electrophoresis with novocaine, multivitamins, and biogenic stimulants are also prescribed. In old age, it is useful to prescribe antisclerotic and vasodilator drugs.
Ciliary ganglion syndrome (Hageman-Pochman)
The ciliary ganglion is located behind the eyeball from 12 to 20 mm, between the beginning of the external rectus muscle and the optic nerve. It has a long sensory root from the nasociliary nerve, a short motor root from the oculomotor nerve, and a sympathetic root from the sympathetic plexus of the internal carotid artery. 4-6 short ciliary nerves extend from the ciliary ganglion to the eye. Bypassing the ganglion, the long ciliary nerves go to the eye along with the short ones. The short ciliary nerves, being mixed, carry into the eye motor fibers from the oculomotor nerve for the ciliary muscle and sphincter of the pupil, vasomotor fibers of the sympathetic system for the intraocular vessels and sensory fibers of the trigeminal nerve for the uveal tract. Long ciliary nerves are distributed in the cornea as sensory nerves. There are motor sympathetic fibers going to the dilator pupil and partly to the ciliary muscle. The disease appears suddenly, at a young age and more often in women. Characterized by pain in the head and depth of the orbit. They can intensify with movement of the eyeball and with pressure on the eyeball in a posterior direction. The pain may radiate to the corresponding half of the head, temple, or back of the head. The pain lasts from several days to several weeks. There is unilateral mydriasis with preservation of the correct round shape of the pupil, absence of pupillary reactions to light and convergence, weakness or paralysis of accommodation, hyposthesia of the cornea. There may be swelling, irritation with bubble-like elevation of the corneal epithelium, and an incoming increase in ophthalmotonus. Rarely, optic neuritis occurs. The syndrome is usually one-sided and occurs in different ways. It may go away in 2-3 days, a week or later. Accommodation improves, the pupil slowly narrows, and the pupil reacts to light. Or it may stay for a long time. Paralysis or paresis of accommodation may persist for a particularly long time, which is sometimes the only indication of the process that has been suffered. There may be relapses.
The causes are inflammatory processes in the paranasal sinuses, teeth, infectious and viral diseases, trauma or contusion of the orbit, etc.
Treatment: sanitation of the paranasal sinuses, oral cavity, ganglion blockades, vitamin therapy, corticosteroids, pyrotherapy, diphenhydramine, retrobulbar novocaine (1.5 ml of 1% solution), local quinine with morphine, vitamin drops.
Share on social networks!
0
Symptoms
The pathology can be characterized by the following symptoms:
pain in the affected half of the face;- lacrimation;
- skin redness;
- swelling;
- excessive salivation.
Doctors diagnose ganglionitis by collecting anamnesis and assessing the overall clinical picture of the disease. This excludes other causes of symptoms.
Treatment methods
Treatment is carried out using the following drugs in complex therapy:
- painkillers;
- anti-inflammatory;
- antibacterial;
- ganglion blocking and antihistamines;
- lubricating the nasal mucosa with dicaine solution.
Physiotherapeutic agents, such as UHF therapy (a method of physiotherapy, which is based on the impact on the patient’s body of a high-frequency electromagnetic field with a frequency of electromagnetic oscillations of 40.68 MHz or 27.12 MHz), electrophoresis, DDT (electrophoresis of drugs with diadynamic currents - simultaneous impact on the body with diadynamic currents and medicinal substances introduced with their help), mud therapy.
Causes of the disease
The disease mainly begins to progress due to the penetration of infectious agents into the pterygopalatine node, which cause the development of the inflammatory process.
Sometimes ganglionitis of the pterygopalatine ganglion manifests itself as a neurodental complication of dental caries, which is accompanied by the development of pulpitis and periodontitis.
Pathology appears due to infectious diseases such as:
sinusitis;- chronic rhinitis;
- pharyngitis;
- arthritis of the temporomandibular joint;
- toxic effects on the nerve ganglion in chronic tonsillitis;
- chronic purulent otitis.
Factors contributing to the appearance of ganglionitis of the pterygopalatine ganglion:
- lack of sleep;
- overwork;
- stress;
- excessive consumption of alcoholic beverages;
- loud noise;
- dental caries;
- pulpitis and periodontitis, against the background of ARVI, herpes, tuberculosis, rheumatism, as well as in case of injury with damage to the pterygopalatine fossa.
Read also
Rehabilitation
Restoration of the body after diseases of the central and peripheral nervous system, operations on the brain and spinal cord, conditions after removal of the mammary gland due to a tumor, consequences...
Read more
Encopresis
Encopresis is a condition in which a person does not control or feel the urge to defecate, and also cannot control the act of defecation itself; Fecal incontinence significantly impairs the patient’s quality of life,...
More details
Consequences of traumatic injuries to the skull, spine, brain and spinal cord
Traumatic brain injuries, or traumatic brain injuries, are damage to the brain that impair brain function. Brain injuries are divided into two large groups - closed...
More details
Myositis
Myositis is a group of diseases characterized by an inflammatory process in skeletal muscles. Depending on the cause of the disease, there are several forms of myositis: Autoimmune…
More details
Gliomas
What is a glioma? Glioma is a neuroepithelial tumor, a type of tumor of the central nervous system, the source of growth of which is glial tissue. In turn, glial tissue (glia) ...
More details
General clinical picture
Ganglionitis is manifested by an attack of intense facial pain that occurs spontaneously. The pain is never limited to the area of the pterygopalatine node. It is localized in a variety of ways: in the eyeball, in the upper jaw, at the base of the nose, in the hard palate, in the area of the gums and teeth of the lower jaw, in the occipital region, neck, auricle, in the temporal region, less commonly appears in the shoulder, forearm, and sometimes even in the hands, and the pain can be localized throughout half of the body.
The duration of an attack of pain varies from several minutes to several hours, as well as several days. Most often, it is noticed that pain occurs at night. Ganglionitis is chronic and can last for years. An exacerbation was noted in spring and autumn, just at the time when seasonal diseases, such as acute respiratory viral infections and tonsillitis, become more active.
Treatment
The necessary drugs are injected directly into the nasal cavity with turundum with novocaine and the nasal cavity is lubricated with dicaine.
Severe pain is relieved with azamethonium bromide, benzohexonium, and there is also the option of using a blockade with lidocaine or novocaine.
Treatment of ganglionitis with infectious etiology is carried out by specialists using antibiotics and anti-inflammatory drugs. Hydrocortisone in this case showed very good results in the treatment of ganglionitis. The following antihistamines are mandatory:
chloropyramine;- loratadine;
- desloratadine;
- B vitamins.
You also cannot do without the following drugs:
antispasmodic;
- neuroleptics;
- antidepressants;
- anticholinergics.
- vascular and anti-sclerotic medications that improve cerebral and cardiac circulation.
Physiotherapeutic methods of treating ganglionitis include:
- UHF;
- DDT;
- endonasal electrophoresis of novocaine;
- mud therapy;
- massage of the muscles of the face and neck.
The patient can be examined by visiting the following specialists:
- neurologist,
- dentist,
- otolaryngologist.
These specialists will refer you for the following examinations:
- radiography of the skull;
- radiography of the tooth;
- radiography of the paranasal sinuses;
- otoscopy (examination of the external auditory canal, eardrum);
- pharyngoscopy (examination of the nasopharynx);
- UHF therapy;
- extracavitary diadynamic therapy;
- endonasal electrophoresis;
- peloidotherapy (mud therapy);
- fangotherapy (treatment with mineral mud of volcanic origin);
- algotherapy (algae treatment);
- pterygopalatine-orbital block.
Experts in the field of medicine have noted that complex treatment of ganglionitis of the pterygopalatine ganglion brings much more results and is the most effective method to combat this disease.
Patients and methods
105 patients, 61 men and 44 women aged 18 to 59 years, were examined. Patients included in the study underwent septoplasty with maximum preservation of the nasal septum skeleton in combination with submucosal ultrasound disintegration of the inferior turbinates. After the operation, layer-by-layer light nasal tamponade with hemostatic tampons was performed for 2 days. The patients were combined into four groups. Patients 1st ( n
=59) and 2nd (
n
=16) groups underwent surgery under general anesthesia;
hydraulic preparation of the perichondrium was performed with a 0.5% lidocaine solution with the addition of adrenaline hydrochloride 1:100,000. Patients of the 2nd group underwent bilateral blockade of the pterygopalatine ganglion. Patients of the 3rd ( n
=15) and 4th (
n
=15) groups underwent surgery under local anesthesia with a 1% lidocaine solution with the addition of adrenaline hydrochloride 1:100,000. Patients of the 4th group additionally underwent bilateral blockade of the pterygopalatine ganglion using the safest palatal approach. For a preliminary assessment of the individual anatomical features of the pterygopalatine fossa, the method of cone beam computed tomography (CBCT) was used [11].
Considering the length of the pterygopalatine canal, the maximum injection depth was 43 mm. For injection, a disposable 2 ml syringe with a disposable 0.42×88 mm needle was used.
The injection depth was consistent with the CT scan evaluation. Since the target of the injection was the pterygopalatine ganglion and not the maxillary nerve, 3 mm was subtracted from the calculated canal length. The average thickness of the soft tissues above the greater palatine foramen was taken to be 7 mm. Thus, during injection, the tip of the needle did not reach the level of the round hole by 10 mm.
To infiltrate the pterygopalatine fossa, a 2% lidocaine solution in a volume of 2 ml was used. About 0.5 ml of 2% lidocaine solution was used for superficial infiltration and injection of anesthetic as the needle was advanced.
The injection site, calculated based on the CBCT results, was palpated with a blunt instrument. A needle attached to a syringe was inserted into the greater palatine foramen and a small volume of anesthetic was injected. The required injection depth was marked on the needle with a piece of sterile latex. The needle was then slowly inserted to the set depth. During needle insertion, a small amount of anesthetic was aspirated three times. After reaching the desired depth, a slow injection of 2 ml of anesthetic was performed, after which the needle was removed.
Intraoperative bleeding was assessed in all operated patients. For this, we used a modified method of A. Boezaart et al. [12].
A visual analog pain scale was used to assess pain after surgery. The results of the survey on a visual analogue scale were recorded 1 hour after the patient was transferred to the ward from the operating room, during the morning examination on the 1st and 2nd days after surgery before removal of the nasal tampons.
To assess changes in the sympatho-vagal balance, we used the method of analyzing cardiointervals. In 5 patients from the 3rd and 5 from the 4th groups, the state of the autonomic nervous system was assessed before surgery by spectral analysis of heart rate variability after recording rhythmograms lasting 300 cardiointervals using the VNS-micro device connected to a personal computer with software "Neurosoft", using the fast Fourier transform with the selection of frequency spectra of different powers. High frequency waves (HF) at 0.15-0.4 Hz reflect the parasympathetic activity of the vagus nerve. Low frequency waves (LF) with a frequency of 0.04-0.15 Hz are an indicator of the activity of the sympathetic division of the autonomic nervous system. The LF/HF ratio is an indicator of the dynamic balance between segmental sections, reflecting the level of sympatho-vagal balance.
Statistical processing of research results was carried out using Wilcoxon, Mann-Whitney and Spearman tests.
Preventive recommendations
Treatment of this pathology can only prevent relapses due to the chronic course of the disease. So, if you have a predisposition to this disease, and in order to exclude ganglionitis of the pterygopalatine ganglion, you must adhere to the following points:
follow the necessary recommendations of doctors;- avoid stressful situations;
- drink a minimum of alcoholic beverages;
- limit contact with people who suffer from infectious diseases;
- carry out timely prevention of viral and infectious diseases during periods of mass disease (spring, autumn).
It is also necessary to put your sleep and wakefulness in order, as well as avoid overwork and heavy loads, and devote as much time as possible to rest and walks in the fresh air.
It is necessary to visit the dentist in order to avoid caries, pulpitis and other problems with the teeth and oral cavity. Avoid stressful situations. Reconsider your attitude towards the things that worry you most and react to stimuli more calmly; perhaps use antidepressants. In order to choose the right sedatives, you need to consult a doctor.
Diagnostics
Certain difficulties in making a diagnosis are explained by multiple QU connections with different structural branches of the nervous system.
In addition, it is necessary to take into account additional factors that can provoke spontaneous occurrence of HCU - stressful situations, alcohol consumption, smoking, overwork and hypothermia, sudden noise exposure.
The key sign of a specific diagnosis of the disease is the cessation of a HCU attack after treatment of the posterior sections of the nasal cavity with a weak solution of tetracaine with epinephrine.
The disease should be differentiated from trigeminal neuralgia, in which attacks are fleeting, their irradiation is not observed, “trigger zones” are present, and local lubrication with an anesthetic does not relieve symptoms.
For certain indications, the organization of collegial consultations with a dentist, rheumatologist, ophthalmologist, and otolaryngologist is encouraged.