Prognosis after ischemic, hemorrhagic
Cerebral hemorrhage usually occurs in a more severe form. The mortality rate in such patients reaches 70%; even after removal of the hematoma, the rate is not much lower. Unfavorable factors include:
- breakthrough of blood into the ventricles of the brain;
- uncontrolled arterial hypertension;
- large volume of hematoma;
- progressive cerebral edema;
- signs of displacement of the stem part;
- acute heart failure;
- increase in creatinine content in the blood;
- convulsive syndrome, lack of consciousness, reactions to painful stimuli for more than 3 days;
- age after 70 years.
With ischemic stroke, a more benign course is observed; it is rarely accompanied by a profound impairment of consciousness. This happens with repeated vascular accidents, massive blockage of the brain arteries with cholesterol plaques, lack of treatment or complete disregard of doctors’ recommendations.
Blockage of arteries in the brain
Precoma and the first degree of coma can still give the patient a chance for recovery; with a higher degree, the prognosis is considered doubtful, and the onset of extreme coma is usually regarded as fatal.
Forecast
It is impossible to say with complete certainty what prognosis awaits this or that person; it all depends on additional factors that existed before or after the coma. Let's consider the factors that can lead to the death of a patient:
- Creatine. With an increased concentration of creatine in the blood (up to 1.5 mg/dL), the chances of an unfavorable outcome increase.
- Severe convulsions that can remain intense and strong for up to three days or more.
- Complete loss of all reflexes, especially breathing and swallowing.
- Age. Naturally, the older a person is, the more difficult it is for him to get out of a comatose state. People whose age exceeds 70 years have virtually no chance of rehabilitation.
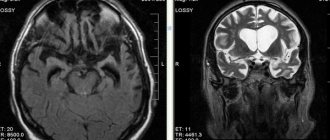
- Negative indications for magnetic resonance imaging (MRI) studies.
A fairly common occurrence in which coma gives way to a vegetative existence.
Positive prognoses depend only on the degree of damage to the brain and central nervous system (CNS), as well as on additional factors, let’s consider them:
- Information about the cause of the disease will have a positive impact on the quality of treatment, and therefore on the period of rehabilitation.
- Provide first aid.
- Compensatory ability of the central nervous system.
With a gradual recovery from a coma, the degree of brain damage can be determined. They can manifest themselves in the form of speech impairment, severe loss of sensitivity, loss of vision and other complications caused by the coma state.
Duration of coma
The duration of a coma can be very different: from several hours to several days or weeks. Some patients die without regaining consciousness. Rarely does a patient remain in a coma for several months, a year, or more. But the chances of recovery after such a long coma are extremely low.
A quick exit is more likely when:
- moderate area of necrosis;
- ischemic nature of stroke;
- partial preservation of reflexes;
- young age of the patient.
Prevention
The most important prevention of coma is the prevention of stroke. Prevention lies in the basic principles, let's look at them in detail:
Always worried about your health, you need to undergo regular medical examinations, and also adhere to the right lifestyle in order to avoid any complications or pathologies.
It is necessary to literally memorize the main symptoms of a stroke; it is worth mentioning that at the slightest suspicion you should immediately go to a specialist for advice.
As a result, we realized that stroke and coma are very related to each other. Coma is just a developed vegetative state. That is why rehabilitation depends on all extraneous factors that literally fall on a person. Coming out of a coma is possible, but it requires a lot of effort. We hope we were able to answer your question, how many days does a coma last and what to do about it.
What is coma and stupor?
Coma is a disorder of the central nervous system. A person has no consciousness, reflexes or reactions to external stimuli. There is a failure in all the most important life processes.
There are primary and secondary coma. The first occurs with focal brain damage. These could be injuries, tumors, apoplexy. The second is a consequence of some pathological process.
Stupor is one of the stages of coma. It is also characterized by depression of the central nervous system. The patient's reflexes are preserved, but he does not react in any way to the environment. In fact, stupor is an intermediate state between stunned consciousness and coma.
- On the verge of life and death: extensive cerebral stroke. What are the chances of survival?
Why do people fall into a coma?
The main reason for the development of coma after a stroke is cerebral hemorrhage or apoplexy. Several factors can provoke it:
- Heavy bleeding.
- Insufficient or completely absent blood circulation in the brain.
- Brain swelling.
- Atheroma. This is a disease associated with blood vessels.
- Poisoning with chemicals or other substances hazardous to the body.
- Callagenosis. Represents pathological changes in connective tissue.
- Angiopathy. This is a condition characterized by the accumulation of a specific protein in the blood vessels of the brain.
- Acute stage of vitamin deficiency.
- Infectious and autoimmune diseases of the circulatory system.
- Most often, the listed pathologies develop with hemorrhagic stroke.
Ischemic stroke very rarely leads to coma. Even if a coma does occur, the chance that a person will come out of it is great. In the hemorrhagic form, the death of brain tissue occurs, which entails serious complications.
Degrees of coma
Depending on how damaged the brain is after a stroke, there are 5 stages of coma:
Prekoma. This is a state when there is no coma yet, but brain functions are weakening. Its duration ranges from 2 hours to several days. The patient's consciousness is confused, his mood often changes, and coordination of movements is impaired. However, all the reflexes necessary for life are preserved. The body reacts to stimuli. A person feels touch.
Coma of the first degree of severity is considered to be stupor. It is characterized by lethargy, difficulties with communication and establishing contact, and increased muscle tone. The patient has difficulty eating. He can only eat liquid meals or drink water.
Second degree. Brain activity is greatly reduced. The patient does not respond to attempts to establish contact with him. However, there is a reaction to loud sounds and bright light (the pupils are constricted). Muscle tone either increases or decreases. Muscle fibers contract chaotically. Reflexes are also inconsistent. In some cases, spontaneous urination and defecation occur. Experts consider the second degree to be a borderline state.
The third degree is the coma itself. The person is in an unconscious state. He has no reaction to stimuli, reduced muscle tone, and muscle twitching is observed, for example, as a response to pain. The functioning of almost all organs and systems is disrupted. Blood pressure drops, heart rate decreases, and breathing slows down.
Treatment
Treatment is a complex, comprehensive process that must prevent death, maintain vital body functions, and at the same time combat the root cause of this condition.
The first resuscitation measures aimed at preserving a person’s life are carried out immediately upon the arrival of the ambulance team and during transportation of the patient, before all diagnostic procedures are carried out. First aid consists of fixing the patient's position, ensuring patency of the airway - straightening the tongue, clearing the nose and mouth of vomit, an oxygen mask, tracheotomy with the installation of a breathing tube. It is necessary to normalize blood circulation by administering medications that normalize cardiac activity and blood pressure. If necessary, indirect cardiac massage is performed.
In the intensive care unit, the patient is connected to an artificial respiration apparatus. Medicines are administered aimed at eliminating the pathological symptoms of the disease - anticonvulsants, antipyretics, hemostatics. Intravenous infusions of glucose and saline solutions are required. Measures are necessary to normalize body temperature. In case of hypothermia, the patient is covered and covered with hot water bottles. If there is a suspicion of poisoning with chemical or pharmacological drugs, gastric lavage is performed.
At the second stage, having detailed results of all types of examinations, the cause is eliminated. In case of hyperglycemic coma, measures are taken to normalize blood sugar and insulin levels. In case of renal failure, hemodialysis is performed. If an injury, hematoma or brain tumor is detected, urgent or planned surgical intervention is performed according to indications.
How does a person feel
There is no clear and uniform answer to the question of how a person feels while in a coma. But scientists have recorded brain activity when visiting relatives or changes in breathing and heartbeat when trying to communicate with a patient. Many relatives wonder: can a person in a coma hear them?
The people themselves who have experienced such an experience describe their sensations differently: some were conscious, but could not show it, some saw various dreams, and some communicated with deceased loved ones; there are also cases when patients couldn't remember anything.
How does nutrition occur in a coma?
The patient is provided with food enterally (through the gastrointestinal tract) or parenterally (intravenously) , and combined nutrition is also organized.
When using a probe, liquid and semi-liquid (cream-like) products are served. They go directly to the stomach . Dense dishes are ground and diluted taking into account the nature of the mixture - boiled water, tea, broth, vegetable decoctions, milk, juices and other components are used for this.
Parenteral nutrition involves the intravenous administration of nitrogenous drugs, energy substances , and saline solutions in quantities that are necessary to maintain the strength of a person in a coma. First, a daily infusion program is developed, which indicates the method and sequence of drug administration, as well as the volumes of solutions, the rate of infusion and the necessary drug additions. To monitor the patient's condition, control laboratory tests are regularly carried out.
How quickly do you recover from a coma?
- 3 months – active rehabilitation,
- the first 1-2 years – maximum rehabilitation,
- in the next 3 years, recovery occurs more passively.