Patients after a long coma are the most severe group, requiring long-term treatment and subject to persistent and long-term disability. Severe traumatic brain injury (TBI) is the most common cause of coma and post-comatose unconscious states (PLS), including vegetative states (VS) [1]. At the same time, post-traumatic genesis of PPS is the most favorable compared to other causes with regard to the prognosis of restoration of consciousness in this group of patients [2]. As the most common and favorable in terms of the prognosis for the restoration of consciousness, PPS of post-traumatic origin attract the attention of researchers in various specialties. Studying the characteristics of the restoration of brain functions in these patients makes it possible to more accurately diagnose various conditions and syndromes, plan rehabilitation measures, predict the outcome, and also better understand the neuronal mechanisms of such brain functions as consciousness.
Prognosis after ischemic, hemorrhagic
Cerebral hemorrhage usually occurs in a more severe form. The mortality rate in such patients reaches 70%; even after removal of the hematoma, the rate is not much lower. Unfavorable factors include:
- breakthrough of blood into the ventricles of the brain;
- uncontrolled arterial hypertension;
- large volume of hematoma;
- progressive cerebral edema;
- signs of displacement of the stem part;
- acute heart failure;
- increase in creatinine content in the blood;
- convulsive syndrome, lack of consciousness, reactions to painful stimuli for more than 3 days;
- age after 70 years.
With ischemic stroke, a more benign course is observed; it is rarely accompanied by a profound impairment of consciousness. This happens with repeated vascular accidents, massive blockage of the brain arteries with cholesterol plaques, lack of treatment or complete disregard of doctors’ recommendations.
Blockage of arteries in the brain
Precoma and the first degree of coma can still give the patient a chance for recovery; with a higher degree, the prognosis is considered doubtful, and the onset of extreme coma is usually regarded as fatal.
Anatomical and functional features of the central nervous system
Being the central regulator of all processes occurring in the body, the brain operates in an active metabolic mode. Its weight is only 2% of body weight (about 1500 g). However, for the uninterrupted functioning of the brain, 14-15% of the total volume of circulating blood (700-800 ml) must flow into and out of the cranial cavity every minute. The brain uses 20% of all the oxygen the body consumes. It is metabolized only by glucose (75 mg per minute or 100 g per day).
So, the physiological functioning of brain tissue depends on adequate perfusion with its blood, the content of a sufficient amount of oxygen and glucose, the absence of toxic metabolites and the free outflow of blood from the cranial cavity.
A powerful autoregulation system ensures smooth functioning of the brain. Thus, even with significant blood loss, the perfusion of the central nervous system is not impaired. In these cases, a compensatory reaction of centralization of blood circulation with ischemia of less important organs and tissues is activated, aimed primarily at maintaining adequate blood supply to the brain. The body reacts to another pathological condition - hypoglycemia - by increasing blood flow to the brain and increasing the transport of glucose here. Hyperventilation (hypocapnia) reduces blood flow to the brain; hypoventilation (hypercapnia) and metabolic acidosis, on the contrary, increase blood flow, promoting the removal of “acidic” substances from tissues.
With significant damage to brain tissue, insufficient autoregulation or excessive manifestations of the compensatory reaction of the inflow and outflow of blood, the brain cannot voluntarily change its volume. The closed cavity of the skull becomes its trap. Thus, an increase in intracranial volume by only 5% (with hematomas, tumors, hyperhydration, liquor hypertension, etc.) disrupts the activity of the central nervous system with the patient losing consciousness. In another pathology, excessive growth of cerebral blood flow leads to overproduction of cerebrospinal fluid. The brain tissue is compressed between the blood and the cerebrospinal fluid, swelling develops, and functions are impaired.
Traumatic destruction of brain tissue, edema and swelling, increased intracranial pressure, impaired circulation of cerebrospinal fluid, circulatory disorders and other damaging mechanisms lead to hypoxia of CNS cells. It manifests itself primarily as a disturbance of consciousness.
Duration of coma
The duration of a coma can be very different: from several hours to several days or weeks. Some patients die without regaining consciousness. Rarely does a patient remain in a coma for several months, a year, or more. But the chances of recovery after such a long coma are extremely low.
A quick exit is more likely when:
- moderate area of necrosis;
- ischemic nature of stroke;
- partial preservation of reflexes;
- young age of the patient.
Rehabilitation after a coma
To bring a patient out of a coma, doctors make many attempts, and this process takes an indefinite amount of time. If persistent efforts are successful, the person’s consciousness returns, the mood for recovery is formed, and rehabilitation is carried out under the supervision of specialists.
For this purpose, targeted centers with multifaceted rehabilitation programs are created. In the Minsk region, one operates in the Aksakov region. Those who require specialized assistance are there free of charge.
What is coma and stupor?
Coma is a disorder of the central nervous system. A person has no consciousness, reflexes or reactions to external stimuli. There is a failure in all the most important life processes.
There are primary and secondary coma. The first occurs with focal brain damage. These could be injuries, tumors, apoplexy. The second is a consequence of some pathological process.
Stupor is one of the stages of coma. It is also characterized by depression of the central nervous system. The patient's reflexes are preserved, but he does not react in any way to the environment. In fact, stupor is an intermediate state between stunned consciousness and coma.
- On the verge of life and death: extensive cerebral stroke. What are the chances of survival?
Why do people fall into a coma?
The main reason for the development of coma after a stroke is cerebral hemorrhage or apoplexy. Several factors can provoke it:
- Heavy bleeding.
- Insufficient or completely absent blood circulation in the brain.
- Brain swelling.
- Atheroma. This is a disease associated with blood vessels.
- Poisoning with chemicals or other substances hazardous to the body.
- Callagenosis. Represents pathological changes in connective tissue.
- Angiopathy. This is a condition characterized by the accumulation of a specific protein in the blood vessels of the brain.
- Acute stage of vitamin deficiency.
- Infectious and autoimmune diseases of the circulatory system.
- Most often, the listed pathologies develop with hemorrhagic stroke.
Ischemic stroke very rarely leads to coma. Even if a coma does occur, the chance that a person will come out of it is great. In the hemorrhagic form, the death of brain tissue occurs, which entails serious complications.
Degrees of coma
Depending on how damaged the brain is after a stroke, there are 5 stages of coma:
Prekoma. This is a state when there is no coma yet, but brain functions are weakening. Its duration ranges from 2 hours to several days. The patient's consciousness is confused, his mood often changes, and coordination of movements is impaired. However, all the reflexes necessary for life are preserved. The body reacts to stimuli. A person feels touch.
Coma of the first degree of severity is considered to be stupor. It is characterized by lethargy, difficulties with communication and establishing contact, and increased muscle tone. The patient has difficulty eating. He can only eat liquid meals or drink water.
Second degree. Brain activity is greatly reduced. The patient does not respond to attempts to establish contact with him. However, there is a reaction to loud sounds and bright light (the pupils are constricted). Muscle tone either increases or decreases. Muscle fibers contract chaotically. Reflexes are also inconsistent. In some cases, spontaneous urination and defecation occur. Experts consider the second degree to be a borderline state.
The third degree is the coma itself. The person is in an unconscious state. He has no reaction to stimuli, reduced muscle tone, and muscle twitching is observed, for example, as a response to pain. The functioning of almost all organs and systems is disrupted. Blood pressure drops, heart rate decreases, and breathing slows down.
Material and methods
For 2 years, 87 patients, 65 (74.7%) men and 22 (25.3%) women, aged from 16 to 75 years (average - 36.0±1.5 years) with prolonged post-traumatic coma were observed. In 8 (9.2%) patients, the level of depression of consciousness in the acute period of injury corresponded to a mild coma (coma I), in 79 (90.8%) - moderate (coma II). The duration of coma in all patients exceeded 7 days (on average 13.4±2.7 days).
Analysis of the clinical and neurological picture in patients after an episode of prolonged coma was carried out on the basis of the dynamics of vital functions, neurological status and the patient’s reactions to the presentation of external stimuli. VS was diagnosed taking into account the criteria of the Multisociety Task Force on Persistent Vegetative State (MSTF on PVS, 1994) [1]. The diagnostic criteria for VS were the lack of conscious perception of one’s own personality and the surrounding world, voluntary, purposeful movements, both spontaneous and in response to external stimuli, verbal expression and understanding of spoken speech; the presence of intermittent episodes of wakefulness observed during the sleep-wake cycle, preservation of the autonomic functions of the hypothalamus and brain stem to the extent that allows maintaining the patient’s vital activity during medical therapy, dysfunction of the sphincters, various variants of spinal and brain stem reflexes.
Low consciousness was diagnosed based on the Aspen Working Group criteria [3]. The criteria for its diagnosis were the patient’s execution of simple/monosyllabic commands (show tongue, open/close eyes, close/open mouth, etc.), verbal and gestural responses/reactions of the patient of the yes/no type (despite the accuracy of their execution), an episode of meaningful verbalization, simple reactions/answers of the patient, related in content to the presented tasks/stimuli and different from reflex ones (emotional reactions (smile/crying) in response to a corresponding visual or verbal external stimulus, but not an external stimulus of a neutral nature; purposeful movements; holding objects in a way/manner corresponding to the size and shape of the object; fixation and consistent movement of the gaze in response to addressing or approaching the patient). The listed clinical signs may not be constant, but they are necessarily reproducible.
A level of functioning of patients higher than “low consciousness” was determined based on the constant ability to functional interactive communication (through verbalization, writing, gesturing) and/or functional use of at least two everyday objects.
Dysautonomia was diagnosed when patients had at least five of seven criteria: tachycardia (more than 120 beats per minute), tachypnea (>30 breaths per minute), increase in muscle tone, appearance of decortication or decerebrate posture, arterial hypertension (BP system. more than 160 mm Hg), profuse sweating, hyper- (>38 ° C) or hypothermia.
How does a person feel
There is no clear and uniform answer to the question of how a person feels while in a coma. But scientists have recorded brain activity when visiting relatives or changes in breathing and heartbeat when trying to communicate with a patient. Many relatives wonder: can a person in a coma hear them?
The people themselves who have experienced such an experience describe their sensations differently: some were conscious, but could not show it, some saw various dreams, and some communicated with deceased loved ones; there are also cases when patients couldn't remember anything.
What causes coma?
The coma is caused by impaired blood circulation in the brain and/or toxic damage to the cells of the central nervous system. These pathologies arise for the following reasons:
- head injuries;
- drowning, suffocation, cardiac arrest;
- stroke;
- decompensated diabetes mellitus;
- meningitis, encephalitis;
- kidney or liver dysfunction as a result of poisoning or disease;
- epileptic seizures that follow one after another.
In addition, there is an artificial medical coma. It is used as an alternative to anesthesia if a neurosurgical operation is performed, as well as when the patient is brought out of an epileptic state.
Diagnostics
The diagnosis immediately establishes the causes of the comatose case. The conclusion differentiates the condition from other similar disorders of consciousness. The following diagnostic methods are used:
- Anamnesis collection. They find out from the patient's relatives or witnesses whether the patient took medications, and whether empty jars or blisters of medications were found nearby. You should ask about the presence of chronic diseases of blood vessels, endocrine glands, and heart. Clarify that the patient may have voiced complaints. An important factor is the age of the patient and the speed of development of symptoms. Young people more often fall into this state after poisoning with sleeping pills or narcotic drugs. In elderly patients, the formation of a coma occurs against the background of heart attacks, strokes, and other cardiovascular diseases.
- Inspection. During the examination, the possible root cause of the coma is determined. Respiratory rate, pulse rate, blood pressure, body temperature, injection marks, bad breath, bruises are indicators on the assessment of which the establishment of a correct diagnosis depends.
- The patient's position can also characterize the severity of brain damage. During hemorrhages and meningitis, the patient’s head is thrown back, the neck muscles have a pronounced tone - signs of irritation of the meninges. Convulsive attacks, cramping spasms of individual muscles indicate the patient’s status epilepticus, the condition of eclampsia in pregnant women. Unexpressed paralysis of the limbs indicates a stroke, a complete absence of reflexes indicates deep lesions of the cortex and spinal cord.
- A differential feature distinguishing it from other disorders of consciousness was the study of the patient’s function to open his eyes to irritation in the form of sound or pain. If the response to sound and pain stimulation in the form of involuntary opening of the eyes persists, then this is not a coma. If the eyes remain closed, the case is considered comatose by doctors.
- The doctor carefully evaluates the ability of the pupils to respond to light. Its quality makes it possible to determine the damaged area of the brain, and also indicates the factor that provoked the coma. The clarity of the pupil's reaction to light indicates the future prognosis of the disease.
Pinpoint pupils that do not respond to bright light indicate alcohol or drug poisoning. If the pupils of the left and right eyes have different diameters, this is a sign of increasing intracranial pressure. Excessively wide pupils are a symptom of midbrain pathologies. If, when exposed to bright light, the reaction of the pupils is completely absent, their diameter remains wide, this is a very unfavorable symptom, which indicates imminent brain death.
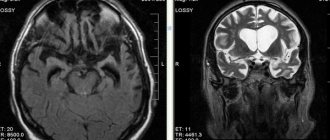
The development of medicine makes it possible to use hardware methods for diagnostic purposes to examine patients with impaired consciousness immediately upon admission to a medical institution. Performing head computed tomography (CT), magnetic resonance imaging (MRI) makes it possible to detect changes in areas of the brain, lesions, tumor-like neoplasms, and signs of intracranial hypertension. The conclusions obtained as a result of the tomograph study serve as the basis for determining treatment tactics - surgical or conservative.
X-rays of the head and spine in several projections are performed if MRI or CT is not possible.
A biochemical blood test can confirm a metabolic failure. Tests for the level of glucose, urea, acetone, and ammonia in the blood are carried out very quickly. The ratio of the content of electrolytes and blood gases is determined. In addition, the blood is examined for insulin levels, adrenal and thyroid hormones, for the presence of narcotic substances, tranquilizers and other toxic drugs, and bacterial blood cultures are performed to identify a possible infectious agent.
During an electroencephalogram (EEG), electrical impulses from the brain are recorded, which make it possible to determine the type of coma and understand what caused it - hemorrhage, poisoning or a tumor.
Rehabilitation period
Not all cases of impaired consciousness require a long rehabilitation period. According to statistics, recovery from a coma caused by diabetes, high doses of drugs or alcohol does not last long. In such cases, impaired consciousness is present before the toxic substance is eliminated from the body.
Coming out of a 3rd degree coma after a TBI or 1st degree equally requires rehabilitation measures. First of all, measures are taken to restore brain function. Not in every case, amnesia develops, but there is a deterioration in memory and attention.
How do you recover from a coma after a TBI? During this period, the ability to sit and walk without assistance and available means is lost. Confusion of consciousness is observed, the person loses orientation in space. The following specialists help correct such disorders caused by prolonged impairment of consciousness:
- neurologist (helps restore speech);
- psychologist (normalizes the psycho-emotional state);
- occupational therapist (helps improve motor skills);
- neurologist, physiotherapist, etc.
When recovering from a coma after a TBI, there is no need to immediately subject the patient to physical and mental stress on the first day. Rehabilitation should take place gradually. How many months or years it will take to fully restore the activity of the central nervous system, and what the prognosis will be, depends on the severity of the traumatic brain injury.
Rehabilitation after a coma consists of assisting the patient in all everyday activities: eating, going to the toilet and showering. Developmental games are required to help restore motor skills, memory, and speech. It is important to normalize your diet so that it includes all useful vitamins and microelements.
To restore muscle tone, massage procedures are prescribed, which are carried out in a specialist’s office and subsequently at home. During the massage, you can use any essential oil. The procedure also helps improve blood circulation. The main condition is continuity of therapy, even if the first positive changes are visible.
When to see a doctor
If a person falls into a coma, you should immediately consult a doctor. There can be no exceptions here. First of all, the patient will need the help of a resuscitator who will try to quickly remove the patient from the pathological condition. If resuscitation measures have no effect, treatment of the patient must be started.
Which specialist will treat the patient depends on the cause that caused the disturbance in the state of consciousness. You can seek qualified medical help at our clinic. We have specialists who understand how to work with people who have fallen into a coma. The choice of a doctor who will treat coma in the Central Administrative District depends on the cause that led to the development of the pathology.
Signs of third degree coma during stroke
This condition has its own distinctive features:
- Lack of response to pain.
- The pupils do not respond to light stimuli.
- Lack of swallowing reflex.
- Lack of muscle tone.
- Reduced body temperature.
- Inability to breathe independently.
- Bowel movements occur uncontrollably.
- Presence of seizures.
As a rule, the prognosis for recovery from a third-degree coma is unfavorable due to the absence of vital signs.
How to call a resuscitator
If you decide to go to our clinic in the center of Moscow for medical help, dial the ambulance number -. A team of our specialists will arrive at the address you specified to transport the patient to a medical facility and provide him with first aid.
All our specialists are highly qualified and have extensive medical experience. All diagnostic measures are carried out promptly. This is also due to the availability of modern equipment. Our doctors choose the most optimal treatment method, taking into account the characteristics of the disease and the patient’s body.
Our clinic is located at the address: Moscow, Central Administrative District, 2nd Tverskoy-Yamskaya Lane, building 10. The nearest metro station is Mayakovskaya (5 min walk).
Remember that if a person falls into a coma, he requires emergency assistance from specialists. The slightest delay can lead to the death of the patient.