Myelitis is an inflammation of the spinal cord, which is most often localized in the lumbar and sacral regions. The disease is usually accompanied by a significant weakening of sensory, motor and trophic functions. Inflammation of the spinal cord often occurs in parallel with inflammation of its membranes (meningomyelitis). These conditions are very similar, so it is sometimes very difficult to establish the exact geography of inflammation.
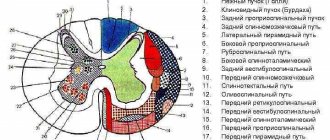
Myelitis can develop differently - locally, affecting only one segment of the spinal column, or diffusely - in more severe cases of the disease. Capture of half the diameter of the spinal cord by the pathological process leads to the development of Brown-Séquard syndrome - a circulatory disorder of the artery supplying one half of the spinal cord.
Myelitis is divided into primary, caused by damage to the spinal cord by viruses (canine plague), and secondary - complications of general infectious diseases (septicemia, sepsis, discospondylitis).
Traumatic myelitis – complications after spinal fractures. Myelitis caused by displacement of intervertebral discs.
Toxic myelitis is caused by severe poisoning.
In cases of myelitis, macroscopic examination of the spinal cord shows its laxity and vascular reactions. Microscopically - swelling of the membranes and substance of the brain, minor hemorrhages, infiltrative reactions, vascular necrosis, cell death. Changes usually also affect the membranes and roots, in this case we can talk about meningoradiculomyelitis.
Depending on the location and extent of the process, various symptoms are observed: tetraplegia, spastic paraplegia, Brown-Séquard syndrome, etc. Necrotizing myelitis gives a picture of a transverse break of the spinal cord involving several segments or sometimes the spinal cord along its entire length.
Symptoms
Symptoms of the disease manifest themselves in different ways and depend on the location of the inflammatory process and the causes of its occurrence. When an animal becomes ill with myelitis as a result of a viral infection, it becomes restless and squeals in pain when moving. At the same time, the muscles of the limbs are tense, trembling, twitching and convulsions are manifested. The dog's gait becomes unsteady, the animal quickly gets tired and often lies down. Cardiac and respiratory arrhythmias, involuntary urination and bowel movements appear. Paresis and paralysis occur, leading to the development of bedsores and muscle atrophy.
With traumatic myelitis, at the onset of the disease, paralysis of the hind limbs is observed, swimming movements appear, and the dog is predominantly in a sitting position.
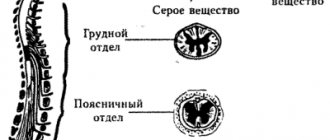
When the cervical spine is affected, paralysis of the muscles of the trunk and all extremities occurs, lethargy and weakness of the skin behind the pathological focus; When the thoracic region is damaged, shortness of breath, paralysis of the hind limbs and loss of sensitivity of the skin behind the damage to the spinal cord appear. Pathological processes occurring in the lumbar region cause paralysis of the hind limbs, bladder, rectum and anal sphincter.
Diagnosis of myelitis:
- neurological examination;
- cerebrospinal fluid examination;
- myelography;
- magnetic resonance and computed tomography;
- visual assessment of the spinal cord during surgery;
- cytological examination;
- histology.
A neurological examination determines:
- degree of neurological disorders;
- localization of the lesion.
Determining the degree of neurological disorders is important for the prognosis of the disease.
According to our data (more than 100 animals), in dogs that had 2-3 degrees of neurological disorders, recovery of spinal cord function is possible up to complete. Patients with grade 4 neurological disorders also have a chance to restore spinal cord function. In these dogs, complete recovery of the spinal cord usually does not occur; however, motor function of the limbs may be restored to almost normal. Dogs with grade 5 neurological disorders, with transverse spinal cord lesion syndrome, especially if we are talking about flaccid paralysis, have no chance of restoring spinal cord function.
It is important to determine the location of the lesion. If the damage is limited to 5–10 segments and the degree of neurological disorders is 2–4, then you can count on restoration of spinal cord function partially or completely. When 10–20 segments were affected, we did not observe complete recovery. In such animals, necrotizing myelitis (myelomalacia) with transverse brain lesion syndrome was observed.
Spinal fractures
The vertebrae have great strength and can withstand a lot of pressure, while at the same time the spine does not lose flexibility. But like other bones in the body, they can break under extreme excess pressure, injury or disease. In such cases, damage or fractures to the vertebrae can range from minor to severe.
Compression fractures
As the name suggests, compression fractures occur from excessive axial loads that compromise the integrity of the vertebral body. Osteoporosis is one of the leading causes of compression fractures, as there is a decrease in the ability of the vertebrae to withstand stress. In such cases, even a slight fall or even a cough can lead to a compression fracture. People often perceive back pain as a normal part of aging, and sometimes compression fractures go unnoticed. Repeated compression fractures can lead to a decrease in spinal height. Another common cause of a compression fracture is trauma, such as a fall.
Often, vertebral compression fractures will eventually heal on their own (without treatment). NSAIDs (for example, aspirin) may be prescribed to relieve pain. For severe fractures, surgical methods (vertebroplasty and kyphoplasty) may be used.
Burst fractures
Blowout fractures usually occur after severe trauma (for example, a car accident or a fall from a height). Blast fractures are significantly more dangerous than compression fractures because the anterior and middle portion of the vertebral body is fractured into multiple fragments and is more likely to result in spinal cord injury. Additionally, as the vertebral body loses its integrity, the spine becomes unstable. In some cases, with burst fractures, if there is no impact on the spinal cord, conservative treatment can be performed. If there are loose fragments or damage to the nerve structures, then surgical treatment is necessary.
Flexion-extension fractures
Such fractures are sometimes called Chance fractures and occur during sudden flexion-extension. Most often, this type of injury occurs in car accidents, in people wearing a seat belt, and not only fractures of the vertebrae, but also ligaments, discs, and sometimes internal organs. Such fractures are usually unstable and require surgical treatment. This type of fracture occurs in 5-10% of cases of spinal fractures.
Vertebral fracture with dislocation. Such fractures occur when exposed to great force, and not only the integrity of the vertebral body is violated, but also its displacement (due to rupture of ligaments and discs). Such fractures often require surgical intervention.
Fractures are also divided into stable and unstable. Compression fractures are generally considered stable and do not require surgery. In contrast, unstable fractures (eg, burst or Chance fractures) typically require surgical treatment, often as an emergency.
CSF examination
According to the literature, primary diseases of the central nervous system rarely lead to changes in a general blood test and biochemical analysis of serum, and if they exist, this indicates the likelihood of systemic disorders and secondary diseases of the central nervous system (Willard M. D., Tvedten H., Turnald GH, 1999). Therefore, in our practice, we perform a cerebrospinal fluid analysis even in the absence of abnormalities in blood tests before performing myelography.
In the cerebrospinal fluid sample, the physicochemical properties (color, transparency, protein content, glucose) are determined, and the cellular elements in the Goryaev chamber (erythrocytes and nuclear cells) are counted. Next, the cytogram in the stained preparation must be analyzed (May-Grunwald staining) to determine the content of each type of cell.
Normally, cerebrospinal fluid is transparent and colorless, the albumin content is 0.1–0.3 g/l, the number of cells does not exceed 5 cells per μl. The cytogram is scanty; single erythrocytes and mononuclear cells can be detected. The liquor is sterile.
With meningitis, turbidity of the cerebrospinal fluid is observed, accompanied by pleocytosis (increased content of cellular elements). In our studies, during acute inflammatory processes of the central nervous system, the protein concentration in the cerebrospinal fluid exceeded 100 mg% (1 g/l), cytosis - from 25 to several thousand nuclear cells per μl. Neutrophilic leukocytes predominate in the cytogram; microflora (usually coccal) is often detected. When the inflammatory process subsides, the number of cellular elements is often quite normal, the protein content may be normal or slightly increased, but, as a rule, does not exceed 3 g/l. In this case, the cytogram is represented by neutrophils, lymphocytes, and macrophages. In meningitis of viral etiology, the cerebrospinal fluid is usually clear, the protein content is slightly increased (up to 100 mg%), cytosis is 10–500 cells per μl, and mainly lymphocytes/mononuclear cells are present.
It should be noted that the cerebrospinal fluid is in direct contact with the membranes of the brain, therefore it more reflects the intensity of the inflammatory process of the membranes. In this regard, with deep disorders of the spinal cord parenchyma and the absence of damage to the membranes, analysis of the cerebrospinal fluid may not reveal significant abnormalities.
Rice. 1. Liqueur for purulent myelitis. Rice. 2. Swelling of the spinal cord in a Staffordshire Terrier due to myelitis. Block of liquor pathways in area C2. The cause of myelitis was chronic bacteremia, which in turn could be caused by impaired liver function. This dog was diagnosed with liver cirrhosis. After treatment for 3 years, no signs of spinal cord damage were observed.
Rice. 3. Repeated (in a week) myelography of the Staffordshire Terrier after the course of treatment. At the time of myelography, clinical manifestations of improvement were not observed. Recovery of spinal cord function occurred within 1.5 months.
Osteochondrosis
Over time, the spine is subjected to daily stress and minor injuries, which ultimately leads to wear and tear of the intervertebral discs and their degeneration. The fibrous ring of the intervertebral disc is damaged under load, micro-tears of fibrous tissue occur, and then the damaged area is replaced by scar tissue, the elastic properties of which are much worse than those of fibrous tissue. Such changes in the annulus fibrosus lead to decreased shock-absorbing function of the disc and a greater risk of recurrent disc ruptures. As the annulus fibrosus becomes scarred, the gelatinous part of the disc (nucleus) also gradually shrinks, which in turn leads to a decrease in disc height. As the height of the disc and shock-absorbing functions decrease, the vertebrae begin to exert more pressure on each other under load, which leads to the formation of bone growths (osteophytes). Violation of the integrity of the fibrous ring leads to the formation of disc herniations. Disc herniations and osteophytes can cause compression or stenosis, leading to neurological symptoms.
Myelography
According to the literature, “in all doubtful cases of acute and chronic myelopathies, myelography data play a significant role...” (Bersnev V.P. et al., 1998)
Before myelography, all animals were administered antibiotics and methylprednisolone at a dose of 30 mg/kg. Thanks to myelography, it is possible to accurately assess the size of spinal cord edema. Sometimes this test can reveal the cause of myelitis in cases where myelitis developed as a complication of instability or as a result of compression of the spinal cord by an intervertebral disc or tumor. It is necessary to begin myelography with atlanto-occipital puncture. At the same time, a sample of the cerebrospinal fluid is taken. If the contrast does not penetrate the thoracic and lumbar spine, a lumbar puncture is mandatory to contrast the entire subdural space, even if it seems that the diagnosis is obvious. From our experience, the following sequence of punctures is important: first, the atlanto-occipital one is performed, and then the lumbar one. This is due to the fact that with myelitis, significant swelling of the spinal cord develops, this causes a decrease in the subdural space, which makes it impossible to obtain cerebrospinal fluid. With atlanto-occipital puncture, it is almost always possible to obtain cerebrospinal fluid, even if the cervical spine is affected. The study of cerebrospinal fluid in myelitis can be crucial.
Visual assessment of the spinal cord during surgery can be decisive in some cases. When performing a hemilaminectomy or laminectomy with significant swelling of the spinal cord, a durotomy must be performed. After opening the dura mater, in some cases the spinal cord leaks out. In this case, we can talk about the impossibility of restoring the spinal cord. To confirm necrotizing myelitis, an imprint can be taken for cytological examination.
Herniated disc
A herniated disc occurs when the annulus fibrosus that surrounds the intervertebral disc ruptures. This rupture causes the central portion of the disc, which contains a substance called nucleus pulposus, to be released. When pressure is applied to the vertebrae above and below, the nucleus pulposus comes out, puts pressure on nearby nerve structures and causes severe pain and nerve damage. Disc herniations most often occur in the lumbar spine and are sometimes called disc extrusion.
MRI for myelitis
The diagnosis of myelitis and myelomalacia is important for prognosis. Transverse myelitis refers to diseases characterized by the rapid development of symptoms of spinal cord damage. On MRI in the acute stage, some thickening of the spinal cord may be observed in size with the identification of an intramedullary area of increased signal on T2-weighted MRI, usually involving several segments of the spinal cord. Late in the process, MRI reveals descending spinal cord atrophy
Causes of pathology
Disturbance of the spinal circulation can be caused either by compression of the vessels supplying the spinal cord (at any part of the blood flow), or by damage to the vascular system of the spinal cord. Among the most common reasons are:
● congenital pathologies. These include: aneurysm (protrusion of the artery wall), malformation (pathological connection between arteries and veins), hypoplasia (impaired development of blood vessels);
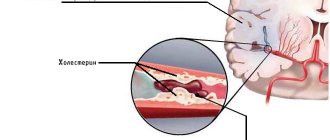
● acquired pathologies. These include: atherosclerosis (accumulation of cholesterol and fats on the artery wall), vasculitis (inflammation of blood vessels);
● neoplasms (benign and malignant) of the spinal column;
● abnormalities of the endocrine system (obesity of any type);
● degenerative-dystrophic lesions of the spinal column (hernia, osteochondrosis);
● toxic vascular lesions;
● vegetative-vascular dystonia:
● hemodynamic disorders (for example, a persistent decrease in blood pressure);
● oxygen starvation;
● compression lesions (in particular, surgical interventions);
● blood diseases (anemia, leukemia).
Assessment of the condition in traumatic myelitis
– Objective assessment of the severity of spinal cord injury in post-traumatic myelitis is difficult. Neurological disorders in the acute period are primarily caused by spinal shock. Spinal shock is characterized by the reversible nature of neurological disorders that occur in the acute and early periods of injury. It has also been established that the depth and duration of spinal shock depends on the severity of the injury; its manifestations are most pronounced in areas adjacent to the source of damage.
– In more severe trauma with crushing of the spinal cord, necrosis spreads over the entire diameter and several segments of the spinal cord, and may be accompanied by rupture of its membranes. Compression of the cerebrospinal fluid pathways, vessels and the spinal cord itself aggravates the course of the traumatic disease and contributes to the development of traumatic myelitis.
– Neurological examination on the first day does not provide a true picture of the damage, although the presence of symptoms of damage to lower motor neurons, as well as the presence of symptoms of transverse spinal cord injury, should alert the attending physician and may serve as a sign of an unfavorable prognosis.
– In the early period, neurological examination may be more objective; the progression of neurological disorders indicates the development of myelitis. Neurological examination can reveal lesions in other parts of the spinal cord. As a rule, with traumatic myelitis, a significant area of the spinal cord is captured, up to the involvement of the entire spinal cord and its membranes in the pathological process.
– And, of course, MTR can provide the most objective data on the degree of spinal cord destruction.
– Along with neurological examination, contrast myelography plays an important diagnostic role in traumatic myelitis. Carrying out this study helps to assess the size of the spinal cord edema along its length, the presence of spinal fragments causing compression of the spinal cord, which, in turn, significantly influences the choice of treatment. If fragments causing compression are present, surgical treatment is necessary.
| Rice. 4. Traumatic myelitis in a kitten after a fall. Block of cerebrospinal fluid in the thoracic region. Rice. 5. Ascending myelomalacia. Rice. 6. At autopsy - liquefaction of the entire spinal cord. |
Radiculopathy
The term radiculitis (radiculopathy) is widely used and means root compression. Radiculitis can occur in both the lumbar and cervical spine, or much less frequently in the thoracic spine. Root compression occurs when there is excess pressure on the nerve root. Excessive pressure can come from both bone tissue and soft tissue (muscles, cartilage, ligaments). This pressure disrupts nerve function, causing pain, tingling, numbness, or weakness.
Osteoporosis is a disease in which bone tissue, including the vertebrae, weakens, which increases the risk of vertebral fracture, even with minor loads. Vertebral compression fractures are the most common type of fracture caused by osteoporosis, and hip and wrist fractures are also possible with osteoporosis. These vertebral fractures can change the shape and strength of the spine, especially in older women, who often develop spinal deformity as a result of such fractures. The spine becomes excessively tilted in the thoracic region (kyphosis) and the shoulders bulge forward. With severe osteoporosis, even simple movements such as bending forward can lead to vertebral fractures.