Nootropics are neurometabolic stimulants that have a positive effect on complex psychophysiological processes. The mechanism of their action is associated with the restoration of the bioenergetic and metabolic functions of the neuron, as well as the neurotransmitter systems of the brain. The principle of operation of nootropic drugs, as their name suggests, is aimed at improving the functioning of the parts of the brain that are responsible for learning, memory, attention and other cognitive functions.
Nootropic drugs are drugs containing organic or synthetic active substances, as well as their derivatives, which stimulate the functioning of neurotransmitters. They are grouped into a pharmacotherapeutic group with the ATX code N06BX (“Other psychostimulants and nootropic drugs”).
The term nootropics was coined in 1972 by Romanian chemist, psychologist and Ph.D., Corneliu E. Giurgea, who first synthesized piracetam in 1964. Its therapeutic effect turned out to be the opposite of the chemist's expectations - characteristic of psychostimulants, without the occurrence of non-core actions. This effect still remains a mystery to scientists.
Nootropics used in medicine today are presented in the international drug classification system (Anatomical Therapeutic Chemical, ATC), adopted by the Ministry of Health of the Russian Federation in 2002. Other nootropic drugs are created for use within specific countries and are not introduced into the international market.
Clinical use of nootropics
Psychiatrists and psychotherapists can prescribe nootropic drugs either as monotherapy or in combination with other psychotropic drugs. For example, nootropics are prescribed for the treatment of neuroses, attention deficit hyperactivity disorder (ADHD), depressive disorders and other mood disorders, and schizophrenia.
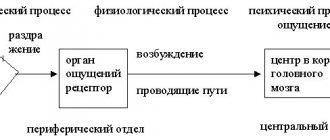
The purpose of prescribing nootropic drugs is to restore the cognitive functions of the brain responsible for the processes of interaction with received information, in particular:
- perception (information, - approx., etc.);
- processing;
- analysis;
- memorization;
- storage;
- correlations;
- conclusions.
Nootropic drugs are also used in other areas of clinical medicine. For example, in pediatrics, where nootropics help restore amino acid deficiency that disrupts protein biosynthesis in the body and metabolic processes in general. In particular, a doctor can prescribe nootropics for children with signs of delayed speech and mental development, mental retardation, and the consequences of perinatal damage to the central nervous system. Doctors of other specializations (speech therapists, neurologists, endocrinologists, gynecologists, urologists, ophthalmologists) can prescribe nootropics depending on the symptoms, including in complex therapy, for various diseases and conditions:
- neuroleptic syndrome;
- stuttering, logoneurosis;
- hyperkinesis, dyskinesia;
- urinary disorders;
- insomnia and other sleep disorders;
- headaches of various etiologies;
- dizziness;
- seasickness;
- open-angle glaucoma;
- vascular diseases of the retina;
- macular diseases;
- diabetic retinopathy;
- Alzheimer's disease;
- Parkinson's disease;
- Huntington's disease;
- with the consequences of TBI.
In other words, the range of use of nootropic drugs is wide and is not limited only to mental disorders. The gentle therapeutic mechanism of drugs in this group allows nootropics to be prescribed to newborns and infants, as well as the elderly. It is also important that nootropic drugs are included in the List of vital and essential drugs for medical use.
What nootropics (list of drugs and their characteristics) are widely used in pediatrics?
First of all, I would like to remind you that nootropics in pediatrics have fairly clear indications for use. These are, first of all, the following conditions: • Prevention and treatment of child retardation in mental, motor and speech (after 3 years) development. • Stimulation of central nervous system functions associated with the processes of learning, concentration, memorization and reproduction of information. • Organic damage to the central nervous system as a result of neuroinfections, traumatic brain injuries, genetic diseases. • Cerebral palsy. • Urinary disorders of neurogenic nature. • Stuttering. • Complex therapy of epilepsy. • Neurotic conditions and asthenia (obsessive-compulsive disorder) • ADHD – attention deficit hyperactivity disorder. Most often, children are prescribed nootropics from the list of so-called true nootropics, which primarily affect the mnestic (memory) and cognitive (cognitive) abilities of a person of any age. These are nootropic drugs such as: • Racetams. • Neuropeptides. • Cholinergic nootropics. • Neuroprotectors. • Activators of amino acids and GABA (gamma-aminobutyric acid). • Antioxidants. Of the Racetams, the most significant and widespread is Piracetam - a drug used by doctors for almost 50 years and being the founder of nootropic drugs, the list of which is constantly expanding and updated. Known under the commercial name nootropil. In children, it is especially effective as a stimulator of speech development, and also helps well with cerebral palsy and mental retardation, during rehabilitation after TBI and GM intoxication, and helps increase learning ability. Available in a wide variety of pharmacological forms - tablets, granules, capsules, syrups, solutions for parenteral administration. Peculiarities of use: not recommended for use in the afternoon.
In childhood, drugs such as: • Cortexin, which is considered the best for children 1 year of life, are also often prescribed. It can be used starting from the first birthday. It has a positive effect on the nervous system, including the peripheral one, counteracts toxic effects, improves blood circulation, and is used in the complex treatment of epilepsy. In addition, cortexin improves memory, increases resistance to stress and is effective when taken by children with developmental delays (psychomotor and speech). Quite popular among students, especially during sessions, to improve memory and assimilate large amounts of information. Cortexin also has positive reviews from parents and pediatricians; it is quite safe, but quite expensive. Available in the form of a lyophilisate (powder dried at sub-zero temperatures). • Semax 0.1% solution is the safest and is produced in the form of nasal drops convenient for use in children. It has virtually no side effects, except for rare and minor irritation of the mucous membrane. It belongs to the peptide series of nootropics and has a positive effect on attention, learning and perception. In addition, it helps restore and adapt the nervous system after anesthesia. In pediatrics, it has proven itself well in the treatment of brain dysfunction in children over 5 years of age. The advantages of Semax include high safety and a convenient release form for use. A relative disadvantage is the need to store the drug in the refrigerator at a temperature not exceeding 8 degrees.
• Cerebrolysin, which is a neuropeptide of animal origin (a concentrate of peptides from the brain of pigs or cattle. It is actively used as an activator of neural metabolism, helps to increase concentration and reduce hyperactivity. Its disadvantage is that it is a relatively expensive drug and is produced only in in the form of injection solutions, and the plus is that this is one of the most effective nootropics for developmental delays in children.Side effects are rare and boil down to individual allergic reactions to the components of the drug, insomnia and, extremely rarely, arrhythmias.
For delayed speech development (DSD), the following nootropics are also effective: • GABA analogues and derivatives (Picamilon, Pantogam), which normalize the conduction of nerve impulses and improve glucose utilization and oxygen consumption in neurons. Being inhibitory mediators, they are effective for hyperactivity and increased excitability of the central nervous system. • Pyritinol drugs (Encephabol, Cerebol), which have a neuroprotective (stabilization of membranes and inhibition of the production of free radicals that destroy the structure of cells) and antihypoxic effects. • Ceraxon is a stimulant of central nervous system activity, containing citicoline, which is responsible for restoring neuronal membranes and their energy supply, as well as reducing the amount of intercellular fluid in the brain and thus providing an anti-edematous effect. It is recommended not only for mental retardation with symptoms of inhibition, but also for autism. To summarize the answer to this question, I would like to say that the choice of nootropic drugs, the list of which, taking into account the new generation drugs, includes more than a hundred items, remains with the pediatrician. Under no circumstances should you prescribe nootropics on your own, even based on the indications indicated in the instructions. Of course, nootropics are quite safe drugs that have a positive effect on the nervous system, but each of them has its own preferential effect and is aimed at different processes in the nervous tissue. By independently prescribing CNS activators to a small patient with hyperactivity, parents can get increased activity and increased excitability in their child, leading him to a nervous breakdown and treatment by a child psychiatrist. To prevent such excesses, the vast majority of nootropics are sold in pharmacies only with a doctor’s prescription. Some of them can be purchased without a prescription, but their list is quite limited. I will dwell on them in more detail at the end of the interview.
Mechanism of action of nootropic drugs
The mechanism of action of nootropics has not been fully studied to date. However, the principle underlying the therapeutic effect, repeatedly confirmed in vivo, is still of interest to researchers in the fields of biochemistry, cytology and pharmacology. In particular, researchers know that the effectiveness of nootropics in clinical medicine is associated with several mechanisms observed at the cellular level in the central nervous system:
- enhance the synthesis of ATP and its derivatives;
- enhance the process of synaptic transmission in the central nervous system;
- enhance the plastic process in the central nervous system by increasing the synthesis of RNA and proteins;
- enhance the process of glucose utilization;
- have a membrane-stabilizing and antioxidant effect.
Thus, the mechanism of action of nootropic drugs is associated with the restoration of metabolic and bioenergetic processes in the brain, which affect a person’s mood, performance and well-being. A correctly selected nootropic will have the effects necessary for treatment, which manifest themselves over a long period of time, provided that the recommendations of the attending physician are followed (for example, regarding a rational and healthy lifestyle, attending psychotherapy sessions, taking first-line medications).
Rice. 1. Neuron
What medications should I take for osteochondrosis?
Medicines for osteochondrosis differ not only in the form of release. They are also divided into the following pharmacological groups.
Anti-inflammatory drugs for the treatment of osteochondrosis
The work of non-steroidal anti-inflammatory drugs for osteochondrosis is based on suppressing the production of prostaglandins - hormone-like substances that cause inflammation and pain in the affected areas. Non-steroidal drugs for osteochondrosis can quickly eliminate pain and hot skin, restore local metabolism, relieve swelling, discomfort and deterioration of sensitivity, and relieve pressure on the nerve roots of the spine.
Non-steroidal anti-inflammatory drugs for the treatment of osteochondrosis are produced in various dosage forms - capsules and tablets, gels and creams, solutions for intramuscular, intravenous or subcutaneous administration. Treatment of NSAID drugs for osteochondrosis usually involves a combination of different forms. For example, tablets are used as the main therapy, gels and ointments “quench” residual inflammation, and injections are needed for pain relief. Patches (for example, Voltaren, Versatis) help relieve inflammation at all stages of treatment.
The list of NSAID drugs for osteochondrosis includes:
- artradol;
- ibuprofen (nurofen, dolit, ibuprom);
- ketoprofen (ketonal, fastum, bystrumgel, flexen);
- diclofenac (Voltaren, Diclac, Diclobene, Dicloran Plus, Ortofen);
- ketorolac;
- xefocam;
- indomethacin (indovazin, indobene, indocid);
- nimesulide (nimesil, nise, nimulid, nimika);
- naproxen;
- piroxicam;
- Celebrex (celecoxib);
- febrofide;
- meloxicam (movalis, movasin).
Steroid (hormonal) anti-inflammatory drugs for osteochondrosis are rarely used - mainly in the most advanced cases. These include prednisolone, cortisone, dexamethasone and others.
Chondroprotectors
With osteochondrosis, the spring function of the intervertebral discs deteriorates, which directly depends on the volume of cartilage tissue and its elasticity. To maintain sufficient cartilage thickness, the body must regenerate cartilage cells (chondrocytes) at a rate that roughly matches their destruction. But with dehydration, unbalanced nutrition, stress, metabolic or anatomical disorders, the rate of decay of chondrocytes increases, and new cells are either inhibited in growth or have an insufficient margin of safety. To protect cartilage and restore its normal growth rate, it is worth taking special products based on glucosamine and chondroitin - chondroprotectors. Chondroprotective drugs for the effective treatment of osteochondrosis can stabilize the condition of cartilage, prevent its further destruction and, subject to all medical recommendations, even help restore lost chondrocytes.
Chondroprotective drugs for osteochondrosis include:
- artracs;
- chondrolone;
- rumalon;
- Don;
- chondroxide;
- osterepar;
- teraflex;
- alflutop;
- collagen ultra.
Some of them (for example, Dona) contain only glucosamine, others (Structum, Chondroxide) - only chondroitin. Modern drugs combine active ingredients and additionally include vitamins (artracam).
For a sustainable effect, chondroprotectors (in the form of tablets, injections or external agents) must be taken for life, in courses of 3-6 months.
Warming drugs
To eliminate discomfort in osteochondrosis, the so-called. warming medications. They:
- dilate blood vessels in the skin, which inhibits the transmission of pain impulses to the brain;
- improve blood microcirculation in connective tissue;
- distract the patient from unpleasant sensations.
When irritating drugs are applied, the peak effect is observed after half an hour, and the analgesic effect lasts for 2-4 hours. A local increase in skin temperature is normal.
The list of drugs for the treatment of osteochondrosis includes ointments, creams, gels and tinctures based on:
- camphor (camphor ointment);
- turpentine;
- benzyl nicotinate;
- nonivamide;
- capsaicin (espol ointment, capsicum tincture);
- bee and snake venom.
Most of these drugs have a combined composition - for example, bee venom and NSAIDs or snake venom, salicylic acid and turpentine. Therefore, before use, you must make sure that you are not allergic to each of the components.
Local and general analgesics
Painkillers for osteochondrosis are usually used in the form of tablets and injections. For moderate pain, the usual medicines in the medicine cabinet can help - analgin or paracetamol. Nefopam and Ambene are also effective (has an anti-inflammatory effect, which reduces pain).
In the later stages of osteochondrosis, opioids are prescribed - potent drugs with a number of contraindications. These include tramal (tramadol).
For complex pain relief (for example, blockade), the so-called. “cocktails” that simultaneously have an analgesic, decongestant, anti-inflammatory, local anesthetic and allergen-reducing effect. The composition may include lidocaine or novocaine, bupivacaine, corticosteroids, vitamin B12 and other components.
Important! Analgesics only relieve pain without affecting its cause. Therefore, without proper treatment, osteochondrosis continues to progress, requiring a transition to increasingly serious painkillers.
Vasodilators
Vasodilators for osteochondrosis, or vasodilators, help restore normal blood supply to the tissues around the affected intervertebral joints.
Pain and muscle tension cause the blood vessels to narrow. This impairs tissue nutrition, causes oxygen starvation of the brain and accelerates the progression of the disease. Therefore, in case of cervical osteochondrosis, drugs to normalize blood circulation are especially important. During rehabilitation therapy the following are used:
- pentoxifylline, or trental (vasodilator);
- xanthinol nicotinate (improves blood flow, reduces swelling of nerve roots);
- aminophylline (eliminates circulatory failure);
- Mexidol (pressure and metabolic processes stabilizer);
- vasonite-retard, octolipene (microcirculation stimulants);
- actovegin (tissue regeneration stimulator);
- Cavinton (promotes saturation of tissues with oxygen, dilates blood vessels);
- berlithion (antioxidant).
Vascular medications for osteochondrosis improve peripheral blood circulation and cellular metabolism and relieve pain.
Antispasmodics and muscle relaxants
To eliminate spasm and tension, antispasmodics and muscle relaxants are used. They normalize blood circulation, relieve pain, and restore mobility. Patients are prescribed:
- sirdalud (tizanadine);
- mydocalm (tolperizole);
- baclofen;
- cyclobenzaprine;
- novocaine, lidocaine, trimecaine.
To enhance the effect of drugs to relax muscles in osteochondrosis, they can be prescribed together with clonazepam or diazepam (prescription drugs). These drugs can be addictive, so they are used with caution.
Sedatives
Symptoms of osteochondrosis and treatment with drugs often provoke chronic stress, emotional stress, depression and other disorders of the psycho-emotional spectrum in patients
For general calming and combating insomnia, you can use herbal preparations - for example, tincture of valerian, motherwort, peony.
For more serious disorders, antidepressants are recommended - gidazepam, Cymbalta, Eglonil, Donormil.
Vitamin and mineral complexes
Since osteochondrosis is considered a disease of the whole body, complex vitamin and mineral therapy (complivit, duovit, doppelhertz, multi-tabs) is of great importance. Vitamins A, groups B, C, D, E, calcium and phosphorus preparations help to significantly improve the condition.
Vitamin A
(retinol acetate) is a natural antioxidant that stimulates collagen production and reduces the destruction of chondrocytes, promotes the renewal of joint tissue.
B vitamins
(cyanocobalamin, milgamma, neuromultivit, neurobion, neurorubin, neuroplex, celtican complex, pyridoxine, thiamine) reduce pain, inflammation and numbness of the hands, improve the sensitivity of nerve fibers.
Vitamin D
(calciferol, aquadetrim, vigantol) is responsible for the absorption of calcium and helps restore bone tissue lost due to osteochondrosis.
Vitamin E
(tocopherol) is necessary for normalizing blood circulation, protecting against free radicals and cartilage regeneration.
Don't self-medicate! Good luck to you in the treatment of osteochondrosis!
Images designed by Freepik
The effectiveness of nootropics
The effectiveness of nootropics, in particular, is explained by the therapeutic effect on the neurotransmitter systems of the brain - monoaminergic, cholinergic and glutamatergic. Nootropics help restore the regulation of the synthesis of phospholipids and proteins in neurons, normalize the structure of cell membranes; reduce the oxygen demand of neurons; suppress the formation of free radicals and lipid peroxidation of cell membranes; increase the protection of neurons to adverse factors affecting their proper functioning.
The results of biochemical blood tests and EEG, as well as laboratory experiments using modern microscopes, allow us to visualize the effectiveness of nootropics. For example, the results of an electroencephalogram can clearly see the effect of using nootropics - increased amplitudes of transcallosal evoked potentials, enhanced power spectrum of the EEG of the cortex and hippocampus, an enlarged dominant peak, smoothed interhemispheric asymmetry.
Rice. 2. Visualization of the effect of nootropics on the electroencephalogram
Monoamine neurotransmitters
Classic monoamines include: histamine, adrenaline, dopamine, norepinephrine, serotonin, melatonin. Monoamine neurotransmitters and neuromodulators act as neurotransmitters in the monoaminergic systems of the central nervous system, which regulate a variety of processes in the body, including:
- emotional condition;
- cognitive activity;
- concentration;
- ability to remember information;
- excitation processes.
Cholinergic neurotransmitters
Cholinergic neurotransmitters in the central nervous system are responsible for the processes of excitation and inhibition in the body. Neurotransmitters of this central nervous system support the autonomous functioning of internal organs and vital processes associated with the work of innervated organs and participate in the transmission of motor activity impulses. Cholinergic deficiency directly affects the imbalance of the central nervous system structures associated with it and can cause the development of:
- neurological symptoms;
- emotional-volitional pathology.
Glutamatergic neurotransmitters
Glutamatergic neurotransmitters are involved in CNS processes associated with cognitive function - they help process and store information. In addition, these neurotransmitters are responsible for motor coordination, response to pain, and the body’s immune response; are responsible for the quality of transmission of nerve impulses and the state of the nervous system as a whole.
Rice. 3. Central nervous system
Ensuring drug safety is a priority in modern medicine. It is associated with the creation of a large number of new drugs, the identification of new biological effects of previously synthesized drugs (drugs) that can modify the functional connections of organs and body systems, and the sensitization of patients due to polypharmacy. The results of pharmacoepidemiological studies indicate that underestimation of this problem is fraught with the development of serious consequences, an increase in the number of severe complications requiring hospitalization and often causing death [1-3].
The problem of drug safety is especially acute for patients with cerebrovascular diseases (CVD), since most of them have risk factors for the development of adverse effects of drugs: old age, comorbid pathology, the need to take two or more drugs, a burdened allergic history, etc. [ 4].
Neuroprotectors are widely used in the Russian Federation. Favorable pharmacokinetic parameters, low risk of drug interactions and side effects, and over-the-counter availability have led to their extremely widespread, often unsystematic and uncontrolled use. You should be aware that without taking into account pharmacodynamics and possible drug interactions, the prescription of any drug is associated with serious risks [5].
Neuroprotectors should be prescribed only for specific indications according to the instructions. It is necessary to strictly adhere to the course and daily dosage regimens. The possibility of adverse effects should be taken into account when taking several drugs simultaneously. In addition, it is necessary to keep in mind the patient’s age and the presence of concomitant pathology, predict the development of side effects and assess the risk-benefit ratio. Of the large number of neuroprotectors, only a few have demonstrated effectiveness in clinical studies [5]. The task of drug therapy is not only to find effective and safe drugs, but also to study the effectiveness of combinations that include drugs with different mechanisms of action [6].
Pathogenetic rationale for complex neuroprotection
In clinical practice, drugs that have a complex effect on various brain cells are most often used, since in case of cerebral circulation impairment, protection of not only neurons, but also astrocytes, oligodendrocytes, and microglia is required. Their use can increase the degree of brain adaptation to ischemia, increase cell viability, and ensure better recovery of impaired functions. The processes of neuroplasticity and neuroprotection are of primary importance [6].
Neuroplasticity includes the processes of regeneration of nervous tissue and is considered as the adaptation of a neuron to new functional conditions, reducing damage to brain tissue caused by ischemia.
Cell death occurs within a certain period of time after the development of ischemia and occurs through passive (necrosis) and active (apoptosis) pathways. Excitotoxic cell damage develops within minutes, with inflammation and apoptosis occurring in the following hours and days. The pathobiochemical cascade involves glutamate and calcium cation, the concentration of which is disrupted inside and outside the cell. Normally, apoptosis plays a positive role and, as a rule, does not activate inflammation, but the pathological processes associated with stroke are associated with excitotoxicity and inflammation. Extensive cell damage in the infarct area leads to neuronal swelling and lysis due to massive stimulation of NMDA receptors. Their moderate hyperactivity in the penumbra zone is a trigger for the formation of free radicals and processes leading to apoptotic damage.
Neurotrophic factors determine the processes of cell proliferation, migration, differentiation and survival. Understanding this mechanism is key to developing new treatment strategies. Defense processes can be natural or pharmacologically induced. They are interconnected and together cause a complex of processes of preservation and regeneration of nervous tissue. Pharmacotherapy for CVD should be combined and aimed not only at restoring blood flow in the affected area, but also at eliminating neurometabolic, neurotransmitter, neurotrophic and other reactions that determine the development of destructive changes in neurons. The therapeutic strategy should include correction of cerebral perfusion, systemic hemodynamics, energy metabolism and neurotransmitter metabolism. Adequate use of neurotrophic and neuroprotective drugs can slow down the formation of ischemic damage and increase the brain’s resistance to hypoxia [7].
The most common methods of combined neuroprotection
Most often, an antioxidant and a neurotransmitter drug are prescribed simultaneously [7]. Antioxidants are natural or synthetic substances that slow down or prevent the oxidation of organic compounds. Enzymatic antioxidants created on the basis of superoxide dismutase (SOD), isolated from natural materials (ontosein, oxodrol, peroxinorm), have significant disadvantages: they are unstable, quickly inactivated and have a number of side effects, as a result of which they have limitations for clinical use.
Ethylmethylhydroxypyridine succinate (EMHPS) (Mexidol, Neurox, Mexiprim) has a wide range of pharmacological activity and has the ability to stabilize membranes. Unlike succinic acid preparations, pyridine and succinate residues facilitate the penetration of the molecule into the cell and have a minimal number of side effects. EMGPS, being an antioxidant, has antihypoxic, membrane-protective, nootropic, anticonvulsant and anxiolytic effects. EMGPS stimulate the oxidation of glucose through the pentose phosphate shunt, increasing the level of the pool of reduced nucleotides. Due to stabilization of the level of endogenous antioxidants, the succinate oxidase oxidation pathway is activated, which, under conditions of limited NAD-dependent oxidation in the early stages of hypoxia, allows maintaining a certain level of oxidative phosphorylation. Activation of the succinate oxygenase oxidation pathway during hypoxia increases cell resistance to oxygen deficiency and determines the antihypoxic effect of EMHPS. The drug also inhibits lipid peroxidation, increases SOD activity and the lipid-protein ratio, and reduces membrane viscosity, increasing its fluidity. Modulates the activity of membrane-bound calcium-independent phosphodiesterase, adenylate cyclase, acetylcholinesterase, benzodiazepine, GABA, acetylcholine receptor complexes, which increases their binding to ligands, helps maintain the functional organization of biomembranes, transport of neurotransmitters and improve synaptic transmission. EMGPS increases the content of dopamine in the brain, activates aerobic glycolysis and reduces the degree of inhibition of oxidative processes in the Krebs cycle with an increase in the formation of ATP and creatine phosphate. Pharmacological effects are realized at three levels: neuronal, vascular and metabolic. The combination of pyridine base and succinic acid ensures passage through the blood-brain barrier.
EMGPS is approved for the treatment of various CVD, encephalopathy (hypertensive, atherosclerotic, traumatic, etc.), neurotic and neurosis-like disorders with anxiety, for the relief of withdrawal symptoms in alcoholism, for the treatment of acute intoxication with neuroleptics, etc. EMGPS has a stress-protective effect, which manifests itself in normalization of post-stress behavior, somatovegetative disorders, restoration of the sleep-wake cycle, impaired learning and memory processes, reduction of dystrophic changes in brain structures [8].
The advantage of EMGPS is the low incidence of side effects. Enhances the effect of benzodiazepine anxiolytics, antiepileptic, antiparkinsonian drugs, nitrates, without affecting the state of systemic hemodynamics. The drug has no inhibitory or stimulating effects on spontaneous motor activity, coordination, exploratory behavior, rectal temperature, corneal reflex, does not cause drowsiness, the adequacy of the animal's response to provoking stimuli is maintained, simple reflexes are not impaired, even in high doses. Increasing the dosage by 4-5.5 times does not have a muscle relaxant effect; when used in ultra-high doses, an antiamnestic effect is manifested [8]. EMGPS does not cause hyperactivation, dyssomnia, or increased convulsive readiness. The range of therapeutic doses in the experiment ranges from 10 to 300 mg/kg. As the dose increases, the period of onset of the effect decreases and its severity increases. Stopping treatment does not cause withdrawal syndrome.
Four randomized studies of the use of EMGPS in patients with ischemic stroke (IS) were conducted, one of them was double-blind, placebo-controlled [9, 10]. EMGPS has been shown to be effective in the treatment of chronic cerebral ischemia (CCI) [11–16]. Of particular note is an open comparative controlled study lasting 15 days, which included 60 patients with stage 1–2 CCI aged 45–68 years [17]. Patients of the 1st group received Neurox, 2nd - Mexidol; There were no significant differences between groups by gender and age. A positive effect of both drugs on the oxidative potential of low-density lipoproteins, a decrease in their susceptibility to oxidative processes in vivo,
increased content of α-tocopherol and β-carotene. The therapeutic equivalence of the drugs was recorded.
Neurox (Sotex, Russia) has established itself as an effective, safe agent that improves metabolism and blood supply to the brain, microcirculation, metabolic processes in the ischemic myocardium, increases coronary blood flow in the ischemic zone, and reduces the consequences of reperfusion syndrome in acute coronary syndrome [18, 19 ]. Taking into account possible drug interactions, it can be recommended for the treatment of CVD [20].
Drugs with neurotransmitter and neurometabolic effects
Helps improve metabolic processes and eliminate mediator imbalance in the central nervous system. Of interest are drugs that affect acetylcholine metabolism.
During IS and CCI, the content of phospholipids in the brain sharply decreases due to slower biosynthesis and increased degradation of phosphatidylcholine [21]. The role of phospholipids in hemocoagulation has been studied. Intravascular fibrin formation is characterized by disorders of the blood coagulation system with a violation of the ratio between neutral (NPL) and acidic phospholipids (APL) [22]. The process of transformation of fibrinogen into fibrin, accompanied by a decrease in the content of CPL and an increase in the level of NFL, changes this ratio. It is characterized in each specific case by their pro- and anticoagulant activity. This may be manifested by the stimulating or inhibitory effect of these compounds on prothrombin time values, thromboplastic activity, blood clotting time, fibrinogen concentration and fibrinolytic activity [23]. Under ischemic conditions, the synthesis of phosphatidylcholine decreases, which is an important factor in brain aging and neuronal damage in CVD [24]. In this situation, it is important to prescribe drugs that affect phospholipid metabolism. The use of natural metabolites makes it possible to slow down the progression of the process already in the early stages of the disease.
Citicoline
Of undoubted interest are data on the use of citicoline (cytidine 5'-diphosphocholine; trade names - Ceraxon, Neipilept, Recognan). Its effectiveness over the past 30 years has been studied in detail for CVD in Europe, the USA and Japan [25]. Information was obtained about its pleiotropic effect, impact on the consequences of cerebral ischemia, processes of restoration of the structure and functions of nervous tissue. There is an extensive evidence base for the drug; about 12,000 patients were included in studies of its effectiveness. Citicoline is normally present in all cells of the human body and is a natural product of biochemical processes. Consists of cytidine and choline linked by a diphosphate bridge and is a necessary intermediate in the synthesis of phosphatidylcholine, the main brain phospholipid (Kennedy pathway), reduces the loss of phosphatidylcholine, which is part of the cell membrane. Being a source of choline, it participates in the synthesis of acetylcholine, stimulates the activity of tyrosine hydroxylase and the secretion of dopamine.
In an experiment, citicoline reduced the degeneration of hippocampal neurons caused by the administration of beta-amyloid (BA) [26]. BA is a protein formed as a result of proteolytic processing from the BA precursor (PBA), which is expressed in virtually all animal cells. The severity of cognitive impairment (CD) is directly proportional to its accumulation. Choline in combination with cytidine stimulates the secretion of normal neurotrophic PBA by rat neurons [27]. Citicoline reduces the deposition of BA in the brain, which is clinically manifested by an improvement in cognitive function.
A large number of clinical studies have been conducted on the effectiveness of citicoline in the treatment of CR associated with brain aging and CVD [27]. In addition to its effect on AD, the neuroprotective effect of citicoline is due to the redistribution of the main glutamate transporter EAAT2 and an increase in its uptake [28]. Citicoline leads to the mobilization of bone marrow endothelial progenitor cells, improving functional recovery after acute IS [29].
Citicoline has high bioavailability both orally and intravenously. After absorption, the drug breaks down into choline and cytidine, which easily penetrate the blood-brain barrier, from which citicoline is synthesized in the brain. Its content in blood plasma after oral administration has two peaks - after 1 hour and 24 hours.
Studies have shown the safety and effectiveness of long-term (6 months) administration of citicoline to prevent post-stroke CR [30-32]. The use of citicoline within 24 hours from the onset of IS symptoms and subsequent continuous use for 6 months is an effective means of preventing post-stroke CR compared with placebo. Improvements were observed in time orientation, attention, and executive function. The use of citicoline in patients who underwent stroke for 12 months demonstrated good tolerability and effectiveness in preventing post-stroke CR [33].
The drug citicoline neipilept (Sotex, Russia) is produced from a substance manufactured in Italy and is available in the form of solutions for intravenous and intramuscular administration, as well as a dosage form for oral administration.
An open comparative multicenter randomized study of the effectiveness and safety of the use of Neipilept and Ceraxon in patients with acute carotid IS showed their safety and high efficiency [32], a minimal number of side effects and compatibility with other drugs, which gives grounds to recommend it for use in clinical practice.
Choline alphoscerate
Choline alphoscerate (gliatilin, cereton, cerepro) contains 40% choline, which in the body is converted into a metabolically active form - phosphorylcholine, which penetrates the blood-brain barrier and activates the synthesis of acetylcholine in the presynaptic terminals of neurons [34]. Glycerophosphate is involved in the synthesis of the membrane phospholipid phosphatidylcholine [35].
Choline alfoscerate is a centrally acting parasympathomimetic drug. Three main mechanisms of its action have been established. As a donor of acetylcholine, it helps restore interneuron connections and improve neurotransmission. Participates in the repair of neuronal membranes, reducing the severity of degeneration of free fatty acids [36].
Choline alfoscerate replenishes the biochemical and functional deficiency of the cholinergic system affected by ischemia, which justifies its use in IS [37]. In addition, it has an anabolic effect, manifested in the stimulation of glycerolipid synthesis due to the formation of membrane phospholipid precursors from its breakdown products [38].
Experiments have shown that drugs of this series prevent induced cholinergic deficiency, prevent the development of dementia, and facilitate learning and memory processes by increasing the synthesis and release of acetylcholine in brain structures [39]. The neuroprotective effect of exogenous choline sources during ischemia has been proven in both preclinical and clinical studies [40].
The largest study of the effectiveness of gliatilin in patients with IS was conducted in Italy (2058 patients in 176 clinical centers) [41]. Treatment began no later than 10 days after the development of IS or transient ischemic attack and lasted for at least 6 months. A significant decrease in cognitive and motor impairment was observed after the first month of injection therapy with the drug (1000 mg IM). The results obtained confirm the effectiveness of choline alfoscerate in restoring neurological and cognitive functions. The most significant effect was recorded by the 3rd month of observation. A subsequent meta-analysis studying the use of choline alfoscerate showed its effectiveness against CR, exceeding that of other acetylcholine precursors [42].
Mechanisms of the neuroprotective effect of citicoline and choline alfoscerate
The drugs have different mechanisms of action - the main effect of citicoline is associated with the effect on membranes, the effect on neurotransmission is less pronounced, the dominant effect of choline alfoscerate is an improvement in neurotransmission with a weaker membrane protective effect. Thus, the main mechanisms of citicoline are the repair of neuronal membranes, reducing the degeneration of free fatty acids, and choline alfoscerate is increasing the production and release of acetylcholine from the terminals [43]. The difference between choline alfoscerate is its ability to restore acetylcholine levels, while the main neuroprotective properties of citicoline lie in the preservation of both external and internal neuronal membranes [44-46]. Citicoline helps stabilize protein synthetic processes in the vascular wall and neurons. If therapy is not started in a timely manner, correction of the destruction of these membranes will no longer be possible, therefore, to enhance the effects of these drugs, it is advisable to use them in combination as early as possible in the disease [47, 48]. The choice of cholinergic drugs for patients with CVD should be pathogenetically justified, taking into account the dysfunction of modulating subsystems of brain activation, the predictors of which are the patient’s age, level of consciousness, the presence of somatic pathology, a history of cerebrovascular accidents, and CR.
Disturbances in metabolic processes in the vascular wall and neurons underlie the development of subsequent neurodegenerative lesions. Neurological diseases often occur against the background of severe somatic pathology and are often accompanied by decompensation of an existing brain lesion, especially in elderly patients [49]. Therefore, it is important to prescribe drugs that affect the metabolism of phospholipids, since they are a structural component of all cell membranes, and from them Numerous cell functions are directly dependent. The more pronounced the hypoxia, the higher the consumption of phosphatidylcholine. Depletion of its pool exceeding 20% is accompanied by membrane destruction [50]. Replenishment of phosphatidylcholine deficiency is not able to eliminate the cause of the disease, therefore citicoline should be considered as a universal membrane protector capable of preserving the basic properties of biological membranes in patients with severe somatic pathology, in acute and recovery periods of IS and traumatic brain injury, in patients with Parkinson's disease, hypertensive encephalopathy with severe CR.
Over a certain period of time, choline reserves for acetylcholine synthesis can be provided by hydrolysis of phosphatidylcholine by phospholipases. A decrease in its concentration leads to the death of cholinergic neurons [51]. This biochemical phenomenon is called phosphotidylcholine autocannibalism [52]. Therefore, it is necessary to enhance the cholinergic effect through the use of a choline donor - choline alfoscerate.
Another form of use of drugs in young and middle-aged patients with minimal clinical manifestations is initial therapy with choline alfoscerate, since the leading clinical picture is mild CR due to acetylcholine deficiency. Also, choline alfoscerate should be considered as a drug that stimulates cholinergic neurotransmission in patients with acute, including severe IS [53].
Thus, when treating patients with CVD, it is necessary to use rational combination therapy with the use of neuroprotectors, taking into account information about their possible positive and negative effects.
Nootropics for children, adults and the elderly
Currently, clinical studies of nootropics are being conducted in the USA and Europe to identify therapeutic effects that can be used to treat diseases in various fields of medicine. It should be emphasized that we can talk about nootropics with proven effectiveness only in terms of the positive mechanism of their action, recorded by both researchers and doctors in clinical practice.
For example, on February 12, 2010, data from a clinical study on the use of nootropics in the treatment of CNS pathologies was published in the USA (Malykh A., Sadaie R. “Piracetam and piracetam-like drugs: from basic science to novel clinical applications to CNS disorders”). The study demonstrated the neuroprotective effect of the substance, effectiveness in the treatment of cognitive disorders of cerebrovascular and traumatic etiology, as well as associated depressive states. In particular, the study notes the effectiveness of nootropics as part of complex therapy in the treatment of epilepsy.
Similar and other positive effects of using nootropics are noted in many modern clinical studies, the results of which are published in scientific journals and are publicly available on the Internet. In other words, nootropics with proven effectiveness exist, they are presented on the pharmaceutical market, and are actively prescribed by doctors in various fields of medicine, but the final decoding of the therapeutic mechanism of drugs in this group has yet to be learned.
Nootropics for children
Nootropics are used in the treatment of various diseases associated with central nervous system pathology in children. In the first years of a child’s life, they can be prescribed for the prevention and treatment of delayed psycho-speech-motor development; at a later age - to stimulate the activity of the central nervous system systems responsible for concentration, the learning process, memory, and the ability to reproduce information.
Nootropics for children include drugs with dominant or predominant mnestic effects (“true” nootropics):
- racetams;
- cholinesterase drugs;
- neuropeptides and their analogues;
- amino acid activators;
- neuroprotectors;
- activators of brain metabolism;
- cerebral vasodilators;
- calcium antagonists;
- antioxidants;
- GABA activators.
Indications for prescribing nootropics for children are:
- delayed speech development;
- impaired mental function;
- cognitive impairment due to organic brain damage (consequences of neuroinfections, head injury, genetic pathology);
- mental retardation;
- ADHD;
- Parkinson's disease;
- neurogenic urination disorders;
- neurosis-like conditions;
- stuttering, predominantly clonic;
- asthenic and anxiety-neurotic conditions;
- epilepsy (in complex therapy).
Nootropics for adults
Biological therapy for mild, borderline and severe mental disorders may include nootropic drugs. They are prescribed for the occurrence of pathological conditions associated with cognitive functions, mood and sleep. For example, they have a positive effect on the psycho-emotional state and personal effectiveness as an addition to psychotherapeutic treatment, and accelerate the achievement of the desired result.
Nootropics for adults used in mono- and complex therapy of mental disorders:
- pyrrolidone derivatives (Nootropil - note, for example, and further);
- cyclic derivatives, GABA (Pantogam, Phenibut, Aminalon);
- acetylcholine precursors (Deanol);
- pyridoxine derivatives (Pyritinol);
- Devincan derivatives (Vincamine, Vinpocetine);
- neuropeptides (Vasopressin, Oxytocin, Thyroliberin, Cholecystokinin);
- antioxidants (Ionol, Mexidol, Tocopherol).
The above nootropics are prescribed for mental disorders arising from vascular diseases of the brain (F00-F09, “Organic, including symptomatic, mental disorders”):
- exogenous-organic mental disorders;
- transient psychotic disorders;
- persistent mental disorders;
- psychoorganic disorders;
- vascular dementia.
Nootropics for older people
Neuroprotective nootropic therapy for older people is prescribed for Alzheimer's disease, Pick's disease, as well as syndromes including confusion, instability of attention, confusion, disorientation in space and time, memory problems, fragmented thinking, emotional imbalance, fear, anxiety, motor agitation or lethargy, deceptions of perception, sleep disturbances.
Rice. 4. Structure of the nervous system
What nootropic drugs are prescribed to older people and for what purpose?
Indications for prescribing nootropics to older people are the following conditions: • Alzheimer's disease. • Syndromes of confused consciousness and fragmented thinking. • Pick's disease. • Disorientation in space and time. • Confusion and instability of attention. • Emotional imbalance. • Anxiety disorder. • Illusory perception. • Memory problems. • Sleep disorders. • Motor overexcitation or retardation.
In addition, nootropics can also be prescribed for preventive purposes to slow down age-related changes in the neuropsychic sphere associated with cerebrovascular accidents, weakening of memory and cognitive abilities. Among the nootropic drugs used for older people, the most common and popular are: • Cavinton, the active ingredient of which is vinpocetine. Its main therapeutic effect is aimed at improving cerebral circulation by reducing blood viscosity and, accordingly, improving the supply of oxygen to the brain. It is characterized by a targeted selective effect on the affected area of the brain, so this nootropic drug is especially effective in the treatment and rehabilitation after stroke, vascular dementia and cerebrovascular accidents. It is also used in the treatment of vascular and retinal lesions and Meniere's disease. Side effects may include nausea, heartburn, weakness, headache and tachycardia, which is a disadvantage of the drug and a contraindication for its use in case of heart rhythm disturbances (arrhythmias). • Encephabol – stimulates metabolic processes in the brain by accelerating the utilization of glucose, normalizes blood circulation in areas affected by ischemia, and helps restore the functions of the nervous system. Other therapeutic effects include improved memory, increased mental activity and overall central nervous system tone. It helps well in overcoming the negative consequences of encephalitis, as well as in the treatment of cerebroasthenic syndrome and mental retardation in children. The downside is the ability to cause allergic reactions in people sensitive to pyritinol, as well as the high price.
• Phenibut is a drug that combines nootropic and tranquilizing effects. Which manifests itself in a decrease in the excitability of the nervous system, a decrease in anxiety and fear. The drug prolongs the duration of action and enhances the effect of sleeping pills. With long-term use, it increases physical and intellectual capabilities, normalizes sleep, and improves memory. Effective in the complex treatment of withdrawal syndrome in alcoholism. The downside is the possibility of withdrawal syndrome after completing the course of the drug.
• Picamilon is a nootropic drug popular among doctors and patients, which has several effects: a psychostimulant, a tranquilizer and an antioxidant. Improves metabolic processes and blood supply to brain tissue, reduces the intensity of headaches, relieves anxiety and nervous tension, and also increases a person’s physical and intellectual capabilities. Has a positive effect on the restoration of motor and speech functions after stroke and toxic lesions of the brain. In older people, it has a good effect in the complex treatment of migraines, cerebrovascular accidents, and retinal diseases. Side effects include the possibility of developing an allergic response to this drug.
The use of nootropics in older people should be treated very carefully, taking into account the depth of age-related changes, possible side effects, prevailing symptoms, the presence of concomitant diseases and the general condition of the body. Only a specialist can objectively evaluate all these aspects and correctly prescribe treatment using nootropics. Prescribing these drugs to your elderly relatives yourself is extremely undesirable and unsafe for their health.
List of nootropic drugs
Nootropic drugs for the brain can be found in the international Anatomical-Therapeutic-Chemical Classification of Medicines. The list of nootropics in the subsection “Other psychostimulants and nootropic drugs” (N06BX), which is included in the section “Psychostimulants, drugs used for attention deficit hyperactivity disorder, and nootropic drugs” (N06B), contains:
- Meclofenoxate;
- Pyritinol;
- Piracetam;
- Deanol;
- Fipexide;
- Citicoline;
- Oxiracetam;
- Pirisudanol;
- Linopyrdine;
- Nisophenone;
- Aniracetam;
- Acetylcarnitine;
- Idebenone;
- Prolintane;
- Pipradrol;
- Pramiracetam;
- Adrafinil;
- Vinpocetine;
- Mebicar;
- Phenibut.
The list of nootropics does not end with the names above. On the domestic pharmaceutical markets there are other derivatives, synthetic analogues and drugs that have the properties of nootropics, but are not such. It should be noted that recently there has been a fashion for precisely these “latest generation nootropics” - dietary supplements that can be purchased without a prescription. As a rule, they are complexes of vitamins and substances of plant origin.
In the strict sense of the word, it is not possible to talk about the latest generation of nootropics. It should be understood here that the first nootropic, by definition, was piracetam. Racetams, which have variations in formula and therapeutic effect, and drugs with nootropic properties are still being developed by pharmaceutical companies. Some of them are prohibited in the United States and, in particular, are classified as new psychoactive substances (NPS) in several European countries.
Features and principles of therapy
According to its concept, neuroprotection has several directions:
- Primary, where the effect is aimed at interrupting the rapid mechanisms that contribute to cell death. This is problematic to implement due to the selective nature and the importance of accurately detecting the receptor that is involved in the process.
- Secondary, aimed at reducing the severity of the consequences of ischemic damage.
Neuroprotective therapy is used not only for acute conditions associated with brain function. In this way, chronic diseases of the nervous system are also treated. Neuroprotection is prescribed for:
- vegetative-vascular dystonia;
- neuroses;
- encephalopathy;
- depressive disorders;
- asthenia;
- neuroinfections.
The scheme for a specific patient is formed individually. An anamnesis is collected and the clinical picture is studied in detail. The course also depends on the general health of the patient.
List of used literature
1. Klitochenko G.V., Malyuzhinskaya N.V. "The use of nootropic drugs in pediatrics."
2. Pichikov A.A., Popov Yu.V. "Anorexia nervosa in adolescent girls: course options, relapse factors and suicidal risk in the early stages of treatment."
3. Davydova O.N., Boldyrev A.A. "Glutamate receptors in cells of the nervous and immune systems."
4. Vostrikov V.V. "The place of piracetam in modern practical medicine."
5. Shabalov N.P., Skoromets A.A., Shumilina A.P. “Nootropic and neuroprotective drugs in pediatric neurological practice.”
6. Malykh A., Sadaie R. “Piracetam and piracetam-like drugs: from basic science to novel clinical applications to CNS disorders.”
7. Calliauw L., Marchau M. “Clinical trial of piracetam in disorders of consciousness due to head injury.”
8. Rybak V.A., Matokhina N.V. “Nootropic drugs in the clinical practice of a neurologist.”
Share
Share
Goals of drug treatment
Treatment of osteochondrosis with drugs is so effective in the early stages of the disease that, with a properly selected treatment regimen, it can completely cure osteochondrosis or permanently eliminate its most unpleasant symptoms. In the later stages, drug control of the disease is possible.
Medicines for osteochondrosis are designed to influence the disease not only symptomatically, but also to eliminate its causes systemically. Therefore, therapy is carried out in the following directions:
- anesthesia of affected areas;
- relieving inflammation and stopping the acute period of the disease;
- restoration of microcirculation in affected tissues;
- improving metabolic processes and protecting cartilage from further destruction (for example, by free radicals);
- regeneration of cartilage tissue in intervertebral discs;
- restoration of mobility in the vertebral joints.
In cases where the disease is accompanied by depression or emotional stress, therapy is also aimed at restoring a normal psychological state.
During the period of remission, patients can do without medications or take them in courses in prophylactic dosages.
Cost of treatment in our clinic
| Service | Price | |
| Ambulatory treatment | ||
| Psychiatrist consultation | 4 500 ₽ | |
| Consultation with a psychotherapist | 4 500 ₽ | |
| Psychodiagnostics extended | 7 000 ₽ | |
| Consultation with a psychiatrist at home | 6 000 ₽ | |
| Treatment in hospital | ||
| Delivery to hospital | For free | |
| Standard room | 7 700 ₽ | |
| 3-bed superior room | 10 600 ₽ | |
| 2-bed superior room | 13 700 ₽ | |
| 1 local VIP chamber | 19 000 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |