Convulsions, paralysis, paresis are signs of damage to the nervous system. Paresis is a decrease in muscle strength that is caused by damage to the nerve pathways connecting the brain to a muscle or group of muscles. The difference between paresis and paralysis is that with paralysis there is complete immobilization of a part of the body, and with paresis it is partial. Paresis can occur with any type of damage to the brain, spinal cord, or peripheral nerves.
Depending on the level of damage, neurologists distinguish between central and peripheral paresis. At the Yusupov Hospital, doctors use comprehensive treatment of paresis, an individual approach to the choice of method of therapy and rehabilitation of each patient.
Neurologists prescribe modern medications that are highly effective and have minimal side effects. The rehabilitation clinic is equipped with modern equipment for mechanotherapy. Exercise therapy instructors use innovative methods of physical therapy. Specialists at the Yusupov Hospital adhere to the principles of evidence-based medicine and use the best practices of their foreign colleagues. The hospital has created comfortable conditions for patients to stay, which help create a positive attitude toward recovery.
Types of paresis
Central paresis occurs when the brain or spinal cord is damaged. Disorders develop below the site of damage. They capture the right or left half of the body. This condition is called right-sided or left-sided hemiparesis. Paresis of the left arm is called left-sided monoparesis.
If, as a result of central paresis, disturbances occur in both arms or both legs, we are talking about paraparesis, and if motor function is impaired in all four limbs, we are talking about tetraparesis.
Chapter 6. Paralysis and other movement disorders
General views
Loss of the ability to control voluntary muscle movements is usually described by patients as “muscle weakness” or as difficulties that can be interpreted as “loss of agility.” The diagnostic approach to the problem begins with determining which part of the nervous system is affected. It is important to determine whether weakness arises from upper motor neuron disease (motoneurons in the cerebral cortex and their axons descending through the subcortical white matter, internal capsule, brain stem and down the spinal cord) or from "motor unit" disease (lower motor neurons in the ventral horn). spinal cord and their axons in spinal roots and peripheral nerves, neuromuscular transmission and skeletal muscles). [Each motor nerve cell, through the tree-like branching of the terminal parts of its fibers, is in contact with many muscle fibers: together they form a “motor unit.” — Approx. translation
General characteristics: dysfunction of the upper (central) motor neurons - increased muscle tone (spasticity), increased deep tendon reflexes, positive Babinski sign.
Lower motor neuron dysfunction: decreased muscle tone, decreased reflexes, muscle atrophy.
In table Figure 12-1 presents symptoms of muscle weakness and other manifestations that occur when various parts of the nervous system are affected. Table 12-2 shows the most common causes of muscle weakness due to the primary location of the lesion.
Grade
From the anamnesis, attention is paid to the rate of development of muscle weakness, the presence of sensory disturbances and other neurological symptoms, information on the use of medications, predisposing factors and family history. During physical examination, the location of the lesion should be determined in accordance with the criteria outlined earlier and in Table. 12-1.
When there is damage to the brain or spinal cord, studies such as CT, MRI, and myelography are important to recognize the causes of the disease, especially in structural and demyelinating processes. Lumbar puncture is diagnostically significant for demyelinating and infectious processes; examination of blood serum and urine - for eating disorders and intoxications; biopsy of the affected tissue - for differential diagnosis between a tumor and an infectious process.
Table 12-1 Clinical differences in muscle weakness in different parts of the nervous system
| Localization of the lesion | Clinical signs of muscle weakness | Associated symptoms |
| UPPER MOTONEURON (central palsy) | ||
| Cortex | Hemiparesis (face and arm predominantly, or leg predominantly) | Unilateral sensory loss, seizures, homonymous hemianopsia or quadrant hemianopsia, aphasia, apraxia |
| Inner capsule | Hemiparesis (face, arm, leg may be equally affected) | Unilateral sensory loss, homonymous hemianopsia or quadrant hemianopsia |
| Brain stem | Hemiparesis (arm and leg; face may not be involved at all) | Dizziness, nausea and vomiting, ataxia and dysarthria, impaired eye movements, impaired cranial innervation, impaired consciousness, Horner's syndrome |
| Spinal cord (damage to both halves) | Tetraparesis if the upper and middle cervical regions are affected; lower paraparesis, if the lower cervical and thoracic regions are affected | Level of sensory disorders; dysfunction of the rectum and bladder |
| Spinal cord (damage to one half) | Hemiparesis below the level of the lesion (Brown-Séquard syndrome) | Loss of pain sensitivity on the opposite side, tactile and muscle-articular on the affected side below its level |
| "MOTOR UNIT" (peripheral paralysis) | ||
| Brainstem and spinal motor neurons | Weakness of the muscles innervated by motor neurons of the motor nucleus of the cranial nerve or the anterior horn of the spinal segment | Fasciculations and fibrillations of suffering muscles and their atrophy; sensory disturbances in the corresponding dermatomes |
Table 12-1 Clinical differences in muscle weakness in different parts of the nervous system
(continuation)
| Localization of the lesion | Clinical signs of muscle weakness | Associated symptoms |
| Spinal cord root | Weakness of the muscles innervated by the cranial nerve root or spinal cord | Loss of sensation and radicular pain in the corresponding dermatome |
| Peripheral nerve Polyneuropathy | Peripheral muscle weakness is greater in the feet than in the hands; characterized by symmetry | Peripheral sensory disturbances, usually more in the feet than in the hands |
| Mononeuropathy | Muscle weakness according to the zone of innervation of a particular nerve | Loss of sensation and pain in the area of innervation of a particular nerve |
| Neuromuscular junction | Pathological muscle fatigue, often in combination with visual impairment in the form of diplopia and ptosis | There are no sensory impairments; reflexes are normal |
| Muscles | Weakness (most often) of the proximal muscles | There are no sensory disturbances, with severe damage there is a decrease in reflexes; there may be muscle pain upon palpation |
Electromyography and the study of the speed of impulse transmission along nerve fibers help to understand the damage to the “motor unit”. As a result, it is possible to differentiate lesions of various components of the “motor unit”. MRI or myelography is important in assessing the structural causes of nerve root diseases: urine and serum examination may be supplemented by cerebrospinal fluid analysis to rule out systemic lesions; Serum CK is an indicator of muscle tissue damage; Nerve biopsy is rarely used, but muscle biopsy is diagnostic for many muscle diseases.
Table 12-2 Common Causes of Muscle Weakness
UPPER MOTOR NEURONS (CENTRAL LESION)
Cortex: ischemia, hemorrhage, damage to the cortex as a result of an intracerebral pathological process (primary or metastatic cancer, abscess); damage to the cortex by an extracerebral pathological process (subdural hematoma); degeneration (amyotrophic lateral sclerosis).
Subcortical white matter or internal capsule: ischemia, hemorrhage, tissue damage by intracerebral pathological process (primary or metastatic cancer, abscess); pathoimmune process (multiple sclerosis); infection (progressive multifocal leukoencephalopathy).
Brain stem: ischemia, pathoimmune process (multiple sclerosis). Spinal cord: compression (cervical spondylosis, cancer metastases, epidural abscess); pathoimmune process (multiple sclerosis, transverse myelitis); infection (AIDS myelopathy, HTLV-1 myelopathy, tabes dorsalis); nutritional deficiency (subacute combined degeneration).
"MOTOR UNIT" (PERIPHERAL LESION)
Spinal cord motor neurons: degeneration (amyotrophic lateral sclerosis);
infection (poliomyelitis).
Spinal root: compression (degenerative disc disease); pathoimmune process (Guillain-Barré syndrome), infection (AIDS-associated polyradiculopathy, Lyme disease)
Peripheral nerve: metabolic damage (diabetes mellitus, uremia, porphyria); toxic damage (ethanol, heavy metals, abundance of drugs, diphtheria); nutritional deficiency (cyanocobalamin deficiency); pathoimmune process (paraneoplastic, paraproteinemia); infection (AIDS-associated polyneuropathy, multiple mononeuropathy); nerve compression.
Neuromuscular transmission: pathoimmune process (myasthenia gravis); toxic effects (botulism, aminoglycosides).
Muscles: inflammation (polymyositis, including generalized myositis); degeneration (muscular dystrophy); toxic damage (glucocorticoids, ethanol, azathioprine); infection (trichinosis); metabolic lesions (hypothyroidism, periodic paralysis); congenital diseases (central core disease).
Movement disorders
Movement disorders are often divided into akinetic rigid forms, in which muscle stiffness and slowness of movement are noted, and hyperkinetic forms, when involuntary movements are pronounced. In any case, muscle strength is usually preserved.
Most movement disorders arise as a result of disruption of the functional activity of mediators in the basal ganglia; the pathogenesis can be different. The most common causes are degenerative diseases (congenital or idiopathic), possibly drug-induced, organ system failure, central nervous system infections, or basal ganglia ischemia. Below is a brief overview of the clinical aspects of the main categories of movement disorders.
Bradykinesia
The patient's inability to initiate movement or perform normal voluntary movements easily and quickly. Slowness of movements and a decrease in the number of automatic movements, such as swinging arms when walking and blinking, are noted. This usually indicates Parkinson's disease.
Tremor
Rhythmic oscillations of a body part relative to a fixed point, usually accompanied by tremor of the distal extremities and, less commonly, of the head, tongue, or lower jaw. Tremor can be divided into types depending on the location and range of movements. The most common type is large-scale tremor at rest - 4-5 muscle contractions per second, which is a sign of Parkinson's disease; pronounced postural (tonic) tremor with a frequency of 8-10 muscle contractions per 1 s may be a hypertrophied version of physiological tremor or a sign of essential hereditary tremor, characteristic of several members of the same family. To treat the latter, propranolol (Anaprilin) or primidone (Hexamidine) are used.
Asterixis
Rapid arrhythmic movements that interrupt background voluntary muscle contractions, usually rapid flexion and extension of the hands extended forward. This “liver pop” (in liver failure) can also be observed with drug-induced encephalopathy, failure of certain organ systems, or infection of the central nervous system. Treatment should be aimed at the disease underlying the tremor.
Myoclonus
Brief, arrhythmic muscle contractions or twitches. Like asterixis, it is usually a sign of disseminated encephalopathy, sometimes noted after short-term cardiac arrest, when widespread cerebral hypoxia causes multifocal myoclonus. Treatment with the following drugs is effective: clonazepam, valproate, baclofen.
Dystonia
Involuntary long-term posture or poorly changeable fixed pathological postures. They are often ridiculous, pretentious, with forced flexion or extension in individual joints. Dystonia is generalized or focal in nature (spasmodic torticollis, blepharospasm). Symptomatic treatment is carried out with high doses of anticholinergic drugs, benzodiazepines, baclofen and anticonvulsants. Local injections of botulinum toxin are effective for some focal dystonias.
Choreoathetosis
A combination of chorea (fast, jerky movements) and athetosis (slow, jerky movements). These two types of pathological movements coexist, although one of the components may be more pronounced. Choreic symptoms predominate with involuntary movements of rheumatic (Sydenham's disease) chorea and Huntington's disease. Athetosis dominates the picture of some forms of cerebral palsy. Long-term use of antipsychotics can lead to slow dyskinesia, the symptoms of which are choreoathetosis affecting the muscles of the cheeks, tongue and lower jaw. Benzodiazepines, reserpine, and low doses of antipsychotics are used in treatment, although the results are often disappointing.
Tiki
Stereotypical, meaningless movements such as blinking, sneezing or coughing. Gilles de la Tourette syndrome is rare and severe. Its clinical picture includes motor tics (convulsions of the face, neck, shoulders), head tics (grunting, pronouncing words), “behavioral tics” (coprolalia, echolalia). The causes of the syndrome are unknown. Treatment with haloperidol usually reduces the frequency and severity of the syndrome.
Main causes of central paresis
Central paresis develops due to the following diseases:
- stroke;
- traumatic brain injuries, traumatic spinal cord injuries;
- encephalitis;
- neoplasms of the brain and spinal cord;
- osteochondrosis, intervertebral hernia.
The causes of central paresis are cerebral circulatory insufficiency due to atherosclerosis or arterial hypertension, multiple sclerosis, cerebral palsy, amyotrophic lateral sclerosis. Bladder paresis is a temporary or permanent loss of the ability of the muscular wall of the bladder to contract. It occurs with spinal trauma, spinal cord tumors.
Signs of central paresis
With central paresis, muscle strength decreases to varying degrees. In some cases, patients are worried about rapid fatigue and awkwardness, while in others there is an almost complete loss of movement. Since with central paresis the part of the spinal cord below the site of injury remains intact, it tries to compensate for motor disorders. This leads to an increase in muscle tone, strengthening of normal reflexes and the appearance of pathological ones, which do not occur in a healthy person. Due to spastic paresis, contractures can develop - restriction of movements in the joints.
1.General information
First of all, let’s define, as always, the terminology. Paralysis is complete and unconditional immobility of an organ or system for which motor activity is the main natural function. This is the inability of the patient to cause such activity "from within" - neither by conscious nor unconscious effort of will, while from the outside, for example, a paralyzed leg can be rotated at the hip joint or bent at the knee with the help of one's own hands or the hands of another person. This is the difference between paralysis, say, muscle spasm or joint contracture, when such movement is impossible in principle; The term “paralysis” emphasizes precisely the inability of the affected organ to carry out the command of the central nervous system.
Paresis translated from Greek means “weakening, loss of strength”; this term refers to incomplete paralysis (which, by the way, is also translated as “relaxation”), when the available muscle effort or the original range of possible movements is partially preserved; the degree of this preservation can vary widely.
As a synonym for the concept of “paralysis”, the term “plegia” (“stroke”) is often used, which is semantically close to the concepts of “apoplexy” and “stroke” - which apparently formed the etymological basis of the outdated Russian phraseological units “suffered a blow” ", "paralysis after a blow", "apoplexy", etc. However, in modern medical terminology, the word "plegia" is usually used with qualifying prefixes: hemiplegia (one-sided paralysis), mono-, para- or tetraplegia (respectively, paralysis of one , both same-level or all four limbs).
A must read! Help with treatment and hospitalization!
Peripheral paresis
Peripheral paresis develops when the nerve is directly damaged. In this case, disorders develop in one group of muscles that this nerve innervates. Muscle weakness may be present in only one leg or arm. The larger the nerve is damaged, the larger part of the body is affected by paresis or plegia (paralysis).
Peripheral paresis develops due to the following reasons:
- degenerative diseases of the spine, radiculitis;
- demyelinating diseases;
- nerve damage due to connective tissue diseases and vasculitis;
- compression of nerves (“tunnel syndromes”);
- nerve injuries;
- poisoning with alcohol and other toxic substances.
In the presence of peripheral paresis, muscle weakness, weakened reflexes, and decreased tone occur. Involuntary muscle twitching is noted. Over time, muscle atrophy develops (muscles decrease in volume) and contractures occur.
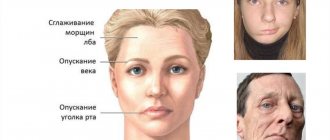
Facial paresis develops when the facial nerve is damaged. It is characterized by impaired functioning of facial muscles. Most patients have unilateral lesions, but total paresis also occurs. The main symptom indicating the progression of facial nerve paresis is facial asymmetry or the complete absence of motor activity of muscle structures on the side of the lesion.
3. Symptoms and diagnosis
The main symptoms of paralysis and paresis, in fact, have already been described in the introductory part. However, there are a lot of clinical nuances and significant typological features that have given rise to a number of classifications. Thus, diagnostically important indicators are the degree of immobility (from mild to deep paresis and complete paralysis), localization of lesions of the nervous system (central, peripheral) or muscle groups (for example, only extensors, only smooth muscles, etc.), the degree of preservation of sensitivity ( complete absence, paresthesia, pain, numbness), preservation and nature of reflexes, etc. However, the essence remains the same: there are no movements either in a dream, or in reality, or under the influence of sedatives, or in any specific, so-called. conditionally desirable situations (which distinguishes true paralysis or paresis, say, from hysterical astasia-abasia, which develops according to a completely different etiopathogenetic “algorithm”).
The diagnosis of “paralysis” or “paresis” itself, even in the mildest form of the latter, can be established and reliably confirmed by an experienced neurologist during a standard clinical examination: for this purpose, a number of diagnostic criteria have been developed and applied, as well as dynamic, static, reflexological tests. Establishing the causes of paralysis sometimes takes quite a long time and requires the use of one or another combination of methods that exist in the extensive diagnostic arsenal of modern medicine - from high-tech imaging and laboratory analytical equipment to experimental psychological, medical genetic and other types of special research.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnosis of paresis
Neurologists at the Yusupov Hospital identify paresis and paralysis during an examination. The doctor asks the patient to make different movements, then tries to bend or straighten the affected limb and asks the patient to resist. The patient is asked to perform a test, which involves trying to hold both limbs of the same name suspended. If muscle strength is reduced in one of the limbs, then after 20 seconds it noticeably drops down.
After the examination, the doctor prescribes an examination that helps to identify the cause of paresis:
- computed or magnetic resonance imaging;
- neuromyography;
- clinical, biochemical and immunological blood tests;
- examination of cerebrospinal fluid obtained by lumbar puncture.
After analyzing the results of the study, the neurologist prescribes drug therapy. Professors and doctors of the highest category discuss severe cases of paresis at a meeting of the Expert Council and make a collegial decision regarding the tactics for further management of patients with paresis.
Treatment and rehabilitation for paresis
Neurologists at the Yusupov Hospital prescribe drug therapy depending on the cause and type of paresis. Rehabilitation treatment is of great importance for restoring movements and preventing contractures. The Yusupov Hospital is equipped with modern equipment from leading world manufacturers. The rehabilitation clinic employs exercise therapy instructors who improve their professional level in leading European and Russian rehabilitation centers.
Rehabilitation for paresis includes:
- therapeutic exercises;
- mechanotherapy on special simulators;
- massage;
- neuromuscular stimulation;
- use of orthoses;
- physiotherapeutic procedures.
For the convenience of patients, comprehensive rehabilitation programs have been developed that allow them to save the family budget and receive a full course of rehabilitation therapy at a stable, affordable price. In order to undergo a course of treatment and rehabilitation for paresis, call the Yusupov Hospital.
Treatment of paralysis
Treatment of paralysis should be aimed at eliminating the cause that caused it. Treatment takes place both conservatively and through surgical intervention.
Conservative treatment consists of:
It is not the paralysis itself that is treated surgically, but the disease that causes it. The surgical intervention consists of:
Sign up for paralysis treatment
Make an appointment