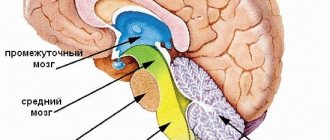
general information
The anatomy of the spinal cord differs from the brain in its oblong structure. In Latin the organ is called medulla spinalis. It is a thickened tube with a small channel inside, slightly flattened in front and behind. It is this structure that ensures the normal transportation of nerve impulses from the main organ located in the cranium to the peripheral structures of the nervous system.
Locally, the organ is located in the spinal canal, where soft and bone tissues and nerve endings responsible for many functions of the human body are concentrated. Without a normally functioning spinal cord, natural breathing, digestion, heartbeat, reproductive activity, and any motor activity are not possible.
In humans, it begins to form at about 4 weeks of development inside the mother’s womb. But in what form it is observed in an adult, it appears much later; at first it is a neural tube, gradually developing into a full-fledged organ. It completes its formation within 2 years after birth.
Structure
The local location of the spinal cord along the entire back has its own characteristics. This physiology ensures that the organ performs its basic functions. The organ begins at the level of the 1st cervical vertebra, where it is gently rebuilt into the brain, but there is no clear division in them. At the junction there is a crossover of the pyramidal tracts responsible for the motor activity of the limbs. The spinal cord ends in the region of the 2nd lumbar vertebra, so it is shorter in length than the entire spine as a whole. This feature allows lumbar puncture to be performed at the level of the 3-4 lumbar vertebrae, without the risk of damaging the spinal cord.
What is special about the structure? The oblong tube has two grooves at the front and back. The brain is covered by three membranes:
- Solid. It is the tissue of the periosteum of the spinal canal, followed by the epidural space and the outer layer of the dura mater.
- Cobweb. A thin, colorless plate that fuses with the hard shell in the area of the intervertebral foramen. In the place where there is no fusion, the subdural space is located.
- Vascular. A soft membrane separated from the previous one by a subarachnoid space with cerebrospinal fluid. The membrane is adjacent to the spinal cord and consists mainly of choroid plexuses.
The space between them is filled with cerebrospinal fluid - cerebrospinal fluid. The gray matter is located in the center of the organ. It consists of intercalary and motor neurons. It also contains two types of horns: the anterior ones, which contain motor neurons, and the posterior ones, where interneurons are located.
External characteristics
The external structure of the spinal cord largely follows the contours of the spine, since the structures adapt to its physiological curves. Two thickenings are observed in the area of the neck and lower thoracic, the beginning of the lumbar calving. These places are characterized as exits of the roots of the spinal nerves responsible for the innervation of the arms and legs.
The external structure can be briefly described by the following characteristics:
- The shape is cylindrical, flattened on the front and back sides.
- Visually, the spinal cord looks like an elongated “cord” with processes.
- On average, the length of the organ is 42-44 cm, but directly depends on the person’s height.
- The mass is 34-38 g, which is 50 times less than the organ of the brain.
- There are two grooves in front and behind, which visually divide the organ into two symmetrical parts.
- In the middle there is a canal, which in the upper part communicates with one of the ventricles of the brain. Inferiorly, the central canal expands, forming the terminal ventricle.
The thickness of the spinal cord is uneven and depends on in which part the measurement is taken. The organ also has four surfaces: two rounded lateral, a convex posterior and a flattened anterior. The external structure is in many ways reminiscent of the internal part of the ridge, since the organ fills the entire canal. The organ is reliably protected by bone tissue.
Internal structure
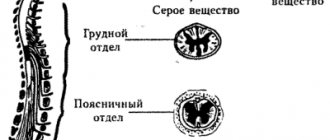
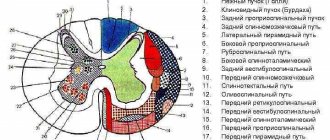
The spinal cord is made up of nerve tissue cells called neurons. They are concentrated closer to the center and form gray matter. According to rough estimates by scientists, the entire organ contains about 13 million cells, which is many times less than in the head section. The gray matter is located inside the white matter, and if you make a cross section, it will be shaped like a butterfly. This is especially clearly visible in the diagram.
Schematic cross-section of the spinal cord
This unique anatomy allows the spinal cord to be divided into several structures. It is arranged as follows:
- Front horns. They are distinguished by their rounded, wide shape and consist of neurons responsible for transmitting nerve impulses to the muscles. It is precisely because they perform such a task that they are called motor. The anterior roots of the spinal nerves begin in the anterior horns.
- Hind horns. They are distinguished by a long, narrow shape and consist of interneurons. They bear this name due to their ability to receive incoming signals from the sensory roots of the spinal nerves, otherwise they are called dorsal roots.
- Side horns. They are present only in the lower segments of the organ, and contain vegetative nuclei responsible for the dilation of the pupils, or the functioning of the sweat glands.
The physiological function of nerve endings is to transmit signals from the brain to the spinal cord, as well as deliver received impulses in the opposite direction. This ensures interconnection at all levels and areas of the nervous system. Nerve fibers are combined into bundles and are present along the entire length of the spinal cord.
Metamer and segmental structure
Each part of the spinal cord is a constituent element of a specific metamere of the body. Moreover, if there is a “piece” of the spinal cord that includes a section of gray matter with a pair of roots, then the metamer includes the spinal segment itself, muscle fiber (myotome), a section of the epidermis (dermatome), a bone component (scletorome), an internal organ (splanchiotome), controlled by this segment. In humans and higher representatives of the animal world, radicular metamerism is observed - the spinal cord is confined to certain parts of the body.
The skin areas of the body consisting of sensory fibers that approach the corresponding segment of the spinal cord are called dermatomes. They are strips of epidermis controlled by sensitive nerve endings. They are located throughout the body and sometimes overlap each other.
Visual representation of the connection between the skin and the spinal cord
Myotomes are muscle groups that receive motor fibers from certain areas of the brain. Thanks to the study and knowledge of their location, the process of damage and diagnosis of spinal cord lesions is greatly simplified. Damage to a certain segment of the spinal cord provokes sensory and motor disorders.
Connection between the spinal cord and muscle fiber
Segmental structure
The spinal cord is conventionally divided into five sections, although it is a single whole. The name of each directly depends on its location in the body. In total, a person may have 31-33 segments, which consist of:
- Cervical area - includes 8 segments.
- Thoracic region - 12 segments.
- Lumbar region – 5 segments.
- Sacral – 5 segments.
- Coccygeal – 1-3 segments.
This division allows us to examine the organ in more detail and simplify the process of diagnosing various pathologies.
White and gray matter
In cross-section, the symmetrical halves can be seen in detail and the anterior medial fissure and connective tissue septum can be seen. The part located inside is darker and is called gray matter (GM), it is located in a lighter substance - white matter (WM). Most of the SV is located in the lumbar region, the least is observed in the thoracic region. What are the main functions of gray matter:
- Transmission of pain impulses.
- Response to temperature changes.
- Closure of reflex arcs.
- Obtaining information from muscle tissue, tendons, ligaments.
- Formation of pathways.
What is the structure of white matter? It consists of myelinated, unmyelinated nerve fibers, blood vessels and a small amount of connective tissue. Its main task is to trigger simple reflexes and provide connections with skeletal muscles.
Spinal cord
Description
The spinal cord (medulla spinalis) is a part of the central nervous system located in the spinal canal.
At the top, the spinal cord passes into the brain stem, and at the bottom, gradually decreasing in diameter, it ends with the conus medullaris. In adults, the spinal cord is much shorter than the spinal canal, its length varies from 40 to 45 cm. The cervical thickening of the spinal cord is located at the level of the third cervical and first thoracic vertebra; The lumbosacral thickening is located at the level of the X-XII thoracic vertebra. A segment of the spinal cord corresponding to two pairs of roots (two anterior and two posterior) is called a segment. The anterior and dorsal roots emerging from the segments of the spinal cord unite into 31 pairs of spinal nerves
.
Along the spinal cord there are arteries supplying it with blood: the unpaired anterior spinal artery and the paired posterior spinal artery, which are formed by large radiculomedullary arteries. The superficial arteries of the spinal cord are interconnected by numerous anastomoses. Venous blood from the spinal cord flows through the superficial longitudinal veins and anastomoses between them along the radicular veins into the internal vertebral venous plexus.
The spinal cord is covered with a dense cover of the dura mater, the processes of which, extending from each intervertebral foramen, cover the root and the spinal ganglion. The space between the dura mater and the vertebrae (epidural space) is filled with venous plexus and fatty tissue. In addition to the dura mater, the spinal cord is also covered by the arachnoid and pia mater. Between the pia mater and the spinal cord is the subarachnoid space of the spinal cord, filled with cerebrospinal fluid.
Research methods
Myotatic reflexes are manifested by shortening of the muscle in response to its stretching when the tendon is struck with a neurological hammer. They differ in locality, and the topic of spinal cord damage is determined based on their condition. The study of superficial and deep sensitivity is important
.
When the segmental apparatus of the spinal cord is damaged, sensitivity in the corresponding dermatomes is impaired (dissociated or total anesthesia, hypoesthesia, paresthesia), and vegetative spinal reflexes change (viscero-motor, vegetative-vascular, urinary, etc.). Important information about the state of motor and sensory neurons of the spinal cord is obtained from electromyography
,
electroneuromyography
, which makes it possible to determine the speed of impulses along sensory and motor nerve fibers and to record evoked potentials of the spinal cord.
Using X-ray examination
damage to the spine and the contents of the spinal canal (the membranes of the spinal cord, blood vessels, etc.) are detected.
In addition to survey spondylography, if necessary, tomography
, which makes it possible to detail the structures of the vertebrae, the size of the spinal canal, detect calcification of the meninges, etc. The anatomical contours of the spine and the structures of the spinal canal of the spinal cord are well visualized using
computed tomography
,
magnetic resonance imaging
.
The level of block of the subarachnoid space can be determined using radioisotope (radionuclide) myelography
. Thermography is used in the diagnosis of various spinal cord lesions.
Functions
Functional anatomy implies that, being part of the central nervous system, the spinal cord performs a reflex and conductive function. In the first case, the body controls the implementation of the simplest actions at the level of reactions contained in the subconscious. A striking example is the initiation of a motor function by withdrawing the hand if the surface is too hot. The limb does this before the person himself understands what happened. The second task of the organ is to transmit nerve impulses to the head section of the central nervous system, along the ascending and descending pathways.
Briefly about the main functions of the spinal cord
Reflex function
This main function of the organ is a response to external irritation. For example, the appearance of a reflex cough due to foreign objects and particles entering the respiratory tract, removing the hand from cactus spines or a source of danger. The impulse enters the spinal canal through motor neurons, which also trigger muscle contraction. This process does not require the involvement of the brain, and the motor reaction occurs without its participation. That is, a person does not even think about his action, often does not realize it.
Children's innate reflexes are checked after birth. They usually include the ability to suck milk, breathe, and jerk their legs. During development, acquired reflexes also appear, which help doctors identify the correct functioning of the arch elements and individual segments of the spinal cord. The test is carried out during a neurological examination. The main emphasis is on the plantar reflex, knee and abdominal. They allow you to check how healthy a person is at one time or another.
Conductor function
Treatment of spinal cord myelitis
Another important function of the spinal cord is conduction. It ensures the transmission of impulses from the skin, mucosal surface, internal organ to the brain and in the opposite direction. The white matter acts as a “conductor”. It is this that carries information about incoming impulses from the outside. Thanks to this ability, a person can characterize any object that surrounds him.
Cognition of the world is carried out through the transfer of information after touch to the brain. It is thanks to this function that a person understands that an object is slippery, smooth, rough or soft. With loss of sensitivity, the patient ceases to understand what is in front of him when touching an object. In addition, the brain receives data about the position of the body in space, tension in muscle tissue or irritation of pain receptors.
Spinal roots
The connection of the spinal cord with the periphery is carried out through nerve fibers passing in the spinal roots, through which afferent impulses arrive to the spinal cord and efferent impulses pass from it to the periphery. On both sides of the spinal cord there are 31 pairs of anterior and posterior roots.
The functions of the spinal roots have been elucidated by cutting and irritation techniques and confirmed by abstraction of electrical potentials. The anterior spinal roots contain centrifugal, efferent fibers, and the posterior ones contain centripetal, afferent fibers. This fact is called the law of distribution of afferent and -efferent fibers in the spinal roots, or Magendie's law (named after the physiologist who first described the corresponding observations).
After unilateral transection of all anterior roots in a frog or any other animal, the reflex movements of the corresponding half of the body disappear, but its sensitivity is preserved. Transection of the posterior roots does not entail loss of the ability to move, but sensitivity in the areas of the body that were supplied by the corresponding roots disappears.
Effective proof of the functional role of the anterior and posterior roots was given by I. Müller, who cut the anterior roots of a frog on one side of the spinal cord and, on the other side, the posterior roots innervating the hind limbs. On the side of the body where the anterior spinal roots , the paw hung like a lowered whip, but irritation caused it to move other parts, in particular the opposite limb. On the other side, where the dorsal roots were cut, the paw made movements in response to irritation of other parts of the body, but did not react to irritation of itself due to a complete loss of sensitivity.
Subsequently, it was shown that in the anterior roots, in addition to the motor nerves of the skeletal muscles, there are also other efferent nerve fibers: vascular and secretory, as well as those going to the skeletal muscles. Their presence does not contradict Magendie’s law, since they are all efferent.
Paradoxical, at first glance, is the fact that irritation of the anterior roots is often accompanied by a sensation of pain. However, this fact does not contradict Magendie’s law, since it has been established that part of the fibers passing behind the roots wraps in the anterior ones and is directed to the spinal membranes, supplying them with sensory endings. They enter the spinal cord in the same way as other afferent nerves, through the dorsal roots. This can be verified by cutting several posterior roots and then irritating the corresponding anterior roots: pain, which is called recurrent sensitivity, is no longer observed.
The fibers that make up the anterior roots are axons of the motor cells of the anterior horns, as well as cells related to the autonomic nervous system located in the lateral horns of the thoracic and lumbar segments of the spinal cord. The fibers that form the dorsal roots are processes of bipolar cells of the intervertebral special ganglia.
The location of the neuron bodies from which the fibers passing in the spinal roots originate is established through experiments in which the roots are cut or limited damage to the gray matter of the spinal cord is performed, and then after a few days the degeneration of the nerve fibers is traced on histological sections.
Transection of the dorsal root below the spinal ganglion entails degeneration of fibers going to the periphery, while cutting above the node results in degeneration of fibers entering the spinal cord. In the area of the node itself, the nerve fibers do not degenerate, which indicates that here are the bodies of the nerve cells from which the fibers of the dorsal roots originate. The fibers of the anterior roots degenerate to the periphery from the site of transection at any level, as well as when the anterior or lateral horns are damaged. This shows that the latter contain the bodies of neurons, the processes of which run as part of the anterior roots.
The spinal roots contain nerve fibers of different thicknesses that have different conduction speeds.
The dorsal roots contain thick fibers belonging to the Aα group, which are afferent conductors coming from the nuclear bursa of the muscle spindles and Golgi bodies located in the tendons. Impulses passing through these fibers cause myotatic reflexes, which occur in response to muscle stretching. Fibers of medium thickness (5-12 microns), belonging to the Aβ and Aγ types, passing along the dorsal roots. come from tactile receptors and from muscle spindle receptors located to the periphery of the nuclear bag. Similar fibers come from the receptors of hollow internal organs (bladder, stomach, small and large intestines, rectum, etc.).
Afferent fibers Aβ and Aγ carry impulses from mechanoreceptors. After entering the spinal cord, these fibers enter the posterior columns, giving collaterals to intercalary (so-called commissural) neurons located in the gray matter of the superior and underlying segments of the spinal cord. Impulses arriving through a small number of afferent fibers of this group can cause excitation of a large number of spinal cord neurons. Thus, stimulation of a limited number of receptors, for example by pricking a finger, can cause a contraction of a large group of the mouse, leading to the flexion of an arm or leg. The thinnest fibers (2-5 microns in diameter) of the dorsal roots, belonging to the AΔ group, carry impulses from thermoreceptors and pain receptors. Impulses from the latter also enter the spinal cord via thin non-myelinated fibers belonging to group C.
The anterior roots also contain efferent nerve fibers of different types. Here are:
- thick fibers (on average 16 microns in diameter) of Tina Aα, carrying impulses to skeletal muscles;
- thin fibers (on average 8 µm in diameter) of type Aγ, innervating the contractile elements of the muscle spindle,
- preganglionic sympathetic fibers belonging to type B.
After transection of the dorsal roots, along with the disappearance of sensitivity, movement disorders are also observed. So, if you cut all the dorsal roots innervating the dog’s hind limbs on both sides of the spinal cord, while keeping the anterior roots intact, then the animal will lose the ability to move with these limbs for the first time after the operation. After some time, the movements of the hind legs, which have lost sensitivity, are restored, but are of an abnormal nature: the movements are jerky, sharp; the paws bend too much and also extend too much. Such movements are called atactic. They also occur in humans with diseases of the spinal cord accompanied by damage to the ascending tracts (spinal ataxia).
Movement coordination disorder occurs as a result of the cessation of the flow of afferent impulses to the brain, primarily from the receptors of the motor apparatus, i.e., from proprioceptors, as well as from exteroceptors of the skin. The lack of information about the state of the motor system at each given moment of movement leads to the fact that the brain loses the ability to control, evaluate the nature of movement and make corrections at all stages of the motor act. And although efferent impulses come from the brain to the muscles and cause their contractions, this process is not controlled or regulated, since there is no feedback, without which it is impossible to control motor acts and perform precise and smooth movements. This is why motor acts that require precise hand movements, such as playing the piano or writing, are disrupted after anesthesia, i.e., a decrease or disappearance of the sensitivity of the skin of the hand from cold, or after intradermal injection of cocaine, a poison that paralyzes the receptors. Loss of sensitivity also leads to a weakening of muscle tone.
What organs does the spinal cord control?
It is also important to understand which internal organs are connected to the spinal cord and may suffer if a particular area of the spine is damaged. Specific spinal segments control specific parts of the body by transmitting nerve impulses and transmitting responses along motor neurons. What each vertebra is responsible for can be clearly seen in the table.
| Back segment | Vertebra serial number | Controlled internal organs |
| Cervical | 3-5 | Diaphragm |
| Cervical | 6-8 | Articular tissue of the upper limbs |
| Chest | 1,2, 5-8 | Muscle tissue and epidermis of the hands, elbows and forearms |
| Chest | 2-12 | Muscles, skin of the body |
| Chest | 1-11 | Intercostal muscles |
| Chest | 1-5 | Heads, heart |
| Chest | 5-6 | Lower esophagus |
| Chest | 6-10 | Gastrointestinal tract |
| Lumbar | 1-2 | Prostate, groin area, adrenal glands, bladder, uterus. |
| Lumbar | 3-5 | Muscles and skin of the legs |
| Sacral | 1-2 | Muscle tissue and epidermis of the lower extremities |
| Sacral | 3-5 | External genitalia, reflex centers, erectile dysfunction and defecation |
Damage to the spinal cord in a specific section negatively affects the functioning of these internal organs. In some cases, dysfunction occurs before vertebral compression or displacement is detected.
Spine structure
Berezhkova Lyudmila Vasilievna
Neurologist, Chiropractor
April 24, 2021
Osteochondrosis can manifest itself with different symptoms. Patients visit many specialist doctors. They complain to the ophthalmologist about flashing “spots” before the eyes and decreased visual acuity, to the ENT doctor they tell about tinnitus, hearing loss, discomfort when swallowing and frequent choking, to the neurologist about headaches, dizziness and unsteadiness of gait, and to the psychotherapist about depression , restless sleep and forgetfulness. Drops in the eyes and ears, various medications do not help them. Because the main cause of ailments is osteochondrosis of the cervical spine.
The most well-known and common symptom of osteochondrosis is pain in the back, neck, lower back, shoulder and pelvic girdle. Acute low back pain is the most common cause of disability in people under 45 years of age. Between the ages of 45 and 65, back pain ranks third in frequency after heart and joint diseases (arthritis). It was found that 60 ~ 80% of the population experienced such pain at least once. Currently, this disease is as common as influenza and cardiovascular diseases, and is not inferior to them in terms of financial costs of treatment. Foreign scientists have calculated that low back pain syndrome ranks third (as the most expensive disease after heart disease and oncology), because it is associated with significant costs for diagnosis and treatment, operations, disability compensation and disability subsidies.
Spine structure
The structure of the human spine is determined by its functions: supporting, protective, shock-absorbing and motor. The spine is a curved vertical column that supports the head from above and rests on the pelvis and lower limbs from below. The human spine consists of 33-34 vertebrae, of which 24 are connected by intervertebral discs and are mobile. There are 7 cervical, 12 thoracic, 5 lumbar, 5 sacral and 4-5 coccygeal vertebrae.
Vertebrae are called (vertebrae) in Latin, and the science that studies the spine and its diseases is vertebrology. Sometimes in the diagnosis you can find the word vertebrogenic or vertebral, which means “derived from the spine.” In the cervical vertebrae, unlike others, there are special openings in the transverse processes that form a canal. The vertebral artery passes through the canal into the cranial cavity. It nourishes the brain, including areas responsible for coordination of movements, hearing, emotions, sleep, wakefulness and much more. This explains the many-sided medical histories of people with cervical osteochondrosis.
The spine as a whole is a flexible rod and support for the head, shoulder girdle and arms, thoracic and abdominal organs. It connects the upper part of the skeleton to the lower. The supporting function of the spine is due to a gradual increase in the size of the vertebrae from top to bottom from the cervical to the sacral region. The largest size is at the lumbar vertebrae. The underlying sacral vertebrae fuse into a single massive bone (sacrum). The coccyx is a remnant of the tail that disappeared in humans.
The protective function of the spine is to protect the spinal cord from damage. Due to the end of the spinal cord at the level of the second lumbar vertebra, the vertebral foramen in the lower vertebrae gradually narrows and completely disappears at the coccyx.
A characteristic feature of the spine that ensures its shock-absorbing function is its physiological curves. Between the bodies of all vertebrae, except the first and second cervical, there are intervertebral discs. Thanks to the discs, the spine is mobile, elastic and resilient, and can withstand significant loads. Simple extension of the spine causes pressure on the spinal discs of up to 90-123 kg. If extension is combined with lifting a load, then the force acting on the disc increases many times. It was experimentally found that a load of 100 kg reduces the height of the disk by 1.4 mm and increases its width by 0.75 mm. Painful changes in the condition of the disc lead to dysfunction of the spine. Staying in a horizontal position for several hours straightens the discs and lengthens the human spine by more than 2 cm. Due to the loss of elasticity of the disc, which occurs with age due to a decrease in its ability to bind water, a person’s height can sometimes decrease by more than 7 cm .
Ligamentous apparatus and muscles.
Ligaments (dense connective tissue structures) firmly connect the vertebrae, directing and holding their movements in different directions. The ligaments can withstand heavy loads and are so tensile that they do not tear during injury. Usually there is a tearing of a section of bone at the site of attachment of the ligaments. Numerous back muscles, along with ligaments, ensure reliable connection of the vertebrae and mobility of the spine.
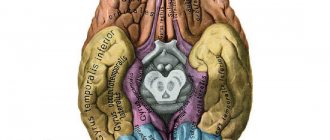
Anatomy of the spinal cord.
Protecting the spinal cord, the structures of the spine closely interact with it, its roots and nerves, ensuring the functioning of their corresponding internal organs and parts of the musculoskeletal system. The spinal cord lies in the spinal canal, located from the edge of the occipital foramen of the skull to the level of the first and second lumbar vertebrae, gradually thinning and ending in a cone. Below the spinal cord in the spinal canal there is a bundle of nerve roots extending from it, which is called the “cauda equina.”
The spinal cord is surrounded by three membranes: soft, arachnoid and hard. The pia mater directly covers the spinal cord. Between it and the arachnoid membrane there is a subarachnoid space in which the spinal cord and its roots lie freely, “floating” in the cerebrospinal fluid. The dura mater is adjacent to the vertebrae. Spinal nerves depart from the spinal cord: 8 pairs of cervical, 12 - thoracic, 5 - lumbar, 5 - sacral and 1 or 2 - coccygeal. Each spinal nerve exits through its own intervertebral foramen with two roots: the posterior (sensitive) and the anterior (motor), which are connected into one trunk. Each pair of spinal nerves is responsible for a specific part of the body, skin, muscles, bones, joints and internal organs. All learned automatic and reflex (involuntary) movements are controlled by the spinal cord.
Statics and biomechanics of a healthy spine.
Maintaining the correct position of adjacent vertebrae and the entire spinal column as a whole is called statics. Normal statics allow the spine to perform its functions of support and protection. The curves of the spine are held by the strength of muscles, ligaments and the shape of the vertebrae themselves. The S-shaped profile of the human spine is due to upright posture. The double curvature of the spinal column gives it strength, softening shocks and impacts during movements.
For most people, the line of gravity runs in front of the spine, so body weight does not increase all the curves, but straightens the lumbar lordosis. When standing, muscles and ligaments tense and increase pressure on the vertebral bodies. Excessive mobility of the vertebrae is dangerous for the spinal cord located in the spinal canal. The degree of mobility (dynamics) of the spine is determined by the movement of adjacent vertebrae and changes in the configuration of the entire spine and its position relative to other parts of the body.
Movements of the spine are possible along three axes: flexion and extension along the transverse axis; lateral tilts around the sagittal axis, rotation around the longitudinal axis. Rotation is maximum in the cervical and upper thoracic regions, and flexion and extension are maximum in the cervical and lumbar regions. Lateral bending with the greatest amplitude is possible in the lower thoracic spine. The movements involve the passive part of the spine (vertebrae, joints, ligaments and discs) and the active part (muscular apparatus).
Correct statics and dynamics ensure stately posture and good mobility of the spinal column, its flexibility. Good flexibility is a sign of the optimal state of all anatomical structures of the spine, and therefore its health.
Risk of organ damage
Due to the characteristic structure of the brain, it is connected to most systems in the body. The integrity of its structure is extremely important for the correct functioning of the musculoskeletal system and the health of internal organs. Any injury, regardless of severity, can lead to disability. Sprains, dislocations, disc damage, vertebral fractures with or without displacement can cause spinal shock and paralysis of the legs, and disrupt the normal functioning of the cords.
Severe injuries result in shock lasting from several hours to several months. In this case, the pathological condition is accompanied by a number of neurological symptoms. These include numbness, sensory disturbances, pelvic organ dysfunction, and inability to control the process of urination and bowel movements.
Treatment of minor spinal injuries is carried out on an outpatient basis, using medications, therapeutic exercises and massage. Severe injuries require surgical intervention, especially if compression of the spinal cord is detected. Cells are quickly damaged and die, so any delay can cost a person’s health. The recovery period after such an intervention is up to two years. Various physiotherapeutic procedures help with this, for example, reflexology, ergotherapy, electrophoresis, magnetic therapy, etc.
The spinal cord is a key element of the human central nervous system, which is connected in one way or another with almost all internal organs and human muscle tissue. The specific structure allows you to transmit impulses and signals, ensure full motor activity, and perform a number of other functions.