Spinal cord tumors (SCT) are pathological neoplasms of malignant and benign nature, localized in the spinal cord. The insidiousness of such pathologies is that they can develop for a long time without clinically manifesting themselves until the tumor seriously increases in size. Another problem is the fact that the symptoms of a spinal tumor can easily be confused with other neurological diseases.
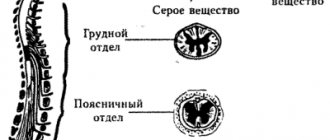
In a medical discipline such as neurology, the classification of tumors of the spinal cord and spine according to their anatomical location is represented by two main types.
- Intramedullary (determined in 18%-20% of cases) - they are formed from medulla cells and grow inside the spinal cord. Mostly found at the cervical and cervicothoracic levels.
- Extramedullary (found in 80-82% of cases) - located near the spinal cord, namely above or below its hard shell (extradural or intradural). Develop from nearby tissues surrounding the spinal cord.
In addition, the pathogenesis can be primary or secondary. Primary extracerebral and intracerebral dysfunctional changes in the genetic cellular apparatus initially originate and develop in the spine. In the structure of all neoplasms of the central nervous system, spinal neoplasia of the primary type accounts for 10% in terms of development frequency. The secondary type of newly formed tissues are daughter atypical formations in the spine, which are metastases of a malignant focus, emanating from a completely different organ or system. Such metastases can give rise to lung cancer (75% of cases), breast, prostate, thyroid cancer, and they penetrate mainly into the thoracic spine. A scientific presentation on spinal surgery contains information that for every 100 thousand population there are approximately 5 cases of metastatic oncopathologies of the spinal cord.
If we take the statistics for oncology as a whole, then the share of OCM of benign and malignant origin accounts for only 1%-2%, which is not so much. However, a serious attitude towards one’s own health will not be superfluous for any person, since cancer in an advanced stage is associated with a high risk of death. With benign tumors the situation is not so critical. Of course, if the clinical recommendations received from the doctor are followed unquestioningly and, importantly, in a timely manner.
Statistics indicate an annual increase in the incidence of ASM, albeit insignificant. Moreover, this diagnosis is given not only to adults of any gender, but even to infants. In infants, a similar picture often begins to develop even at the stages of intrauterine development, and here it is important not to miss the moment, to detect congenital pathology immediately after birth or at its earliest stage, taking appropriate therapeutic measures in a timely manner. A spinal tumor in a newborn will be removed or other treatment measures will be performed. A quick response from parents and doctors, well-chosen treatment tactics in the majority of cases help to achieve the baby’s recovery.
The consolation is that spinal cord oncology in very young children is very rare. In old age, it also does not occur very often. The main category of patients are people 20-50 years old, which is noteworthy: 85% are middle-aged. According to statistics, in the list of adult patients with benign pathologies, the female gender is slightly dominant, while there are more men with metastatic forms. The peak of such diseases in childhood occurs during school years (3 times more often than in preschool years), and boys are more susceptible to them.
Symptoms and diagnosis of tumors
Symptoms depend primarily on the etiology of ASM and the severity of pathogenesis. It is worth saying that at the initial stage, many serious morphological disorders occur latently or are not very pronounced; in other words, a person may not suspect for a long time that a dangerous process is being activated in his body. And this is most alarming, because the absence of symptoms hinders a timely visit to a specialist. Thus, treatment of spinal cord tumors is most effective at the earliest stages of tumor development.
The neoplasm is not a tissue section.
In ICD 10, malignant neoplasms of the spinal cord are assigned the code C72, and benign ones – D33.4. For both forms, the leading symptom is pain due to compression and damage to the most important structure of the central nervous system. The severity and nature of painful sensations are highly variable. The severity of pain is directly related to the class of abnormal cells, the location of the tumor, its size, etc. Thus, the pain can be either mild or moderate intensity or terribly unbearable. We list all the possible manifestations that are included in the symptomatic list:
- pain in a separate area of the back or neck, often radiating to other parts of the body (arms, legs, buttocks, hips, shoulders, ribs, etc.);
- muscle weakness at the level of the lesion and/or decreased tone and sensitivity of the limbs (in advanced cases, muscle atrophy);
- impairment of motor and support functions (reduced mobility in the back, inhibition and decreased accuracy of movements, coordination disorders, sudden falls when walking, etc.);
- various types of paresthesia, for example, numbness, a feeling of crawling, tingling and burning, which can be felt both at the site of the lesion and in the upper and lower extremities, head, chest, and abdomen;
- in advanced cases, paraplegia and paresis of any part of the body, but more often they affect the legs or arms;
- malfunction of the intestines or genitourinary system, expressed by retention or incontinence of urine and/or defecation, decreased potency, infertility;
- high blood and/or intracranial pressure, rise in body temperature, weight loss, seizures in combination with headache (not always).
Don't overlook even minor discomfort in any part of your back! For your peace of mind, do not put off going to the hospital until tomorrow, take into account the fact that the clinical picture of SM tumors may resemble the same osteochondrosis or intervertebral hernia. Relying on chance is risky; only differential diagnosis will help to recognize what disease is causing this or that symptom.
Intramedullary tumor of the spinal cord
Intramedullary (intracerebral) tumors in the general classification of OSM account for an average of 18%. They are predominantly represented by primary neoplasms from the structural components of the nervous tissue of the brain (gliomas). This variant of origin, the occurrence of which, according to some data, is approximately 95%, is called glial. Let's consider the most common neoplasms of the intramedullary series.
- Ependymoma (63%) is often a benign intradural tumor formed due to abnormal cell division of the ependymal epithelium of the central canal of the spinal cord. It is mostly located at the level of the cauda equina or in the neck, and has a clearly demarcated structure, which allows it to be successfully operated on (radically) with positive functional results for the patient. As reviews and clinical observations show, it is more often found in people over 30 years of age. Despite the predominance of benignity, after its total removal, consequences in the form of relapses or the appearance of metastases along the cerebrospinal fluid ducts can sometimes occur. Relapses occur in an average of 16% of cases.
- Astrocytoma (30%) is a benign (in 75% of cases) or cancerous (in 25%) tumor that develops from neuroglial cells (astrocytes). As a rule, this type of oncology is observed in the cervical segments in adults, and in the thoracic region in children. In children, astrocytoma occurs more often; they are usually detected before the age of 10. Intratumoral cysts are often found with this diagnosis, which grow slowly, but can reach impressive sizes. Its characteristic feature is expansive-destructive growth.
- Hemangioblastoma (7.5%) is a slowly growing non-malignant pathogenesis, which is a collection of thin-walled vascular formations. In 50% the lesion is thoracic, in 40% it is cervical. Men are 2 times more susceptible to this pathology than women. Predisposing age is 40-60 years. After high-quality surgical treatment, solitary hemangioblastoma almost never recurs. The situation is much more complicated with Hippel-Lindau disease, which in 25% of patients is combined with this type of tumor. With such a clinical picture, even complete removal of pathological tissue is not able to prevent the re-activation of a process of a similar nature in various parts of the central nervous system.
- Oligodendroglioma (3%) is a rare glial OSM of 2-3 degrees of malignancy, developing from mutated oligodendrocytes, that is, cells that form the myelin sheath of nerve fibers of the SM. It is detected with a high frequency in 30-45 years, the male sex is most vulnerable to it. After surgery, which is a necessary treatment measure, the pathological crisis often returns after 1-2 years.
Intramedullary type.
The first clinical signs of an intramedullary tumor in 70% are expressed by local pain, then it radiates to the lower or upper extremities. Over time, the atypical formation leads to severe neurological deficits: lack of mobility, muscle and joint weakness of the legs or arms, increased or decreased tactile sensations, numbness and other disorders associated with spinal cord damage. Without proper therapy, progression of neurological abnormalities and significant deterioration in a person’s quality of life are observed.
Important information! Today, surgical treatment is the generally accepted standard in the treatment of intramedullary tumors, which for the most part are potentially curable. Modern neuroimaging tools and surgical tactics make it possible to clearly plan the course of the operation and perform manipulations on the principle of the safest radical removal of such a neoplasm - while preserving areas of high functional significance. It is known that the earlier the intervention is implemented, the greater the patient’s chances of successful physical recovery and a significant increase in life expectancy.
Today, few clinics undertake to operate on an intramedullary tumor, considering it to be poorly located, and therefore offer only non-surgical treatment and standard decompression, which is often not justified. Although countries where modern high technologies in the field of neurosurgery are excellently developed, have an excellent command of productive, proven effective methods for removing even such a complex type of tumor.
Among the most successful countries in terms of productive treatment of vertebral oncopathologies of any type and severity, it is worth highlighting the Czech Republic. Why don't we talk about Germany or Israel? Of course, these two countries carry out high-tech operations at the highest level, but the cost is high.
Czech clinics are known everywhere for their specialization in this area, no less than German and Israeli medical institutions, but only in the Czech Republic the prices for surgical interventions for spinal tumors are 2 times lower. Moreover, clinical centers in the Czech Republic always include in this reasonable price (50% lower) full rehabilitation care after the removal procedure, and not just the services of a surgeon, as most medical institutions in Germany or Israel do.
Kinds
Thus, it is already clear that all neoplasms are divided into malignant and benign. Benign tumors often do not pose a serious threat to human life and health, only sometimes they can cause radicular syndrome, vertebral compression fractures and other complications. They are most common in young people, while the risk of developing cancer progressively increases with age.
A compression fracture is a destruction of the vertebral body with a decrease in its height along the entire perimeter, and more often in the posterior part with the formation of a defect that looks like a wedge.
It is malignant tumors that pose a particular danger, but they are formed in the spine initially, that is, they are primary, in less than 4% of cases. Almost always they are metastases, i.e. secondary tumors formed as a result of malignant cells entering the spine and surrounding tissues through the blood or lymph flow from tumors of other organs, usually the prostate gland, mammary glands, kidneys, thyroid gland , lungs, bladder.
Most often, metastases affect the lower thoracic and upper lumbar spine. Malignant cells that enter them and begin to multiply put pressure on nerve fibers, intervertebral discs, and the spinal cord; they can provoke a decrease in the density of the bone structures of the spine and cause instability of the vertebrae. This leads to the fact that patients may not only suffer from manifestations of radicular syndrome, but may also encounter signs of spinal cord damage, death of nervous tissue, vertebral compression fractures, and spondylolisthesis.
On the other hand, primary tumors of the spine, although rare, can also metastasize to other organs, including bones, liver, lungs, lymph nodes, brain, etc. Most often, the spine is affected by the following types of malignant tumors:
- Chondrosarcoma - forms from cartilage tissue on the vertebral arches, but quickly spreads to adjacent structures of the spine and ribs. Most often, chondrosarcomas are diagnosed in the lumbosacral region.
- Ewing's sarcoma is an oncological disease characteristic primarily of children, in which a malignant tumor forms in the vertebrae and surrounding soft tissues. This is a highly aggressive neoplasm, prone to metastasize in the shortest possible time to other parts of the skeleton, lymph nodes and lungs. Often its development and growth leads to the formation of a hematoma in the spine, which significantly worsens the patient’s condition and increases the risk of complications.
- Chondroma - is formed from the remnants of the notochord, i.e. embryonic cells from which the spine was formed during fetal development. Most often, chondroma affects the sacrococcygeal spine.
- Osteosarcoma is the most common malignant tumor of the spine. It is found in 50% of cases of confirmed spinal cancer. Osteosarcoma is formed from bone tissue and is prone to active metastasis.
- Reticulosarcoma is formed from lymphocytes and tends to cause acute neurological disorders, severe pain and provoke fractures of the affected vertebrae.
Malignant tumors extremely rarely form intramedullary, i.e., they affect the substance of the spinal cord. This could be, for example, a neuroectodermal tumor arising from neutral precursor cells. But due to the peculiarities of their location, such tumors are inoperable, i.e. they cannot be subjected to radical treatment. Their growth is suppressed by conservative means, so such neoplasms have an unfavorable prognosis.
The best prospects open up for extradural, i.e., those formed in the bone, and extramedullary intradural tumors, i.e., located within the spinal membranes. They can be removed surgically, which significantly increases the chances of a full recovery.
Benign tumors of the spine can be represented by:
- hemangioma;
- osteochondroma;
- osteoid osteoma;
- osteoblastoma;
- eosinophilic granuloma;
- aneurysmal bone cysts.
In addition, other benign tumors that are not related to the spine can form on the back. These can be atheromas or lipomas, i.e. tumors of subcutaneous fat.
Hemangioma
Spinal hemangioma is a vascular tumor, which in most cases is congenital and much less likely to form during life. It is one of the least dangerous neoplasms and is formed from endothelial cells in the thickness of the cancellous bone of the vertebra.
Hemangiomas account for 10-12.5% of all spinal tumors.
Most often, hemangiomas are found in the thoracic spine, somewhat less frequently in the lumbar spine, and extremely rarely in the cervical spine. As a rule, the tumor behaves calmly and does not require treatment, especially if its size does not exceed 1 cm, but it definitely needs dynamic monitoring. If during the examination it is discovered that the hemangioma has reached a large size, surgical intervention is recommended, as this is associated with the risk of a vertebral compression fracture. In general, hemangiomas have a positive prognosis, especially with timely surgery.
Osteochondroma
Osteochondroma is a nodular neoplasm that forms on the surface of bone tissue, with areas of calcified cartilaginous tissue. Its anterior surface is covered with smooth cartilage. Osteochondroma usually affects the spinous processes of the vertebrae and occurs in children around the age of 10 years. The tumor grows over 15-16 years and can be detected and removed at any stage of development. The prognosis is favorable.
Osteochondroma is the most common tumor of the spine. This is what is diagnosed in 36% of cases of detection of tumors in the spine.
Osteoid osteoma
Osteoid osteoma is a round tumor formed from osteoclasts and affecting bone tissue. Most often it is found in the lumbar spine and affects the articular processes of the vertebrae, involving the posterior structures of the vertebra, in particular the arch, in the pathological process. The tumor can be removed and has a favorable prognosis.
Osteoid osteoma is diagnosed in 10-12% of cases of detection of spinal tumors.
Osteoblastoma
Osteoblastoma or giant cell tumor is similar in many ways to osteoid osteoma, but is much larger in size. Such neoplasms are very rare and are diagnosed in only 1% of patients with spinal tumors, and most often this occurs in patients under 30 years of age, mostly men. Osteoblastoma is characterized by a sensation of the presence of a foreign body in the spine. Treatment is surgical, prognosis is favorable.
Eosinophilic granuloma
This type of benign tumor of the spine is an infiltrate, saturated with macrophages and affecting the bone tissue of the vertebrae. It is a rare phenomenon and has extremely mild symptoms. Initially, eosinophilic granuloma causes increased fatigue, limited movement in the affected area and mild pain during physical activity. But the formation of a tumor can also be completely asymptomatic, which is its main danger.
If persisted for a long time, eosinophilic granuloma of the spine can provoke spinal deformities, cause hypertonicity of the back muscles, and lead to severe pain and gait disturbances. Depending on the complexity of the situation, treatment can be conservative or surgical.
Aneurysmal bone cysts
Bone cysts are benign tumors filled with blood and located within the hard structures of the spine. They most often form in the cervical region at the back of the vertebrae or just inside the vertebral body. Aneurysmal bone cysts can act as a consequence of spinal injury. Treatment is surgical, the prognosis is favorable.
Comparative analysis
Taking into account the official data available to modern neurology on the prevalence of tumors in these two vital parts of the central nervous system, we can draw the following conclusion: the brain (brain) is approximately 4-5 times more likely to be affected by severe oncology than the spinal cord. Thus, among all oncopathies that are possible in the body, OGM is 6%-8%, and OSM is 2% or less. Traditionally, based on the location of brain tumors, the head is divided in the same way as spinal tumors - according to the anatomical relationship to the brain itself and its dura mater.
Most types of tumors of both components of the central nervous system coincide in biological type and are characterized by approximately similar morphological characteristics and stages. For example, such relatively common pathologies of the spinal cord and brain in terms of histogenetic parameters include astrocytomas, oligodendrogliomas, ependomas and hemangioblastomas, which we discussed in the previous chapter.
And even treatment involves the use of approximately identical principles: the surgical approach almost always comes first, it is aimed at total or subtotal removal of tumor tissue. Radiation therapy primarily acts as palliative care. It is worth noting that when diagnosed with a “brain tumor,” the disease proceeds in a more aggressive form, with the first signs (paroxysmal headache, nausea, periodic fainting, lethargy, etc.) appearing, as a rule, already in the initial stages. The prognosis of such diseases, both SM and GM, is directly related to the histological structure, localization and stage of the neoplasm.
Cancer intoxication
Having considered each point, we can derive general patterns. Firstly, it becomes difficult for a person to move. In the final stages there may be complete paralysis. Secondly, a person constantly experiences fatigue, even if he did not work and got enough sleep. It is worth paying attention to sweating: if it is cold (and sticky), then this fact indicates a cancerous disease. The number of urges to go to the toilet increases. An upset stomach is diagnosed: frequent diarrhea.
Extramedullary type
Such neoplasms, which in medicine are given the name “extramedullary,” are concentrated not inside the spinal component, but in close proximity to it. Simply put, they originate in the structures that surround the SC (developing from the meninges, nerve roots, fatty tissue and other tissues passing nearby).
This category of harmful process is the most common; it develops 4 times more often than true intracerebral pathogenesis, and, fortunately, is more represented by pathologies of benign origin. But this does not mean at all that a non-malignant disease cannot portend anything terrible. In the absence of the necessary treatment, it threatens severe disability due to compression of the spinal cord and its elements, up to the complete loss of the ability to move and self-care. Sudden death cannot be ruled out. This is not to mention the fact that due to such neoplasia, irreversible destruction of the bone and cartilaginous units of the spinal column often occurs. Therefore, both extra- and intramedullary tumors equally require timely diagnosis, as well as the rapid involvement of adequate methods of therapy.
MRI.
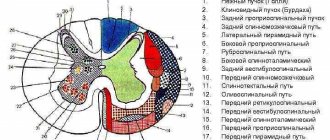
Extramedullary OSM can have extradural (31.5%) or intradural (68.5%) localization. The extramedullary-extradural type is distinguished by its large size and the predominance of malignant forms; in turn, the malignant focus progresses at a fairly intensive pace and is predominantly recognized as a secondary (metastatic) formation. The extramedullary-intradural type of pathology, which is also the most common, is characterized by a predominance of primary neuromas (40%) and meningiomas (25%).
- Meningioma (arachnoidendothelioma) is a benign tumor that grows slowly and gradually. Formed from cells of the arachnoid meninges. Diagnosed over the age of 50 years, and in predominant numbers in women (80%). With a high frequency it affects the spinal membrane in the thoracic region. Rarely, but can recur and produce multiple growths, causing transverse damage to the spinal column. Although the size of this neoplasia, which externally resembles a small dense node, rarely increases by more than 1.5 cm, such a tumor even a few millimeters in size can directly put pressure on the nerve structures, provoking a severe neurological clinical picture of symptoms.
- Neuroma (schwannoma) is a round-shaped benign OSM with clear boundaries and a dense structure, which develops as a result of metaplasia of lemmocytes (Schwann cells), namely auxiliary cells of the peripheral nerve fiber involved in the formation of the myelin sheath. Female patients are more likely to experience this disease; people of middle age and older have the greatest predisposition. At first, the disease proceeds latently, and later it is expressed by severe radicular pain, paresis and paralysis of the muscles in the area of innervation, loss of sensitivity according to the conduction type. The neck and thoracic region are common areas that neuromas affect.
Other extramedullary neoplasms with intradural concentration (angiomas, lipomas, metastases, etc.) are much less common.
Symptoms of spinal cord tumors
It is impossible to determine exactly what type of tumor there is and what its features are only on the basis of complaints, a routine examination or x-ray. To develop the correct algorithm for therapeutic actions to combat an existing tumor, neurologists and neurosurgeons use paraclinical methods, exclusively in combination, and not selectively taken. They are represented by numerous laboratory and instrumental research methods. Their purely complex combination will make it possible to bring clarity and objectivity to the clinical picture, make an accurate diagnosis and achieve a positive result in the treatment of the patient. But we’ll talk about diagnostics a little later; now we’ll provide guidance on the main clinical stages of spinal cord tumors.
We suggest that you familiarize yourself with the stages of development of extramedullary OSM, since they are the ones that lead in the frequency of development. So, pathogenesis is conventionally classified into the 1st, 2nd and 3rd stages, which may not always be clearly distinguishable, let’s consider them.
- The first stage is radicular. Its course lasts from several months to 3-5 years. A characteristic symptom for the initial form of the disease is the occurrence of pain in the area of innervation of certain nerve roots, as a result of their irritation by the tumor object. The pain syndrome is of a girdling or compressive nature. It is most pronounced with cervical lesions and pathology that occurs in the so-called cauda equina. The increase in painful sensations naturally occurs at night, which interferes with normal sleep in a lying position. This stage is often associated with diagnostic errors. When making a diagnosis, some incompetent doctors mistakenly make diagnoses such as cholecystitis, appendicitis, fibrinous pleurisy, cardiac disorders, radiculitis, osteochondrosis, etc.
- The second stage is Brown-Séquard syndrome. It includes a symptom complex characteristic of lesions of half the diameter of the spinal cord: spastic paresis on the side of neoplasia, loss of deep sensitivity (sense of body weight, pressure and vibration, muscle-articular disorders, etc.), disturbance of graphesthesia. On the opposite side of the body, there is a dullness of pain, temperature and, less often, tactile perceptions. This stage does not last long; it is replaced by the most critical phase.
- The third stage is paraplegic. It consists of a complete transverse lesion of the spinal cord and, as a result, paralysis of the upper or lower extremities occurs. Against the background of damage to the diameter, serious problems with the pelvic organs and paresis develop. The approximate duration of this phase is 2-3 years, but in some situations it lasts from 10 years or more. The prognosis for recovery, with the final stage in full swing, is disappointing; the patient’s chances of functional recovery are negligible.
Need to know! Total damage to the diameter, in addition to complete loss of limb mobility, is extremely dangerous, especially if the lesion is located in the cervical or thoracic area. This scenario of events can extremely disrupt the functions of the heart and lungs, up to a sudden fatal outcome due to their failure. Note that approximately 65%-70% of spinal neoplasias are related to the thoracic and cervical spine. Most extradural OSMs, including the most common ones, are completely resectable. And in the first two stages, their surgical excision inspires maximum hope for a complete cure of the disease.
Tumor near the spine: what is it?
Don’t look for photos on the Internet if you find some raised formation or compaction on your spine! You still cannot make a diagnosis on your own. All this is understandable, you are worried about your health and urgently want to find out what kind of pathology has appeared on your back, is it cancer? However, even an experienced doctor will not always be able to make a diagnosis right away, simply by examining or palpating the painful area. Visually recognizable tumors visible on the back are not always a terrible oncology, but even without a qualified examination there is no guarantee that it is not.
There are a great many variants of diseases that can be concentrated in one place or another along the spine. This may be a complicated degenerative-dystrophic pathogenesis, a non-malignant or cancerous tumor of the spinal system. Or some disease of completely different tissues, for example, subcutaneous fat (lipoma, atheroma, etc.).
For your own good, in order to find out the type, malignancy of the pathogenesis, and receive an effective treatment program from a specialist, you should immediately visit a medical facility and undergo the necessary comprehensive diagnostics. Delay in the presence of cancer can cost a person his life.
Benign formation
Benign spinal neoplasms, as a rule, increase in size slowly. In addition, they have distinct contours against the background of surrounding non-pathological structures, making it much easier to completely eliminate them surgically. Many people are interested in this point: does this pathology change its shape, can it become malignant over the years? In general, by their nature, such tumors are practically not prone to malignancy and the spread of metastases throughout the body, both to nearby tissues of the spinal system and to distant areas, that is, internal organs (lungs, gastrointestinal tract, liver, etc.) .
But this is not a reason to resign yourself to the disease! A benign tumor of the spinal cord can cause a lot of suffering, negatively affect the ability to work, make a person disabled and shorten years of life by an order of magnitude if it is not eliminated in time. And all this happens because even a non-aggressive formation “lives” and, although not at a rapid pace, grows, which has a strong compressive effect on the surrounding tissues, as well as on the spinal cord itself. Thus, the gradually growing tumor substance depresses the blood supply, significantly disrupts the morphology, and ultimately leads to atrophy of vital structures and a number of very serious consequences.
Causes
Spinal tumors may originate from the spinal cord, within the meninges covering the spinal cord (intradural), between the meninges and bones (extradural) of the spinal column, or they may be located elsewhere.
Most spinal tumors are located extradurally. These may be primary tumors that originate in the spine, or secondary tumors that are the result of cancer spreading (metastasis) from other organs (primarily the lungs, breasts, prostate, kidneys, or thyroid).
Any type of tumor can occur in the spine, including lymphoma, leukemia tumors, multiple myeloma, and others. A small percentage of spinal tumors occur within the location of the spinal cord nerves (most often, these are ependymomas and other gliomas).
The cause of primary tumors of the spinal cord and spine is unknown. Some tumors are associated with genetic defects. Tumors of the spine and spinal cord are much less common than brain tumors.
As the tumor grows, spinal cord tissue, spinal roots, spinal blood vessels and bone tissue are involved. Exposure to the tumor causes symptoms similar to other compression syndromes (spinal injuries). In addition, tissue ischemia occurs due to invasion of tumor cells or due to pressure on blood vessels.
Risk factors
Most of us are aware of some of the risk factors that are associated with cancer. Smoking, poor diet, chemical and radiation exposure, a family history of cancer such as breast or ovarian cancer and hyperinsolation are common risk factors for cancer. These types of cancer generally occur in various organs and metastasize to the spine only after long-term development in the primary site. The spine has a well-developed circulatory system, and tumor cells can metastasize to the spine from other organs hematogenously (through the bloodstream). Low back pain is not usually the first symptom of malignant cancer coming from another part of the body. And so, doctors evaluate a patient for the potential development of a primary cancer site, but not for the presence of cancer in a patient with low back pain. Regular breast examinations (mammograms), smear tests (to detect cervical cancer), chest x-rays (to detect lung cancer), stool occult blood tests (to detect bowel cancer).
Cervical spinal cord lesions
A tumor can occur in both the upper and lower cervical region. Insidious processes in this zone are especially difficult. With lesions of the cervical part of the spinal column, early radicular syndrome is observed, manifested by shooting pains in the back of the head. When the upper pole of the tumor is concentrated in the cranial cavity, and the lower pole is in the spinal canal, intracranial hypertension is observed. Cervical ASM provokes respiratory dysfunction (dyspnea) due to paralysis of the diaphragmatic zone of the thoracic region; tumors often cause damage to the glossopharyngeal, hypoglossal and vagus nerves with impaired swallowing, speech and respiratory functions. Moreover, common phenomena with a similar location of the disease are:
- flaccid paresis of the arms along with muscle wasting;
- radicular pain and numbness in the hands;
- motor failure of the upper limbs;
- weakness of the hands.
Cervical spine.
Pathologies located in the cervical region contribute to a decrease in visual and hearing acuity, problems with memory and concentration, and the occurrence of severe disorders of the vestibular system.
Diagnosis of spinal cord tumors and treatment principles
The principle of examination for suspected ACM, as indicated initially by signs and symptoms, is not limited to radiography alone; in some cases it does not have any particular informative value. Correct diagnosis involves a multi-complex examination of the body, including:
- assessment of medical history and visual palpation examination;
- conducting neurological tests;
- studying a number of laboratory tests (urine, blood);
- myelographic examination;
- CT and MRI (magnetic resonance imaging provides maximum information);
- spinal tap;
- histological biopsy.
We have listed the standard range of diagnostic measures, however, exactly what types of studies neurodiagnostics will be based on is decided solely by a specialist on an individual basis. As for treatment, the basic tactic for such a medical problem is surgical resection of the spinal tumor. In case of benign encapsulated OSM (meningioma, schwannoma, etc.), full-volume removal is safely performed without the use of radiation. Tumors such as gliomas cannot be completely removed, and therefore they are partially resected, and then radiotherapy is used.
Radiography.
If the lesion is secondary or located in a difficult-to-reach location, radiation therapy may be the primary treatment, but in some cases, radical removal followed by courses of radiotherapy may be undertaken. Chemotherapy is used when absolutely necessary and only in combination with radiation treatment, since its use alone for ACM is not successful.
How is hemangioma treated?
A hemangioma of the vertebral body, if it is small in size and does not manifest itself aggressively, is not touched, but simply observed, periodically doing an MRI. This disease is benign, so there is no strong cause for concern; a tumor up to 1 cm is not dangerous. Usually it does not cause problems for a person, and if there are no signs of osteoporosis and neurological symptoms, treatment is limited to a maximum of exercise therapy and physiotherapy. But increased parameters of an abnormal vascular bundle inside the bone, which happens in isolated cases, require special surgical intervention. And primarily due to the fact that a vertebra affected by a defective conglomerate becomes fragile from the inside and can break at any time.
Hemangioma
In order to regress the tumor substance, as well as to reduce the neurological signs of the tumor and strengthen the weak vertebra, very productive neurosurgical technology is successfully used today. It's called vertebroplasty. This is a minimally invasive modern tactic that does not require general anesthesia and wide incisions. The essence of the technology is the introduction of bone cement based on polymethyl methacrylate through a percutaneous puncture into the pathological formation. The medicinal mixture is first mixed, after which a polymerization reaction occurs, releasing heat. Then the resulting mass is immediately fed through the working needle. The patient is allowed to go home within 24 hours after the intervention.
Syringomyelic syndrome due to tumor
The clinical and pathomorphological syndrome, which is called syringomyelic, is a common consequence of spinal neoplasms. It is characterized by the formation of specific cavities in the spinal cord, which are filled with spinal fluid. The syndrome is expressed by loss of pain and temperature sensitivity in certain parts of the body, which causes frequent painless burns and traumatic injuries. It also includes amyotrophy, spastic paresis of the limbs, motor dysfunction, etc.
Regression of such a complication is possible only after eliminating the main cause due to which it, in fact, developed. In our case, in order to stabilize the cerebrospinal fluid circulation, and, therefore, overcome this type of functional disorder, we must first solve the main problem - to operate on the spinal tumor and drain the resulting cavities. Most operated patients quickly notice noticeable improvements. Strength and range of motion in the limbs increases, pain subsides, reflexes are restored, and the legs do not tighten after removing the main source - an abnormal growth in the spine.
Rehabilitation after removal of tumors
After surgery, patients require very careful rehabilitation care and constant monitoring by experienced doctors. Rehabilitation begins in a neurosurgical hospital, and after that the patient should continue recovery in a specialized medical institution (rehabilitation center, sanatorium). Such operations are considered interventions of increased complexity, therefore, after them, in order to avoid complications and achieve the maximum possible restoration of previously suppressed functions, the prescribed postoperative treatment regimen should be strictly followed. It includes therapeutic measures aimed at:
- normalization of microcirculation and metabolic processes;
- developing self-care and mobility skills;
- increased muscle mass and strength;
- correction of gait, coordination of movements, posture;
- prevention of contractures and muscle atrophy;
- prevention of infectious and other complications;
- normalization of the functioning of affected internal organs.
All these goals are achieved with the help of special drug therapy, the use of orthopedic devices (bandages, collars) during the rehabilitation period, therapeutic exercises, physiotherapeutic procedures, and training on specialized simulators. High-quality rehabilitation and compliance with all preventive measures will help you return to normal life in a short time, as well as reduce to an extreme minimum all the risks associated with the occurrence of relapses of the disease in the future.