An arachnoid cyst is a space-occupying formation located in the brain, predominantly filled with cerebrospinal fluid. The walls of the neoplasm are formed from the structures of the arachnoid (arachnoid) membrane or connective tissue. The cavities are localized in the area between the medulla and the arachnoid membrane. A typical location is in the area of the cerebrospinal fluid tanks, the posterior fossa of the skull, and the temporal lobes. More often detected in men and in children.
Arachnoid cyst of the PCF - what is it?
Arachnoid cyst of the posterior cranial fossa is a type of cerebrospinal fluid neoplasm of the brain. The peculiarity of the posterior cranial fossa cyst is that it develops into oncology less often than other types.
The danger of an arachnoid cyst is the increase in unpleasant neurological symptoms and a negative effect on the functions of the brain and sensory organs. There is a possibility of death from cyst rupture or its degeneration into oncology.
Diagnostics
A consultation with a pediatrician (for children), a neurologist, and an ophthalmologist is indicated. A blood test shows the presence or absence of infectious pathogens, signs of autoimmune diseases, the level of cholesterol and other structural components, and coagulation. The leading method of instrumental research is MRI in the brain area.
An additional CT scan is often performed. Neuroimaging allows you to accurately determine the location of the cystic cavity and determine the degree of influence on nearby areas of healthy tissue. Other methods of instrumental research:
- Radiography.
- Angiography.
- Ultrasound diagnostics.
- Neurosonography (prescribed for newborns).
- Electroencephalography.
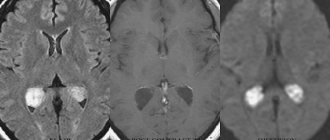
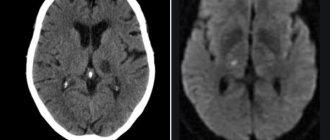
To accurately identify the communication channels between the cystic cavity and the cerebrospinal fluid circulation pathways, the following methods are used: CT myelocisternography and CT ventriculography with the introduction of a contrast agent. The picture of arachnoidal changes of a liquorocystic nature during MR and CT studies shows the presence of foci with the density of cerebrospinal fluid, which confirms the cystic, non-tumor nature of the formation.
During instrumental examination, expansion of the ventricles and extracerebral (isolated in the brain) spaces containing cerebrospinal fluid is more often observed. Electroencephalography is performed before and after surgery. In the second case, in order to determine the results of treatment and the correct selection of anticonvulsants.
An ophthalmological examination often reveals partial atrophy of the optic disc. If the arachnoid cyst is located in the PCF area, the results of echography (ultrasound examination) reveal changes characteristic of cystic formations of cerebellar localization. Differential diagnosis is carried out in relation to pathologies and anomalies of cerebellar development.
Factors influencing the development of arachnoid cysts
The disease can develop as a complication of previously suffered serious illnesses. In particular, the reasons for the development of a liquor cyst in the brain can be:
- Inflammatory diseases of the brain (meningitis, encephalitis);
- infectious diseases (chickenpox, influenza, measles, cytomegavirus, purulent inflammation in the head);
- suffered traumatic brain injuries;
- surgical operations on the skull;
- Marfan syndrome (genetically determined connective tissue pathology);
- congenital pathologies of nerve fibers.
Factors influencing the occurrence of cysts in the brain:
- diseases of the heart and blood vessels that impair blood circulation;
- cerebral hemorrhages;
- diabetes;
- repeated head injuries;
- hereditary predisposition;
- pathologies of intrauterine development of the fetus in the first trimester of pregnancy (with a congenital cyst);
- use of drugs, alcohol, poisoning;
- chronic fatigue syndrome;
- unfavorable living conditions and work that greatly weaken the body;
- radiation;
- poor living conditions of a pregnant woman (poor nutrition, stress, emotional overload, lack of rest);
- a pregnant woman taking medications, smoking, drinking alcohol;
- difficult childbirth with accompanying complications (craniocerebral injuries of the newborn).
The combination of these factors increases the negative impact. With a frozen cyst, any of them can cause tumor growth.
Preventive actions
Prevention of a primary cyst that forms in the mother’s womb includes several measures:
- The expectant mother needs to completely give up bad habits.
- Stop taking drugs that poison the body.
- Avoid taking certain groups of medications, since pregnancy is a contraindication for many of them.
- Adjust your diet by adding fresh vegetables and fruits, as well as foods that increase hemoglobin.
A pregnant woman needs to protect her baby from oxygen starvation. Regular walks in the fresh air provide invaluable assistance in this regard. It is also important to strictly follow all doctor’s prescriptions and undergo the prescribed examination on time.
Prevention of a secondary cyst looks a little different:
- Check your body regularly.
- If necessary, change your lifestyle by giving up bad habits and adding exercise.
- Monitor blood pressure levels.
- After traumatic brain injury, it is necessary to protect the body from excessive stress.
It is also important to control the amount of cholesterol in the blood, avoiding exceeding the permissible values.
Types of arachnoid cysts
A posterior fossa cyst (PCF) is a cavity with compacted walls with liquid or thick contents. Medicine considers two types of such neoplasms, dividing them based on their origin:
- Congenital – formed before the birth of a person, i.e. in utero;
- Acquired – occurs in a person after birth as a result of exposure to unfavorable factors.
The cyst can be simple (consist exclusively of cells of the arachnoid meninges) or complex (also include elements of other tissues).
In addition, all arachnoid cysts are divided into several types according to location.
Conventional arachnoid and retrocerebellar
A rentrocerebellar cyst is not located on the surface of the brain membrane, like a regular arachnoid cyst, but is located deep in the gray matter behind the cerebellum.
A common cyst is often localized in the gap between the arms of the arachnoid membrane, where liquor fluid can accumulate. A retrocerebellar neoplasm of this kind destroys the cells of the deep layers of the brain, growing in their place.
Temporal region cyst
A cyst in the temporal region can form on both the right and left. The symptoms in each of these cases will be slightly different. The reason is the focus of the lesion on different parts of the brain that control various functions in the body.
Posterior fossa cyst
The location in the posterior cranial fossa has its own characteristics. This is where the brain smoothly transitions into the spinal cord. Any neoplasm here can disrupt the connection during the transmission of nerve impulses from the brain to the spinal cord and vice versa.
In addition to the cranial nerves that conduct impulses to the sensory organs, large blood vessels lie here, and there is also the cerebellum, which is responsible for balance and coordination of movements.
This is a very dangerous type of disease, which can cause problems with breathing, heart function, and the ability to move normally. With rapid growth of the PCF cyst, a coma can occur with a fatal outcome.
Clinical manifestations
As mentioned above, subarachnoid and other types of brain cysts have practically no manifestations. They can only be detected by MRI or other diagnostic measures. Symptoms appear when the formations begin to increase in size.
Common signs include:
- cranialgia (headache in the bones of the skull);
- dizziness;
- noise in ears;
- feeling of heaviness and pulsation in the head;
- change in gait.
In some cases, hypertensive-hydrocephalic syndrome develops. It is a consequence of increased pressure inside the skull. Characterized by pain in the eyes, nausea, vomiting, and convulsions.
As the cyst grows, the severity of symptoms also increases. Headache, nausea and vomiting are becoming increasingly common. The patient experiences a feeling of fullness in the eyeballs. Subsequently, vision and hearing are impaired, double vision, speech problems, impaired coordination of movements, instability and partial or complete loss of sensitivity appear.
If the cyst compresses the pathways, paresis or even paralysis may develop. Muscle tone is greatly reduced, convulsions, fainting and hallucinations appear. Mental development slows down in young children.
The symptomatic picture largely depends on the location of the cyst:
- If the tumor is located in the temporal zone, the patient experiences disturbances in sensitivity and motor activity in the part of the body opposite to it. If it compresses surrounding tissues, symptoms develop like those of a stroke. The only difference is in the degree of their expression.
- A cyst located in the posterior cranial fossa manifests itself as breathing problems, disturbances in the functioning of the heart, partial or complete paralysis, and lack of coordination of movements. If the amount of cerebrospinal fluid continues to increase, the patient may fall into a coma. This greatly increases the risk of death.
- If the cyst puts pressure on the cerebellum, coordination is also impaired. The person cannot stand straight, staggers when walking, and makes involuntary movements. Dizziness, nausea, and noise in the head often appear. It's difficult to keep balance.
If at least one of the listed symptoms appears, you should immediately consult a doctor, since delay is fraught with deterioration of the condition and the development of complications.
Symptoms of the disease
Manifestations of the disease depend on the size of the cyst. If they are small, up to 2-3 cm in diameter, then the disease may be asymptomatic.
However, as the tumor grows, symptoms will appear in one way or another, the main ones being constant headaches and nausea with the urge to vomit.
Other manifestations of the disease:
- Loss of coordination of movements, unsteadiness of gait, difficulty maintaining balance;
- periodic paralysis of the limbs;
- changes in a person’s mental state;
- as the cyst grows, hallucinations occur;
- the appearance of seizures.
If a cerebrospinal fluid cyst has formed in a child during intrauterine development, then its first signs are restlessness, multiple regurgitations, difficulty moving arms and legs, lack of response to an adult’s voice, and bright objects.
The more fluid accumulates in the cavity, the worse the patient feels. If the volume of cerebrospinal fluid is up to 30 ml, the cyst is considered small; it manifests itself as a change in the local functions of the brain area. With a volume of 30 to 70 ml it is considered medium; symptoms increase and appear in a more distant period. If more than 70 ml of cerebrospinal fluid accumulates, it is a large cyst that puts pressure on the brain tissue and poses a danger to the patient’s life.
Features of tumor symptoms in men and women
The male part of the population is more often susceptible to arachnoiditis. According to world statistics, this disease occurs 4 times more often in men than in women. So far medicine has not been able to answer the question of why this happens.
In addition, affected men experience faster growth of the cyst, as well as a more frequent spread of growth to adjacent tissues. In women, the cyst causes fewer complications and remains in a dormant stage longer.
If a cyst is detected in a man of military age, he is given a deferment from military service and sent for additional examination and treatment. Further actions depend on their results.
People are not immediately drafted into the armed forces if intracranial hypertension is detected and symptoms of the disease appear. This also applies to single disorders associated with coordination, vision, hearing, etc.
Characteristics of the disease
A cerebrospinal fluid cyst is a formation in the brain tissue that is not a tumor, as confirmed by its morphological structure. It is a cavity isolated from other brain structures with liquid contents and dense walls. Clinically significant are large cystic formations that cause mechanical compression, compression, deformation of surrounding tissues - the brain matter, cerebrospinal fluid outflow tracts, elements of the circulatory system supplying the brain.
Arachnoid cysts are formations whose share, according to the results of intravital instrumental diagnostics, is equal to 1% of all volumetric processes occurring in the brain, which is less than that detected during autopsies (5 cases per 1000 patients). Normally, in adults and children, arachnoid cerebrospinal fluid cysts are absent in the brain tissue; if they are present, the degree of impact on health is determined by their size. Depending on the volume of the cystic cavity, the types of formations are distinguished:
- Small (volume does not exceed 30 ml).
- Medium (volume does not exceed 70 ml).
- Large (volume exceeds 70 ml).
Large formations are almost always associated with dislocation (displacement) of brain structures, which leads to neurological deficits. The suprassellar (growing deep into the skull) form is considered the most dangerous because it almost always causes occlusion or hydrocephalus. Treatment of hydrocephalic syndrome alone in this case is not enough due to significant compression of brain structures with the appearance of focal symptoms.
Diagnostics for identifying an arachnoid cyst
Detection of the disease should begin with a visit to a neurologist who will conduct proper examinations. It is important to differentiate a PCF cyst from diseases with similar neurological manifestations: various types of tumors, hemorrhage, hematoma, abscess and others.
MRI with contrast enhancement of blood vessels is rightfully considered the most accurate method for diagnosing tumors in the brain. It allows you to establish not only the presence of a neoplasm, but also its type and exact location. There is also a variation of this method – multislice computed tomography.
Ultrasound of the brain, EEG, and reencephalography are also used. For congenital arachnoid cysts, examination by a neurologist and psychiatrist is recommended, even if the child has no visible mental abnormalities. This is necessary to study the nature of neural connections affecting higher nervous activity.
Laboratory blood tests are performed for coagulation, cholesterol levels, autoimmune diseases, and neuroinfections.
Symptoms
Symptoms of an arachnoid cyst formed in the brain of newborns depend on the location, the degree of isolation from the spaces where the cerebrospinal fluid is located, and the distance from the cerebrospinal fluid circulation pathways. CSF cysts are often asymptomatic and are detected in childhood or young adulthood. Usually discovered accidentally during an instrumental diagnostic study prescribed for another reason.
Neurological symptoms appear as a result of the growth of a cystic formation, when a mass effect occurs - a tangible impact on nearby intracranial structures. Symptoms appear in 20% of patients with diagnosed pathology. More often, the manifestations of the disease are associated with hydrocephalic syndrome, which provokes the appearance of cerebral symptoms:
- Pain in the head area.
- Nausea, attacks of repeated vomiting.
- Ataxia, movement disorders.
- Hemiparesis, convulsive syndrome.
- Psycho-emotional disorders.
Less common are signs of focal damage to brain tissue, which is often associated with rupture of the cyst wall. To the main symptoms in infants, specific signs are added:
- Deformation of the skull bones.
- Dehiscence of cranial sutures.
- Protrusion of the fontanel.
- Lethargy, apathy, drowsiness.
- Lack of appetite.
- Signs of damage to the pyramidal tracts (pathological reflexes, paresis, paralysis).
- Delayed psycho-motor development.
A subarachnoid cyst formed in the brain in children occurs in 4 variants of the clinical picture. Depending on the characteristics of the manifestation of symptoms, the course of an arachnoid cyst that has arisen in the brain of a child can be:
- Lightning fast (2% of cases).
- Acute (6% of cases).
- Chronic (28% of cases).
- Remitting (2% of cases).
Symptoms may appear several weeks after birth or late in childhood and adulthood. The pathology is characterized by a pseudotumorous (resembling a tumor process) course and the absence of traces of inflammation in the meninges.
Treatment of cerebrospinal fluid cyst
If the tumor is small and there are no symptoms, the patient is monitored by a neurologist. At least once a year, a computed tomography scan of the brain is performed to monitor the further progression of the disease. The doctor may prescribe drugs that improve vascular function, diuretics, and analgesics.
However, more radical treatment in the form of surgery is often prescribed. Usually the indications for it are:
- Rapid increase in cyst size;
- severe increase in intracranial pressure;
- epileptic seizures;
- progression of the disease due to compression of brain tissue;
- ineffectiveness of previously prescribed medications.
Surgical intervention for PCF cyst can be performed in three ways:
- Shunting (pumping out the contents of the cyst into the abdominal cavity through a special shunt);
- endoscopy (pumping out cerebrospinal fluid from the cyst through a hole in the cranial bone, after which the empty cavity is connected to the cerebral ventricle or membrane);
- excision of the cyst (if there is a threat of cyst rupture or hemorrhage).
The third type of operation requires the longest recovery for the patient.
Possible consequences and complications
After a radical intervention with excision of the cyst, some neurological consequences may remain. This depends on the condition of the patient’s body, concomitant diseases, and compliance with medical recommendations.
The most severe consequences (disability, blindness, deafness, intractable headaches, rupture with effusion of cerebrospinal fluid, death) are possible in case of late detection of a large cyst.
An arachnoid cyst is a type of benign tumor. Practice shows that it can degenerate into cancer, but in fact there are not many such cases.
Prognosis and prevention for patients
The best prevention is a healthy lifestyle, strengthening the immune system, minimizing stress, and regular medical examinations for timely detection and treatment of diseases. This is especially true for expectant mothers.
But if a cyst is still detected, there is no need to panic. It is necessary to see a doctor and follow his recommendations, and get more rest.
In some patients, a recurrence of the cyst occurs after treatment. In case of relapse of the disease, regular monitoring of cholesterol levels, blood pressure, and treatment of existing diseases is necessary.
With timely treatment, however, the prognosis is good. Many patients recover completely and say goodbye to the cyst forever.