...a cyst is not a tumor...
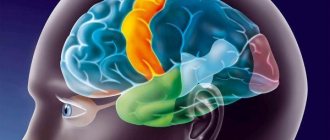
The most common type of brain cyst, occurring in 4% of the population, an arachnoid cyst is a cerebrospinal fluid (CSF)-filled sac located in the arachnoid membrane of the brain. At the site of the cyst, the tissue of the arachnoid membrane is divided into two layers with accumulation of fluid between them.
Get an MRI of the brain in St. Petersburg
It is important to remember that a cyst is not a tumor and in most cases is either asymptomatic or with minor manifestations and very rarely requires surgical intervention.
By origin, arachnoid cysts can be divided into:
- Primary, formed during intrauterine development;
- Secondary, arising as a result of injury or trauma, inflammatory processes occurring in the brain or bleeding.
According to the dynamics of development, there are cysts:
- Progressive. This type of cyst is characterized by a gradual increase in symptoms associated with the fact that the cyst, increasing in volume, increases its pressure on the brain.
- Frozen. These formations are stable and usually do not cause concern, often occur without symptoms, and some are detected only by chance during brain imaging caused by other reasons.
Symptoms of an arachnoid cyst
Depending on the location and size of the cyst, one or more symptoms may appear:
- Headache;
- Nausea and vomiting;
- Lethargy, including excessive fatigue or lack of energy;
- Seizures;
- Developmental delays;
- Hydrocephalus caused by disruption of the natural circulation of cerebrospinal fluid;
- Problems with the endocrine system, for example, early onset of puberty;
- Involuntary shaking of the head;
- Vision problems.
The larger the cyst, the more symptoms will appear, their frequency and severity will increase. With prolonged and strong compression, it can lead to irreversible changes in brain tissue. If excessive compression and rupture of the cyst membranes occurs, the patient may die.
"Scary" names
What is a cyst? A cyst (its other name is “cerebrospinal fluid cyst”) is a cavity filled with liquid, having a capsule that isolates it from other liquor-containing spaces.
with a retrocerebellar cyst consult a neurosurgeon . And although this phrase frightens and even makes parents panic, it must be said that with these words radiologists describe a variant of the norm. Most often, this is not a cyst at all (that is, not an isolated cavity filled with fluid), and it does not require surgical treatment.
Children under two years of age diagnosed with a retrocerebellar cyst should be shown to a neurosurgeon to avoid the development of hydrocephalus.
Another normal variant is a pineal gland cyst . Perhaps the most common incidental finding on MRI. Does not require surgical treatment.
An epidermoid or dermoid cyst is not a true cyst. It is filled not with liquid, but with skin appendages - follicles, sebaceous glands, hair, cartilage tissue, etc. In its structure, it is more similar to a tumor and requires the same treatment as for a tumor - removal.
A porencephalic cyst usually occurs in the place where part of the brain has died as a result of hypoxia or hemorrhage; this place is filled with fluid. In itself, such a cyst does not interfere with development and does not require mandatory surgical treatment.
Pseudocyst - looks like a cyst, but is not a cyst, a cavity that is not limited by anything, it has communication with other parts of the skull. Does not require surgical treatment.
a cyst of the transparent septum is a normal variant, but if it is large in size, it can lead to impaired circulation of the cerebrospinal fluid, which requires surgical treatment.
For children in whom the cerebrospinal fluid cyst rapidly enlarges, causes increased intracranial pressure, neurological symptoms or seizures, surgical treatment is indicated.
If your child has a photo taken and a cyst is found, don’t panic! Having received a description of the x-ray image, first of all, pay attention to the conclusion. If the report says: “There are no pathological abnormalities,” most likely you will not need any surgical intervention. Even if you see the word “cyst” somewhere, most likely the radiologist needed it to describe a normal condition. Just in case, check with him whether you need a consultation with a neurosurgeon.
Diagnosis and treatment of arachnoid cyst
Cysts that occur without any manifestations can only be detected by chance. In the case of neurological manifestations, the doctor first analyzes the patient’s complaints. However, the manifestations can only indicate that there are some malfunctions in the functioning of the brain, but do not allow us to classify the problem. Hematomas, brain tumors, cysts located inside the brain have the same symptoms. For a more accurate diagnosis, the doctor may prescribe electroencephalography, echoencephalography or rheoencephalography. The disadvantage of these methods is that they do not provide information about the exact location of the formation or its nature.
The main goal of any treatment for an arachnoid cyst is to drain fluid and reduce pressure on brain tissue.
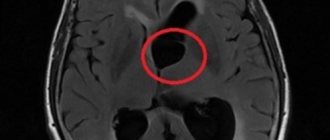
Today, the most accurate diagnostic method, which allows a high degree of accuracy to distinguish an arachnoid cyst from a tumor or hematoma, is computed tomography (CT) and magnetic resonance imaging (MRI).
This can be achieved by various methods including:
- Shunting. With this method, the surgeon installs a tube (shunt) into the cyst through which fluid is drained to other parts of the body (for example, the abdominal cavity), where it is absorbed by other tissues.
- Fenestration. In this case, holes are created in the patient's skull and the walls of the cyst to drain and ensure normal flow of cerebrospinal fluid.
- Needle aspiration and connection using holes of the inner part of the cyst with the subarachnoid space to drain fluid into it.
results
123 publications were found that matched the search criteria, with an abstract or full text of the study available for 72. The vast majority of works (57.79%) describe individual clinical cases and small series (less than 5 observations); 15 (21%) publications represent series of more than 5 observations, 8 (11%) publications contain information about 10 or more patients. The results of the analysis of literature data on the frequency of occurrence of individual clinical manifestations and the incidence of hydrocephalus in patients with symptomatic cysts are presented in Table. 1 . An overview of information on the prevalence of CAT, CPrP and CPV is presented in Table. 2 [1-11].
Table 1. Information on the frequency of occurrence of individual clinical manifestations and the incidence of hydrocephalus in patients with symptomatic midline cysts
| Number of publications: | 123 |
| included in the study | 72 |
| were not included in the study | 51 |
| Number of patients | 368 |
| Symptom, n (%): | |
| headache | 184 (50) |
| convulsive syndrome | 87 (23,6) |
| decreased intelligence/delayed psychomotor development | 74 (20,1) |
| mental disorders | 58 (15,8) |
| dizziness, nausea, vomiting | 40 (10,9) |
| disturbance of consciousness | 36 (9,8) |
| gait disturbances | 33 (9) |
| visual impairment | 31 (8,4) |
| papilledema | 17 (4,6) |
| cranial nerve dysfunction | 15 (4) |
| Hydrocephalus | 61 (16,6) |
Table 2. Main publications on the epidemiology of midline cerebrospinal fluid cysts
| Publication | Research method | Number of observations | Contingent | results |
| W. van Wagenen, 1934 [1] | Autopsy material, unfixed | 30 | Not specified | Checkpoint - ٦٠% |
| J. Schwidde, 1952 [2] | Autopsy material, fixation in 10% formaldehyde solution | 1032 | Newborns, children, adults up to 90 years old | PPP - ٢٠,٣٤% PV - ٢,٣٢% |
| J. Larroche et al. 1961 [3] | Autopsy material | No data | No data | PPP - ١٠٠٪ <٨,٥ months, ٨٢٪ full-term PV - ١٠٠٪ <٦ months, ٣٠٪ full-term |
| H. Schunk 1963 [4] | Photos of macropreparations | 307 | Patients who died from neurological diseases | PPP - ٦٠,٢% PPP ≥5 mm - ٠.٩% |
| J. Finke et al., 1968 [5] | Pneumoencephalography | 7711 | Not specified | PPP - ١,٧% |
| D. Babcock et al., 1981 [6] | Transcranial ultrasound | 102 | Newborns, children up to 9 months | PPP - ٤٢٪ (٦٢٪ - in premature babies, ٥٠٪ - in those born at term) |
| S. Nakano et al., ١٩٨١ [٧] | CT | 1050 | Newborns and children under 14 years of age with neurological diseases | PPP - ٢,٢٪ PPP+PV — ٣٪ PV - ٠,٤٪ |
| K. Akiyama et al., 1983 [8] | CT | 2722 | Adult patients | PPP - ٢.٦% |
| S. Mott et al., 1992 [9] | Transcranial ultrasound | 108 | Premature newborns (<35 weeks) | PPP - 100% average cavity width - 5 mm |
| J. Kwon et al., 1998 [10] | MRI | 113 | Psychiatric patients and control group | PPP >٥ mm - ٣٠,٤٪ patients with schizophrenia and ١٠,٣٪ control group patients |
| K. Wang et al., 2004 [11] | CT and MRI | 54000 | Not specified | Checkpoint - ٠.٠٤% |
Note. CP - septum pellucida cyst; CT - computed tomography; MRI - magnetic resonance imaging; PV - Verge's cavity; PPP - cavity of the transparent septum; Ultrasound - ultrasound examination.
MRI diagnostics for arachnoid cyst
Despite the fact that CT allows you to accurately determine the size and location of the cyst, MRI provides the most accurate and complete information about the formation. Typically, to diagnose an arachnoid cyst, an MRI scan is performed with the injection of contrast into the patient's bloodstream. At the same time, brain tumors tend to accumulate contrast, and cysts do not absorb it from the blood vessels, which is very clearly visible on MRI.
Also, MRI scanning allows you to distinguish a cyst from hemorrhages, hematomas, hygromas, abscesses and other diseases with similar symptoms. In addition, MRI makes it possible to identify a cyst even in cases where the patient does not yet have any symptoms, and the cyst itself measures only a few millimeters.
Get an MRI of the brain in St. Petersburg
1. Tumors of the transparent septum
Among brain tumors localized in the area of the septum pellucidum
, the most common are ganglioneuroma and central neurocytoma.
Ganglioneuroma
, or otherwise ganglioma, gangliocytoma is a benign tumor usually reaching small sizes - up to 4 cm. Ganglioneuroma is formed mainly by glial cells and does not have a capsule. Neoplasms tend to infiltrate into the spinal canal and posterior mediastinum.
Central neurocytoma
It is also a benign tumor and is quite rare - in only half a percent of cases of the total number of brain tumors. The usual location of neurocytoma is the lumen of the lateral ventricles closer to the area of the transparent septum. Central neurocytoma is characterized by slow growth and does not have a tendency to become malignant. This pathology affects both men and women in the age range from 15 to 40 years.
A must read! Help with treatment and hospitalization!
Second opinion for arachnoid cyst
Despite the fact that MRI diagnostics using a contrast agent provides the doctor with the necessary information, there is still a risk of error. It is associated primarily with the doctor’s lack of residual experience in interpreting MRI results and identifying cysts. Not a single patient is immune from such errors, and they happen both in large cities and in small towns. In this situation, the only way to eliminate an error or at least significantly reduce its likelihood is to obtain a second opinion from a highly qualified specialist
The National Teleradiological Network (NTRS) offers you the opportunity to receive consultations from the country's leading specialists in the field of MRI diagnostics, who have extensive experience in analyzing tomographic images of various diseases. To get a consultation, you just need to upload the scan results to our server and within a day you will receive an alternative opinion to the opinion of your doctor.
Perhaps it will be the same as the first medical opinion, perhaps it will differ from it, but the second opinion will definitely allow you to reduce the risk of misdiagnosis and incorrect treatment to almost zero.
The septum is normal
When the human embryo is at the developmental stage, this cavity is always present, but approximately six months after birth it closes. In approximately 15% of cases, the cavity of the septum pellucida normally remains.
This structure is not so well studied, however, experts conclude that non-closure of the cavity occurs due to the effect of alcohol on the fetus during pregnancy. An unfilled cavity, as a rule, does not have a significant clinical effect on the functioning of the body.
The cavity can be of varying sizes, in some cases it reaches 45 millimeters. Due to the complete isolation of this formation from the ventricles of the brain, in some cases the cavity is called the fifth ventricle, but this definition cannot be considered completely correct.
Types of brain cysts
The type of surgery to remove a brain cyst is selected based on the characteristics of the tumor. First of all, cysts are divided into primary and acquired. In the first case, we are talking about the death of brain tissue and problems with intrauterine development of the fetus. Acquired cysts appear due to bruises, inflammation, and bleeding.
Common types of brain cysts:
- retrocerebellar (occurs directly in the brain, namely in places where gray matter cells die);
- arachnoid (forms between the layers of the membranes of the brain filled with cerebrospinal fluid);
- subarachnoid (most often a congenital pathology, accompanied by pulsation in the cranium and painful muscle contraction);
- pineal (appears in the pineal gland and in the area where the hemispheres connect; has a direct effect on the endocrine system);
- pineal (diagnosed in the pineal gland, leads to impaired coordination of movement, vision, and metabolic processes).
There are cysts of the choroid plexuses of the brain, the pineal gland, located between the meninges, in the subcortical ganglia, cerebellum and even the visual thalamus.