The human brain is covered with three membranes: hard, arachnoid and soft. Between the arachnoid and soft membranes there is a cavity - the subarachnoid space. It contains 130 ml of liquor. This space can expand under the influence of negative factors, for example, a traumatic brain injury. In this free space, a cyst can form - a benign neoplasm containing fluid inside. In other words, it is a “light” tumor with water inside. It is 4 times more common in men.
Due to the formation of a cyst in the subarachnoid space, the structure of the arachnoid membrane changes, which forms the clinical picture. Arachnoid changes of a liquorocystic nature are a collective term denoting a number of organic damage to the arachnoid membrane and the space under it.
In medicine, such a diagnosis faces several problems:
- The symptoms that appear as a result of the pathology are nonspecific, that is, they are characteristic of many other diseases.
- The diagnosis itself is controversial: there is no evidence to support the existence of the diagnosis itself.
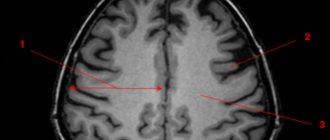
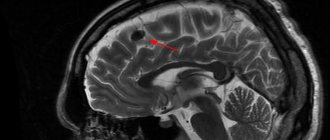
It is generally accepted that inflammation of the arachnoid membrane develops as a result of the formation of an arachnoid cyst underneath it. However, there are problems here too: magnetic resonance imaging does not show inflammation of the membrane, but only the neoplasm itself. Whether a cerebrospinal fluid cyst causes inflammation of the membrane is also a controversial issue.
In addition, the diagnosis of arachnoid changes of a liquorocystic nature is made after examining the brain on an MRI, when the images, except for the expansion of the subarachnoid space, do not reveal anything.
What is a cerebrospinal fluid cyst?
As mentioned above, a cerebrospinal fluid cyst is a benign tumor. It is hollow inside and filled with the same fluid that is found in the spine and protects the spinal cord (cerebrospinal fluid). It gets here through the tentorial notch (an opening in the hard shell). Hence the name.
The word “arachnoid” means that the cyst is located between the membrane of the same name and the duplication. Duplicature is the place where the shell is divided into 2 leaves. Liquid accumulates between them.
In most cases, the cyst is normally small in size. It all depends on the amount of liquid inside it. If it increases, the size of the tumor also changes. It swells and puts pressure on the brain, causing the development of unpleasant symptoms.
There is no specific localization location for the formation. However, most often it appears in the following places:
- posterior cranial fossa (PCF);
- pons-cerebellar angle;
- area above the Turkish sed;
- temporal region (pole right or left);
- Sylvian fissure.
Arachnoid changes, which are of a liquor cystic nature, usually develop in adults, and more often in men than in women. Doctors attribute this to the fact that males are more likely to experience traumatic brain injuries.
Classification of the disease
The pathology classification system is quite extensive. There are several large types of cysts and several subtypes.
Subarachnoid cyst. Is congenital. Discovered by accident. It manifests itself as a slight pulsation felt inside the skull, uncertainty in gait and convulsions. It can develop in any part of the brain, on the left, on the right, in the forehead.
Retrocerebellar. This is a cyst that is not located in the membranes, but directly in one of the parts of the brain. Appears after a stroke and with blood circulation problems. Characterized by serious consequences. Provokes tissue destruction and death.
Arachnoid cerebrospinal fluid cysts. This is a consequence of the development of atherosclerotic changes. Most often it appears in older people.
Primary tumor. Formation begins in the mother's womb. Another reason for its appearance is difficult childbirth or severe asphyxia.
Secondary cyst. It happens in both children and adults. Provoking factors are brain surgery, trauma, viral infections, radiation, age-related changes.
Progressive. The arachnoid cyst of the brain increases in size, affecting the quality of life. Requires immediate local treatment, including symptomatic treatment.
Frozen. The cyst is medium in size, does not grow, and has no manifestations. Even after its detection, there is no need for specific treatment. It is enough to visit a doctor from time to time.
The structure of the neoplasm is also a parameter for dividing into types. It can be simple and complex. In the first case, the cerebrospinal fluid cyst fully lives up to its name, since it is filled with cerebrospinal fluid. In the second case, there are various tissues inside it.
Cysts are also divided into types depending on location:
- in the posterior cranial fossa;
- in the spinal canal;
- in the left or right temporal lobe;
- in the frontal region.
The type of tumor directly affects the treatment plan.
Cysts in a child
Liqueur cysts also appear in children. Most often these are boys. In most cases, the tumor is congenital and is formed as a result of disturbances in intrauterine development. Sometimes it is acquired as a result of various injuries and infectious diseases.
It is noteworthy that a child can have both a primary and a secondary cyst. The first is typical for infants, while the second develops at an older age.
MR picture of arachnoid changes of a liquorocystic nature - what is it?
...cerebrospinal fluid cystic arachnoid changes are most often just an invention of radiologists...
Most often, the diagnosis of “arachnoid changes of a liquor cystic nature” is written when no cysts are reliably visible on MRI, but there is simply an uneven expansion of the subarachnoid space, that is, an increase in the amount of cerebrospinal fluid (CSF) between the brain and the skull bone. This expansion has nothing to do with arachnoid cysts, so liquorocystic arachnoid changes are most often just an invention of radiologists that do not have a reliable morphological basis. This term is absent in the scientific literature. You won’t find it on English-language sites, for example, on the world’s main radiology site, Radiopaedia.
Causes of arachnoid changes
There are many reasons for the development of cystic arachnoiditis. They vary depending on the form of the disease.
A congenital tumor is the result of several factors:
- unfavorable environmental conditions;
- smoking and drinking alcohol during pregnancy;
- intrauterine infections, in particular, toxoplasmosis, rubella, cytomaglovirus, herpes;
- work in hazardous production;
- poisoning of the body with narcotic substances;
- irradiation, overheating of the body in a bath/sauna, too hot baths, prolonged exposure to the sun.
The health condition worsens if Morphan syndrome, characterized by connective tissue pathologies, is added to the listed factors.
The reasons for the appearance of an acquired cyst are:
- various traumatic brain injuries;
- brain surgery;
- neuroinfections and inflammatory diseases, for example, meningoencephalitis;
- hemorrhage, as a result of which so-called bridges and cavities remain in the membrane or tissues of the brain.
These factors either cause the formation of a new cyst or provoke the growth and development of an old one.
Arachnoiditis - causes, signs, symptoms
First, let's deal with the concept of arachnoiditis. It is believed that various brain diseases suffered in childhood (traumatic brain injuries, microhemorrhages, latent meningitis) can cause chronic inflammation of the soft and arachnoid meninges - the so-called arachnoiditis.
- Arachnoiditis you are at risk
- 01
Traumatic brain injuries - 02
Microblood effusions - 03
Hidden meningitis
...if you have been diagnosed with arachnoiditis, you should always keep in mind that it does not carry much meaning
The diagnosis of “cerebral arachnoiditis” is made clinically by neurologists, based on complaints of headaches, fatigue, attacks of nausea and vomiting, memory impairment, etc. But the difficulty is that all these symptoms are nonspecific and can have different causes, and therefore in modern medicine the diagnosis of chronic arachnoiditis is very controversial. If only because we cannot reliably prove whether there is chronic inflammation of the meninges or not. We simply do not have any methods that could reliably detect this inflammation. Therefore, if you have been diagnosed with arachnoiditis, you should always keep in mind that it does not carry much meaning.
Why is an accurate diagnosis difficult to make?
- Symptoms are not specific
- Chronic inflammation is difficult to detect
- The nature of the arachnoid cyst is difficult to determine
On MRI of the brain, arachnoiditis most often does not have reliable signs, but sometimes it can lead to the formation of cysts located in the subarachnoid space, that is, between the brain and the skull bone. These are so-called arachnoid cysts. Arachnoid cysts have clear signs on MRI. But, unfortunately, most often we cannot say whether these cysts arose as a result of arachnoiditis, or whether they are congenital. Therefore, in modern neurology, the concepts of “arachnoiditis” and “arachnoid cyst” are different, and they should not be confused.
Clinical manifestations
As mentioned above, subarachnoid and other types of brain cysts have practically no manifestations. They can only be detected by MRI or other diagnostic measures. Symptoms appear when the formations begin to increase in size.
Common signs include:
- cranialgia (headache in the bones of the skull);
- dizziness;
- noise in ears;
- feeling of heaviness and pulsation in the head;
- change in gait.
In some cases, hypertensive-hydrocephalic syndrome develops. It is a consequence of increased pressure inside the skull. Characterized by pain in the eyes, nausea, vomiting, and convulsions.
As the cyst grows, the severity of symptoms also increases. Headache, nausea and vomiting are becoming increasingly common. The patient experiences a feeling of fullness in the eyeballs. Subsequently, vision and hearing are impaired, double vision, speech problems, impaired coordination of movements, instability and partial or complete loss of sensitivity appear.
If the cyst compresses the pathways, paresis or even paralysis may develop. Muscle tone is greatly reduced, convulsions, fainting and hallucinations appear. Mental development slows down in young children.
The symptomatic picture largely depends on the location of the cyst:
- If the tumor is located in the temporal zone, the patient experiences disturbances in sensitivity and motor activity in the part of the body opposite to it. If it compresses surrounding tissues, symptoms develop like those of a stroke. The only difference is in the degree of their expression.
- A cyst located in the posterior cranial fossa manifests itself as breathing problems, disturbances in the functioning of the heart, partial or complete paralysis, and lack of coordination of movements. If the amount of cerebrospinal fluid continues to increase, the patient may fall into a coma. This greatly increases the risk of death.
- If the cyst puts pressure on the cerebellum, coordination is also impaired. The person cannot stand straight, staggers when walking, and makes involuntary movements. Dizziness, nausea, and noise in the head often appear. It's difficult to keep balance.
If at least one of the listed symptoms appears, you should immediately consult a doctor, since delay is fraught with deterioration of the condition and the development of complications.
Symptoms
If the cyst does not reach pathological sizes and does not obstruct the outflow of cerebrospinal fluid, there will be no symptoms. The clinical picture appears when the neoplasm retains cerebrospinal fluid in the subarachnoid space, which leads to increased intracranial pressure. By irritating the arachnoid membrane, the cyst also causes the clinical picture of meningeal syndrome.
General cerebral signs of arachnoid changes:
- Headache of a bursting and aching nature. Worse in the morning. In response to this, vomiting occurs, bringing relief to the patient.
- Dizziness and nausea.
- Autonomic disorders: severe sweating, hand tremors, alternating diarrhea and constipation, heart pain, difficulty urinating, feeling of lack of air, feeling of a lump in the throat, aching pain in the abdomen.
- Violation of general sensitivity: numbness, chills or a crawling sensation occurs in different parts of the body.
- Diplopia is double vision. Sometimes there are episodes of visual impairment.
- Unsteadiness of walking, lack of coordination of movements and their accuracy.
Symptoms of irritation and inflammation of the arachnoid membrane include:
- Stiff neck. In patients, the muscles of the back of the head contract, causing the patient lying on his back to throw his head back. It will not be possible to bring the head to a normal position: due to a strong spasm, the torso will follow the head.
- Lockjaw. What is it - a spasm of the masticatory muscles.
- Bickel's sign - the arms are constantly bent at the elbow joints.
- Blanket symptom: The patient will involuntarily hold the blanket if he tries to pull it off.
- Photophobia, irritation to faint smells or tastes.
- Hyperesthesia is increased sensitivity to tactile contact. Touching the patient's skin causes discomfort, even pain.
With arachnoiditis, motor and sensory disorders such as mono- and hemiparesis may occur. This means that muscle strength is weakened in one limb or on one side of the body (left arm and leg together). Sensory disturbances include hallucinations. Their content and modality are determined by the proximity of the inflammatory focus to a certain area of the cortex (occipital - visual hallucinations, temporal - auditory hallucinations).
If the cyst reaches a large size and begins to compress the cortex, the patient experiences focal epileptic seizures. In severe cases, minor seizures develop into a generalized epileptic attack, aggravated by status epilepticus.
Arachnoid changes in liquorocystosis are characteristic and can imitate an intervertebral hernia. In this case, pain occurs along the spine, which radiates to the buttocks, thighs or arms. In these same places, sensitivity is weakened and paresthesia occurs.
Diagnostic methods
Due to the fact that arachnoid changes are usually asymptomatic, diagnosis is carried out only when one or more alarming signs appear.
Usually the doctor prescribes several procedures:
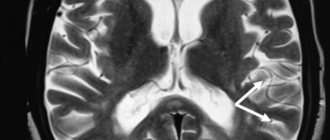
- MRI or CT. They allow you to prove the presence of a cyst, determine its size and location.
- Angiography using a contrast agent. Proves or disproves the presence of cancer cells.
- Blood test for infectious diseases.
- Cholesterol level analysis.
- Dopplerography. This is the study of the patency of blood vessels. Shows whether there are any disturbances in the blood circulation process.
- Electrocardiogram and ultrasound of the heart. Irregularities in the functioning of the heart can provoke deterioration of blood circulation in the brain.
Treatment of arachnoid cyst
If the tumor does not bother the patient and does not increase in size, there is no need for therapeutic measures. Otherwise, it needs to be treated. Usually 2 types of therapy are prescribed:
- medicinal;
- operational.
Treatment with medications can eliminate the cause of the formation of the cyst and its manifestations.
Several types of means are used:
If the tumor is a consequence of a stroke, medications will be needed to improve blood circulation in the brain.
For infectious diseases, you need to take antibacterial and antiviral drugs. With their help, you can get rid of the infection and prevent the growth of the tumor.
Progressive arachnoid cysts are treated with medications that help relieve neurological symptoms.
In some cases, the use of such funds is indicated:
- immunomodulators and immunostimulants;
- nootropics, vasotropics, antioxidants;
- drugs to eliminate adhesions.
The dosage and duration of drug therapy is determined by the attending physician. Self-medication is dangerous. It is possible not only not to be cured, but also to worsen the condition.
If medication is ineffective or ineffective at all, surgical intervention is indicated.
Indications for surgery are several conditions:
- persistent increase in intracranial pressure (does not decrease even after taking medications);
- development of mental disorders;
- frequent fainting;
- regular cramps;
- the cerebrospinal fluid cyst has increased in size;
- hemorrhage into the tumor cavity.
Urgent surgery is required if the cyst bursts. The leaking cerebrospinal fluid puts pressure on the brain tissue, which provokes an increase in pressure.
Surgical intervention is carried out using both trepanation and minimally invasive methods. The latter are used more often than others because they are characterized by a lower level of trauma, an almost complete absence of complications and quick recovery. Trepanation must have strong indications. The doctor must carefully weigh the pros and cons of performing it and assess the possible risks.
The most popular minimally invasive operations are fenestration, bypass surgery and microsurgery. Each method has its own characteristics:
During fenestration, the surgeon uses a special cutter to make a small hole in the skull. Through it, he removes the fluid accumulated inside the cyst. After creating several additional holes, it unites it either with the ventricles or with the subarachnoid space.
During shunting, cerebrospinal fluid from the tumor cavity moves into the chest or abdominal cavity. There it is quickly absorbed by the serous membrane. It is noteworthy that this method of surgical intervention is suitable for treating both adults and children. Most often, this operation is performed in cases where, due to the increasing amount of fluid, the cyst is constantly growing.
Microsurgery involves the removal of not only the tumor, but also the surrounding tissue.
Compared to the listed methods of surgical therapy, trepanation is more effective. But at the same time it is more traumatic.
If there is a need and the doctor allows, you can use traditional medicine methods. Infusions, elixirs and poisons will help improve the general condition of the body and speed up the recovery process.
There are a lot of recipes:
1. Combine 1 tbsp. instant yeast with 3 liters of warm water. Add 40 g of elecampane there. Mix thoroughly and place in a dark place for a day. Take 100 ml 4 times a day. The course of treatment is 21 days. The drug reduces inflammation and lowers intracranial pressure.
2. To eliminate headaches, mix 100 g of hemlock seeds or stems and 500 ml of olive oil. Infuse in a place protected from sunlight for 3 weeks. Then strain and use as nasal drops. Use 2 drops three times a day.
Preventive actions
Prevention of a primary cyst that forms in the mother’s womb includes several measures:
- The expectant mother needs to completely give up bad habits.
- Stop taking drugs that poison the body.
- Avoid taking certain groups of medications, since pregnancy is a contraindication for many of them.
- Adjust your diet by adding fresh vegetables and fruits, as well as foods that increase hemoglobin.
A pregnant woman needs to protect her baby from oxygen starvation. Regular walks in the fresh air provide invaluable assistance in this regard. It is also important to strictly follow all doctor’s prescriptions and undergo the prescribed examination on time.
Prevention of a secondary cyst looks a little different:
- Check your body regularly.
- If necessary, change your lifestyle by giving up bad habits and adding exercise.
- Monitor blood pressure levels.
- After traumatic brain injury, it is necessary to protect the body from excessive stress.
It is also important to control the amount of cholesterol in the blood, avoiding exceeding the permissible values.
Why is the disease dangerous?
A cerebrospinal fluid cyst, if not properly treated, can become a dangerous disease with serious complications and tragic consequences. It entails disability, and in isolated cases even death.
With timely assistance, the prognosis is more than favorable. The risk of worsening the condition is reduced. Otherwise, a number of conditions may develop:
- Neurological disorders. These include disturbances in motor activity, loss of sensitivity, and disruptions in the functioning of the nervous system.
- Epilepsy, frequent convulsions, involuntary movements of arms and legs, loss of consciousness.
Strict adherence to all doctor’s prescriptions will help prevent their development.
Arachnoid cysts do not pose a serious danger for the time being. They do not manifest themselves in any symptoms and are detected only during a routine examination. But sometimes, due to an increase in the amount of fluid, they begin to grow. In such situations, the person’s condition noticeably worsens and requires medical intervention.
These are relatively common benign and asymptomatic brain lesions. They are usually located in the subarachnoid space and contain cerebrospinal fluid. Richard Bright first described the arachnoid cyst in 1831.
Epidemiology
Arachnoid cysts account for about 1% of all intracranial formations. Although the vast majority of them are sporadic, they are most often observed in mucopolysaccharidoses. In a retrospective cohort study of 48,417 patients who underwent MRI, arachnoid cysts were identified in 661 patients (1.4%).
Clinical picture
Most arachnoid cysts are small and asymptomatic. Approximately 5% of patients have symptoms, and these are usually the result of a gradual increase in cyst size, leading to mass effect. And this leads to either direct neurological dysfunction or distortion of the normal cerebrospinal fluid pathways, which can lead to obstructive hydrocephalus. Arachnoid cysts are thought to arise from congenital clefting of the arachnoid layer with accumulation of cerebrospinal fluid in this space. The cyst wall consists of flattened arachnoid cells forming a thin translucent membrane. There is no solid component and no epithelial lining.
Radiological features
Arachnoid cysts can occur anywhere in the central nervous system, most often (50-60%) in the middle cranial fossa, where they invaginate and widen the Sylvian fissure. At this point they can be divided into three types depending on their size (Galassi Classification):
Classification
- type I
- small;
– limited to the anterior part of the middle cranial fossa, below the sphenoid crest;
– free communication with the subarachnoid space;
- type II
– length along the Sylvian gap;
– displacement of the temporal lobe;
– slow communication with the subarachnoid space;
- type III
– big
– fills the entire middle cranial fossa;
– displacement of not only the temporal lobe, but also the frontal and parietal lobes;
– often leads to a shift in the midline;
– weak connection with the subarachnoid space;
On CT: Arachnoid cysts are very well circumscribed, with an inconspicuous wall and displace adjacent structures. When large, they can have a remodeling effect on the bone over time. CT cisternography (injection of contrast into the subarachnoid space) demonstrates the communication of the cyst with the subarachnoid space. Because this communication occurs slowly, the cyst often fills later and the contrast can be seen to merge with it, highlighting its dependent part.
On MRI : Because arachnoid cysts are filled with cerebrospinal fluid, they have similar signal characteristics including FLAIR and DWI sequences. This makes it possible to distinguish them, for example, from epidermoid cysts. Because their wall is so thin, it can only be seen occasionally, and the displacement of surrounding structures suggests their presence. Phase contrast imaging can also be used to not only determine whether a cyst communicates with the subarachnoid space, but also to determine the location of this communication. Magnetic resonance cisternography: High-resolution sequences such as CISS and FIESTA help delineate the cyst wall and adjacent anatomical structures.